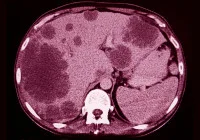
Accurate preoperative assessment of ovarian cancer spread is crucial for determining tumour resectability and guiding treatment strategies. While contrast-enhanced computed tomography and magnetic resonance imaging remain standard diagnostic tools, ultrasound is gaining prominence for its real-time imaging capabilities and accessibility. A recent study published in Ultrasound in Obstetrics & Gynecology evaluated the accuracy and consistency of ultrasound examiners—ranging from less experienced to highly experienced—in detecting cancer infiltration across defined anatomical regions using preacquired videoclips. By examining diagnostic confidence, image quality and inter-rater agreement, the study sought to determine the viability of ultrasound in advanced cancer staging when operated by differently skilled clinicians.
Study Design and Rater Classification
The study formed part of the Imaging Study in Advanced Ovarian Cancer (ISAAC) and focused on a secondary aim: evaluating the ability of ultrasound raters to detect cancer spread using 380 pre-recorded videoclips. These clips were obtained from 96 patients with a high prevalence of ovarian cancer spread, covering 19 anatomical sites grouped into four regions: pelvis, middle abdomen, upper abdomen and lymph nodes. Sites critical for assessing tumour resectability were also specifically included. Each anatomical site featured ten clips with and ten without visible cancer infiltration, judged against surgical, histological or treatment response findings.
Must read: Updated Imaging Guidelines for Ovarian Cancer
Twenty-five gynaecologists from six countries were recruited and categorised into two groups based on their training and experience. Those with over ten years' experience or performing at least 100 relevant scans annually were deemed highly experienced. The others, with fewer years or scans, were considered less experienced. Despite this difference, all raters were certified as Level II or III ultrasound practitioners according to European guidelines.
Performance Outcomes and Influencing Factors
The results revealed high overall diagnostic performance. The mean accuracy for all raters ranged from 70% to 100%, with a median of 100% in the pelvic region and slightly lower but still high figures in other regions. Interestingly, the likelihood of correctly identifying cancer infiltration did not differ significantly between highly and less experienced raters. Instead, accuracy was most influenced by two key factors: the quality of the video image and the examiner's confidence in their diagnosis.
The pelvic region yielded the highest rate of correct classifications, followed by the middle abdomen, lymph nodes and upper abdomen. For regions whose infiltration indicated non-resectability, performance remained strong, further validating the reliability of ultrasound for high-stakes clinical decisions. The generalised linear mixed model analysis confirmed that higher image quality and greater diagnostic confidence significantly improved accuracy. In contrast, rater experience level, training type, institutional setting and routine use of ultrasound had no measurable effect on diagnostic success.
Inter-rater Agreement and Reliability by Anatomical Region
Another central outcome was the assessment of inter-rater agreement. The consistency with which different raters classified cancer infiltration across anatomical regions was quantified using the Fleiss kappa statistic. Agreement was highest for the pelvic sites and lowest for those in the upper abdomen. However, even in the least consistent areas, agreement remained substantial to very good, indicating a robust consensus among professionals regardless of experience level.
These findings underscore the strength of structured ultrasound protocols and suggest that high-quality video materials can support reliable remote assessment by various practitioners. The methodology’s design—limiting bias by ensuring that raters were blinded to clinical details and enabling repeat reviews of clips—enhanced the study’s internal validity. Moreover, the use of a rigorous statistical model allowed for nuanced insights into what factors genuinely impact diagnostic success.
The study demonstrated that ultrasound examiners, regardless of experience level, can reliably evaluate ovarian cancer spread when using high-quality, standardised video recordings. Diagnostic confidence and image clarity proved to be more decisive than training background or institutional environment in determining accuracy. The findings support the inclusion of structured ultrasound evaluations in oncological settings, particularly when guided by consistent imaging standards and supported by appropriate training in image interpretation. As such, preoperative ultrasound, when performed and reviewed under controlled conditions, holds considerable promise as a complementary tool in ovarian cancer staging.
Source: Ultrasound in Obstetrics & Gynecology
Image Credit: iStock