HealthManagement, Volume 5 / Issue 2 / 2010
Author:
Benjamin Hughes,
Researcher,
ESADE Business School
The internet’s impact on healthcare is ever more evident, with over 80% of US citizens searching online for health matters, and 33% of EU citizens using internet health sources every three months. Medicine 2.0 partly drives this increasing use, providing new sources of information and new access models for various healthcare stakeholders. The simplest interpretation of Medicine 2.0, or the closely related term Health 2.0, is the use of Web 2.0 for Medicine and Health.
How Web 2.0 is Applied to Health
Web 2.0 denotes a series of highly participative tools such as wikis, social networks or blogs that allow individuals to contribute to or participate in online health conversations. These conversations provide immense opportunities to improve healthcare delivery and efficiency, in a variety of contexts, such as by engaging users in creating encyclopaedic medical resources, improving medical and public health education, or enhancing clinical collaboration.
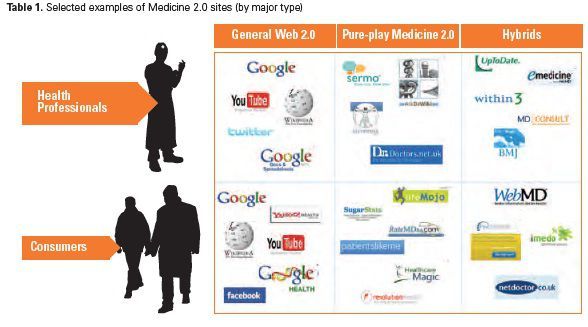
The concept Web 2.0 emerged at the end of the dotcom boom, as observers noted that certain types of websites thrived though the bust. These sites had in common a highly participative nature, the most successful of which emerging a few years later as household names with millions of users (e.g., Facebook or Wikipedia). The underlying approaches have been translated into the health domain, where Web 2.0’s application can be broadly categorised into three types. Firstly, resources vary by the key using stakeholder, with a clear distinction between those that target health professionals or patients. Secondly, sites vary by relative focus on health related subjects, with multi-purpose Web 2.0 tools serving as a platform for health matters amongst other topics. Finally, amongst sites dedicated to health matters, the use of Web 2.0 tools varies, differing from pure-play Medicine 2.0 sites, to hybrid offerings based on the supplementing of traditional health media with Web 2.0 features.
Household Web 2.0 Names and Health
In the application of multi-purpose or general Web 2.0 sites to healthcare, Wikipedia stands out above other sites. Wikipedia’s millions of user-generated articles has documented a significant body of medical knowledge, encapsulating articles on thousands of diseases, disorders, drugs and symptoms. With its high indexing in Google and most internet user’s familiarity with the site, it is not surprising that many patients use it as source of medical knowledge, often bringing Wikipedia printouts to consultations with doctors. Perhaps more surprising is its extensive use by doctors, and according to a survey of 1,900 physicians by Manhattan Research, nearly half of doctors going online for professional purposes use Wikipedia as a source of medical information. Other research based in the UK has shown even more extensive use amongst junior doctors, where up to 70% may consult Wikipedia in any given week. While doctors use it more for background medical information, rather than critical patient treatment decisions such as drug dosage, it still represents on of the most commonly referenced medical fact base due to its accessibility and breadth of topics. While Wikipedia is the most obvious example of a general Web 2.0 use in health, many others play a significant role. For example, YouTube contains 285,564 health education videos with sometimes huge audiences, such as the WHO’s H1N1 educational videos that was viewed up to 30,000 times a day.
