HealthManagement, Volume 4 - Issue 1, 2010
Diastolic dysfunction represents a mechanical malfunction of the relaxation of the left ventricular chamber primarily diagnosed by two-dimensional transthoracic echocardiography and in most cases, has no immediate clinical relevance. The abnormal relaxation is usually separated in different degrees based on the severity of reduction in passive compliance and active myocardial relaxation. Diastolic heart failure, in contrast, is a clinical diagnosis in patients with signs and symptoms of heart failure but with preserved left ventricular function and normal ejection fraction, and is often seen in patients with long-standing history of hypertension or infiltrative cardiac diseases. The question of whether diastolic dysfunction will ultimately lead to diastolic heart failure is critically reviewed based on data from the literature. Treatment recommendations for diastolic heart failure are primarily targeted at risk reduction and symptom relief. Currently, few data have been reported on diastolic dysfunction and its progression to systolic heart failure.
Introduction
Even though often interchangeably used in a clinical setting, there is a distinction between diastolic dysfunction and diastolic heart failure. A PubMed literature search revealed a total of 1,478 articles using the search terms diastolic heart failure and review. In contrast, few randomised controlled trials are available on diastolic heart failure alone. Controversy remains regarding the optimal therapy for patients with either diastolic dysfunction or diastolic heart failure. An important question is whether diastolic dysfunction does indeed lead to diastolic heart failure and how this progression occurs. Moreover, it is unclear whether diastolic dysfunction consequently results in both diastolic and subsequently, systolic heart failure.
In daily routine, heart failure oftentimes is separated into
systolic and diastolic failure based on preservation of left ventricular ejection
fraction. The terms “heart failure with preserved left ventricular function” or
“heart failure with normal ejection fraction” are used to emphasise that the
etiology of the pathophysiology for this group of patients may go beyond
diastolic dysfunction alone. Heart failure in general and diastolic heart
failure in particular causes a significant financial burden and increasing consumption
of healthcare resources, especially among the elderly population (i.e., for
patients 65 years of age or older). The present article will review the current
knowledge of diastolic dysfunction and its progression to diastolic heart
failure.
Diastolic Dysfunction
Diastolic dysfunction is a mechanical abnormality brought on by a breakdown in the passive (compliance) and active (myocardial relaxation) intrinsic properties of the ventricle during diastole. Myocardial hypertrophy (e.g. left ventricular hypertrophy secondary to hypertension) and myocardial ischaemia have been shown to impair the energy-dependent process of myocardial relaxation. The increased afterload in patients with aortic stenosis or hypertension can also inhibit myocardial relaxation by reducing the ability of the left ventricle to contract to small end-systolic volume, and hence limit the ensuing elastic recoil’s ability to enhance myocardial relaxation.
Also, diastolic dysfunction can be secondary to pathological
states that adversely affect passive compliance during diastole, such as increases
in myocardial wall thickness observed in concentric hypertrophy as a result of
longstanding hypertension, or in myocardial fibrosis in patients with
infiltrative pathology.
The Role of Echocardiography in the Assessment of Diastolic Function
Diastolic function can be evaluated noninvasively using two-dimensional transthoracic echocardiography. The evaluation of left ventricular diastolic function should be an essential part of any echocardiography examination. The three phases of diastole consist of a period of isovolumic relaxation time (IVRT) followed by early rapid diastolic filling period (E), a plateau and finally a late filling due to the atrial contraction or atrial kick (A). These can be evaluated by using the pulse wave (PW) Doppler of the mitral valve and pulmonary veins. The left ventricular filling pattern obtained will therefore indirectly reflect the left ventricular filling pressures.
A complete left ventricular diastolic assessment should include
assessment of the IVRT, peak E velocity, peak A velocity, E/A ratio,
deceleration time (DT), and A duration, which are obtained from the transmitral
inflow velocities. Pulmonary vein (PV) flow velocities are then measured, which
include four components: two systolic velocities (PVs1) and (PVs2), diastolic
velocity (PVd), and atrial flow reversal (PVa). Based on the echocardiographic parameters,
diastolic dysfunction has been divided in three different grades of severity of
ventricular compliance, relaxation rate, and filling pressures.