Pure-Play Medicine 2.0
Given the success of general Web 2.0 tools and their clear applications for health, it is not surprising that the concept has been used to develop pure-play Medicine 2.0 resources focusing exclusively on health matters. High profile examples include revolutionhealth.com and PatientsLikeMe.com (patient communities), Sermo.com (a physician social network), or RateMD.com (a physician rating site). Most have more than 40,000 hits per day. PatientsLikeMe.com allows patients with serious diseases to share information, including ALS, multiple sclerosis, OCD, and Parkinson’s. Sermo.com is the largest physician social network, where both medical cases and practice matters such as hiring support staff are discussed. While the success of these sites mean they have started to incorporate content from more traditional sources (e.g., Sermo is now looking to link to Nature’s journals), in their conception they were positioned as pure Medicine 2.0 sites, relying purely on user-generated medical content to engage readers.
Traditional Medical Media Fights Back
Finally, traditional medical institutions are levering Web 2.0 to develop hybrid offerings through their traditional media channels. The comprehensive health resource WebMD is principally driven by traditional media content, but nonetheless incorporates active blogging or other Web 2.0 features in specific areas, such its eMedicine space that claims 10,000 physicians as user-contributors of content. Other hybrid examples include the British Medical Journals online presence, with traditional journal content now offered alongside blogs, or the launch of its doc2doc social networking accompaniment since 2008. Overall, there are numerous Medicine 2.0 sites and resources across professional specialty areas or patient condition types. Though some sites cross these boundaries, the types ‘General Web 2.0’, ‘Pure-play Medicine 2.0’ and ‘Hybrids’ largely describe broad applications of Web 2.0 to the health domain.
An Inseparable But Perilous Combination: Medicine 2.0 vs. Health 2.0
Which of the Aforementioned Case Examples are Medicine 2.0 and
Health 2.0?
Medicine 2.0 usually refers to the science of medicine and the practice of treating or curing patients, and Health 2.0 is focused on the business of health in general including the delivery, the quality, the safety and the cost or efficiency of the people, a practice or facility. The two concepts are intertwined, and if anything, Medicine 2.0 is the broader concept and umbrella term which includes consumer-directed ‘medicine’ or Health 2.0. Within any Medicine 2.0 conversation you will find stakeholders pursuing the goals of both concepts, and all have numerous visitors focused on simply finding the best treatment for a condition. However, many of these communities (such as Wikipedia, PatientsLikeMe or Sermo to name a few), have fulltime staff, revenue generation strategies via a mix of channels, and clear policies to promote information quality and safety. These revenue models may encompass donations, leverage of Google advertising, fees for advanced features, or partnerships that might affect the type of information presented and the way it is used. For instance, PatientsLikeMe is very upfront about that the fact that it sells its datasets onto to pharmaceutical companies for revenue.
Herein lies the most cited concern with Medicine 2.0, that user generated content is prone to be either inaccurate, misleading or manipulated, and that privacy and ownership of the generated information is not fully ensured. Anyone can edit Web 2.0 topics allowing the non-medically trained to dispense medical advice. In several instances, pharmaceutical companies modified Wikipedia entries that mentioned adverse effects associated with their drugs. In 2007, a claim that the psychiatric medication Seroquel made teenagers ‘more likely to think about harming or killing themselves’ was deleted from the Wikipedia entry by a computer registered to AstraZeneca, the drug’s manufacturer. While Wikipedia’s content has been shown to be as accurate as other encyclopaedic resources, such risk via omission remains a concern. A study from The Annals of Pharmacotherapy compared drug information from Wikipedia with the Medscape Drug Reference, and found that Wikipedia could sometimes omit important information such as drug side effects.
A Balanced Perspective of the Risks
This said, researchers have noted that these risks are potentially overblown. The risk of information inaccuracy is countered with three important effects during Medicine 2.0’s use, the encouragement of users to access any information at all, guidance of users to appropriate information through the process of Apomediation, and the purpose for which users seek and use the information found. Firstly, the usability of Medicine 2.0 sources, the underlying factor of their success, increases the chances that both medical professionals and patients seek out a minimum amount of information. For instance, while doctors should ideally be using best in class evidence based resources such as Pubmed, the article based structure of data supplied may require a significant search investment that is not realistic given a doctor’s specific time constraints. Secondly, Web 2.0 communities sift through volumes of information beyond the capability of the individual, impacting search engines page rank via the links they create, ranking individual information pieces, providing personal recommendations in communities, and rapidly correct wiki-based entries. This process, known as Apomediation, uses collective wisdom to filter for information quality and directs information seekers to higher quality content. Finally, it should be noted that users adapt their search and use of information found depending on their information need. For instance, Web 2.0 sources are commonly used for background information seeking, and when used for critical medical decisions, as an initial structuring device for deeper information searches. The linked nature of these websites means that users will usually incorporate multiple information sources in their decision making process.
In addition, privacy concerns may also be overblown. Surveys indicate privacy is a hot issue for healthy people; this isn't always the case for very ill patients. PatientsLikeMe encourages people to use an alias, however, many people freely self-identify themselves by adding information like photos or indicate their real names. This is true for many social networking sites, where users often provide significant information could be used in adverse ways in the future (think of pictures of people drunk at parties on Facebook). The reality is that most users are aware of these risks, but just as in real life conversations, users individually decide on the trade-off of revealing information about themselves given the increased returns this may bring. Overall, most Web 2.0 sites have become clearer about how a person’s information is used, but any organisation hosting Medicine 2.0 conversations must remain vigilant about privacy concerns.
Overall, while it is tempting to prescribe controls on such online health information to eliminate the risk completely, efforts to assess the Quality of Health Information for Consumers in general have had limited success. Use of Medicine 2.0 ultimately devolves responsibility to the individual, and user awareness of its risks and good practices, such as assessing quality and using secondary sources, remains critical.
Using Medicine 2.0, Externally and Internally, for
Effective Healthcare IT
For the healthcare IT manager, two main opportunities present themselves. Firstly, Medicine 2.0 enables improved external collaboration, either with patients, through shared clinical knowledge management, or with specific external organizations. Secondly, Web 2.0 may be applied to internal processes, to create new sources of information or improve collaboration.
Working Externally with Medicine 2.0
An obvious use of Medicine 2.0 is to engage patients, an approach that is gaining significant momentum with hundreds of US hospitals now using YouTube and Twitter for patient communication. However, this represents a small percentage of all hospitals despite the competitive nature of the US for attracting patients. Moreover, according to research at the RUNMC, Swedish, Dutch and English hospitals lead the use of social networking methods and media (Twitter, Facebook, YouTube, blogs), but in no more than around 10 percent of all hospitals in these countries.
Similarly, another clear external opportunity is promoting public Medicine 2.0 tools as knowledge assets for clinical staff. The reality is that such resources are already used by a significant proportion of medical professionals. Rather than passive acceptance of this, healthcare IT managers can establish policies that can ensure consistent use across the clinical staff. This involves ensuring access, creating awareness of the available resources, and disseminating guidelines for appropriate use. Access in itself is not obvious; research by the MLA indicates the majority hospitals have some form of network blockage due to the perception that Web 2.0 sites are a frivolous waste of bandwidth or a security risk. Appropriate guidelines are also key, given the implied devolution of responsibility to individual users for the determining information quality and appropriate use of information for medical decision making. Guidelines for overall internet use they are common (e.g., see http://www.mlanet.org/resources/userguide.html from the medical librarians association) and apply equally to Medicine 2.0.