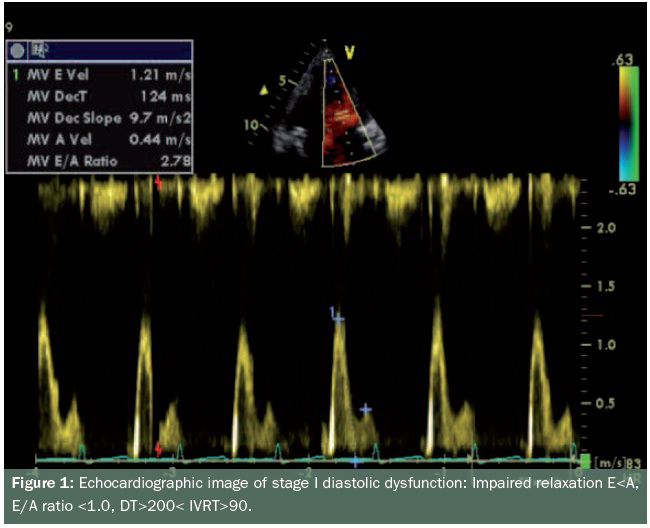
- Stage one is the mildest form of diastolic dysfunction with delayed relaxation defined by an early filling to late or atrial filling (E/A) ratio less than 1, prolonged IVRT and prolonged DT. The systolic to diastolic pulmonary venous (S/D) ratio is greater than 1 (see figure 1)
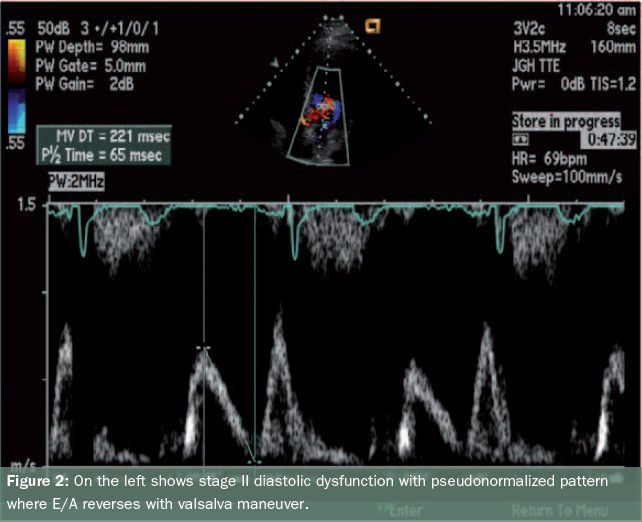
- Stage two is marked by a moderate level of dysfunction and defined by E/A of greater than 1 and/or greater than 2 with S/D less than 1, and is often called pseudonormalisation (with a normal diastolic filling pattern), caused by elevated left atrial pressures. This can be unmasked by reducing preload, for example by use of the Valsalva maneuver or application of sublingual nitroglycerine (see figure 2,).
- Stage three is marked by a restrictive filling pattern and signifies severe diastolic dysfunction, i.e., decreased compliance and marked increase in left atrial pressure. The E/A is greater than 2, IVRT and DT are short, S/D is less than 1 (see figure 3). The mitral A duration is shorter than the PVa duration.
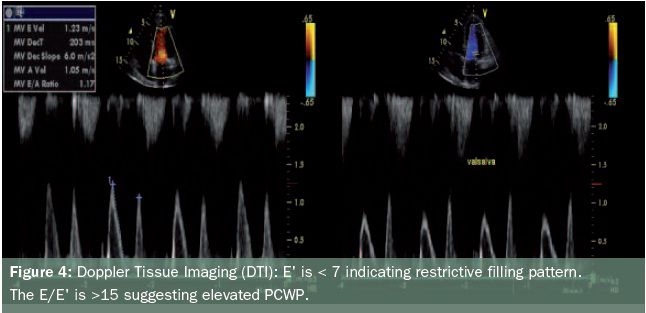
Mitral annular velocity by tissue Doppler imaging also has been
used to assess diastolic function. This referred to as E’. The E m (mitral)/ E’ (annular)
ratio has been found to correlate well with increased pulmonary capillary wedge
pressure (PCWP).The E/E’ ratio is normally less than 8. The E’ is shown to be
low in restrictive stage less than 8. A ratio of greater than 15 indicates elevated
PCWP (see figure 4). Although rarely performed for evaluation of diastolic
dysfunction alone, the most accurate invasive diagnostic technique is cardiac catheterisation
with direct measurements of left ventricular end-diastolic pressure. Parameters
of chamber stiffness are correlated with changes in pressure to changes in
chamber volume.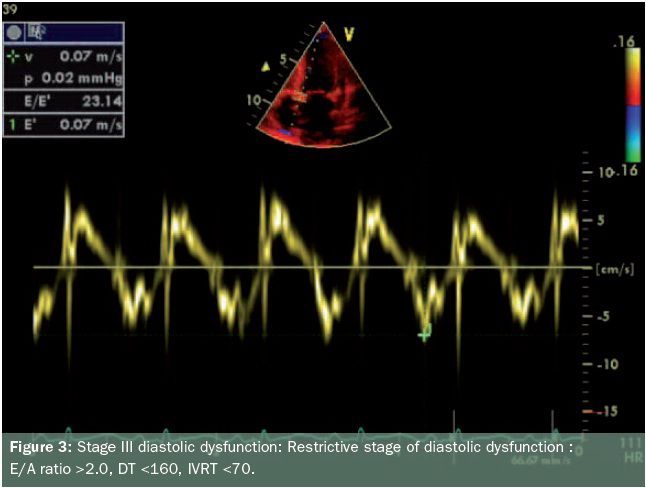
Left Ventricular Diastolic Dysfunction
In its simplest form, left ventricular diastolic dysfunction is defined as impairment in the capacity of the left ventricle to accept blood without a compensatory increase in left atrial pressure. Patients with left ventricular diastolic dysfunction tend to have elevated left ventricular diastolic pressure in the presence of normal or even reduced left ventricular volume, as the pressure- volume curve in these patients is shifted upwards. Over the years, a variety of co-morbid conditions have been associated with development of left ventricular diastolic dysfunction, such as myocardial scarring, transmural myocardial infarction, chronic constrictive pericarditis, chronic coronary artery disease, dilated cardiomyopathy, hypertrophic cardiomyopathy, diabetic cardiomyopathy, hypertension, aortic stenosis as well as normal aging.
The underlying connection in the possible etiologies of left
ventricular diastolic dysfunction is their ability to hinder one or both of the
intrinsic diastolic properties of compliance or relaxation. Pathological states