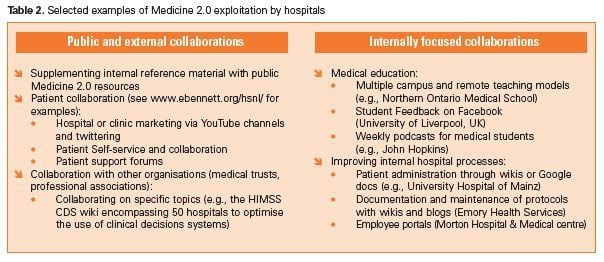
However, the utopian scenario for the user is single access point for Medicine 2.0 resources and local systems, which may take the form of Clinical data or reference material. As opposed to clinical data, internal medical reference, guidelines, lookup tables, terminologies or checklists can often overlap with broader and deeper resources available online. The two sources are complementary, eMedicine may give a better picture of overall diagnosis protocols, but local guidelines are critical to executing them in the specific context. The objective would be, therefore, not to promote external over internal sources, but find an efficient manner of delivering simultaneous access to both. In other knowledge intensive industries, companies are addressing similar issues via improved access to internal and external data, aligned with knowledge creation platforms based on Web 2.0 principles. Concretely, this involves developing ‘single search’ across datasets, coupled to user’s expertise profiles to highlight both codified internal and external data and tactic expertise. Platforms such as REALCOM’s AskMe, Google’s Search Appliance and behind firewall capabilities, FatWire Software’s TeamUp, or IBM’s OmniFind are example market solutions targeting this space. To date, they have mainly penetrated the healthcare sector via clinical collaborators in pharmaceutical companies. The cost of standardising internal data remains a hurdle to implementing this approach, and given constrained healthcare IT budgets, initial steps may need to focus on integrating a limited set of prioritised internal data against a long-term roadmap in order to begin the journey towards this ideal.
Medicine 2.0: Life Beyond the World Wide Web
Medicine 2.0 approaches can be used to improve existing internal processes, clinical systems or create new sources of local information, and do not necessarily mean a World Wide Web presence. Given the relative low cost of Web 2.0 addons (blogs, wikis, rating systems and community portals), the temptation is to supplement existing internal systems or create Medicine 2.0 specific platforms to address any inefficiencies in knowledge management and user collaboration. From a policy perspective, this delivers the best of both worlds, with the benefits of user generated content, as well as a degree of control over the content used. There are numerous examples of successful small-scale Web 2.0 implementations in healthcare organisations, such as the use of wikis to structure and track clinical research projects or document local protocols and processes, or the use of twitter and RSS feed for informing collaborators about events. One such example is Emory Health Services, which has 10,000 employees at four hospitals and numerous physician clinics across Georgia. Emory implemented a wiki and blog based collaboration platform for clinics to follow and develop specific protocols for patient care. The change has resulted in less travel and manual processes, and in addition to the time savings, allowed discussions and amendments are stored in a repository, where they can be secured and audited.
Getting it Right: Users, Scope and Control
This said, replicating large scale Medicine 2.0 models from the internet can be difficult. The lifeblood of Web 2.0 models is user activity, including ‘lead-users’ that represent a small proportion of the population, but who generate a large proportion of the content. The breadth of and relative interest of the Web 2.0 topic must be aligned with the potential user base, and clearly for internal collaborations the available user bases can be much, much lower than on the world wide web. Broad ambitious projects that target a heterogeneous but small number of users may fail due to lack of content depth, and failure of processes such as Apomediation. Given this, prerequisites for implementing a Medicine 2.0 resource include identifying an early lead-user base, ensuring that the scope of collaborations is constrained, providing incentives for initial use, and the levering of existing platforms to lower initial barriers to use. Lowering these barriers may involve using either existing Web 2.0 tools such as Facebook, or existing internal profile information and sign on for existing content management systems such as SharePoint. Careful consideration must be regarding developing a fully internal resource, rather than collaborating with other organisations to increase the user base.
Finally, managers need to live with negative or critical posts, to deploy beta solutions, and allow users to take control and evolve the nature of the participation wherever possible. Overall, much control may need to must be relinquished, but this should not be interpreted as a ‘build it and set it free’ approach. Specific goals and outcomes should be set, incorporating evaluation metrics at every step. Additionally, though the technology around Medicine 2.0 represents a significant step in technical capabilities, it cannot create a culture of knowledge management, and any strategy must consider the human element of the specific context. Addressing these issues is highly feasible, given a clearly articulated and communicated strategy.