such as fibrosis and concentric hypertrophy can reduce compliance of the
myocardium by increasing passive ventricular stiffness, thereby affecting the
passive property of compliance in diastole. Ischaemia and disease processes leading to
increased afterload affect diastole by impairment of the active rate of
relaxation.
Left Ventricular Diastolic Dysfunction and Heart Failure
The prevalence as well as overall significance of diastolic heart failure has become distinctly apparent. Diastolic heart failure was originally reported in 1937 when Fishberg referred to it as “hypodiastolic failure”, a form of cardiac insufficiency secondary to inadequate filling of the left ventricle during diastole. A half a century later, Kessler became the first to discuss the clinical syndrome of diastolic heart failure. Over the years, a number of landmark publications have guided our current understanding for diagnosing diastolic heart failure. Recognising the difficulty of non-invasive assessment of the LV diastolic function, in 2000, Vasan and Levy proposed a classification scheme for diagnosis of diastolic heart failure in the hope of reducing the difficulty for diagnosis of this rather prevalent pathology.
According to the degree of diagnostic certainty, patients were partitioned into possible, probable, or definite diastolic heart failure. While keeping the need for evidence of heart failure for all categories, the diagnosis of probable or definite diastolic heart failure required evidence of normal left ventricular systolic function within three days of an initial heart failure event. Most importantly it was argued that “evidence of abnormal LV relaxation, filling, diastolic distensibility, or diastolic stiffness” is required for a definite diagnosis of diastolic heart failure. More recently, Zile and colleagues published several prospective studies concluding that the diagnosis of diastolic heart failure does not require objective recording of left ventricular diastolic dysfunction but only documentation of preserved systolic function. In two separate studies using both Doppler echocardiography and cardiac catheterisation, the authors observed a statistically significant percentage of patients with clinical diagnosis of heart failure and normal ejection fraction (EF >45 percent) suffering from abnormalities in active relaxation or passive compliance.
The degree of involvement that left ventricular diastolic dysfunction plays in preserved ejection fraction heart failure is debatable and has been the major argument made by those that believe diastolic heart failure is the correct diagnosis for patients with heart failure and normal ejection fraction, given that these patients do not suffer from significant valvular, pericardial or pulmonary disease. Left ventricular diastolic dysfunction has also been found to be present in patients with heart failure and reduced ejection fraction, a form of heart failure that was originally believed to be mainly secondary to a systolic dysfunction pathophysiology.





