Based on stage at diagnosis of breast cancer, the greatest mortality reduction is achieved with mammography utilisation starting at the age of 40. This is the main finding of a study that compared estimated 5-year mortalities of patients diagnosed with breast cancer based on stage at diagnosis and national screening mammography guideline categorisation.
"Annual mammography before breast cancer is predictive of increased overall survival, and the results of this study also demonstrated that reduction in overall and stage I to IV mortalities was greatest with a programme based primarily on annual mammography," says study author Samir B. Patel, MD, of Elkhart General Hospital, Elkhart, Indiana, USA.
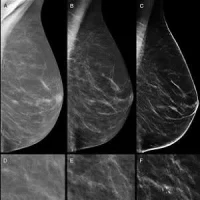
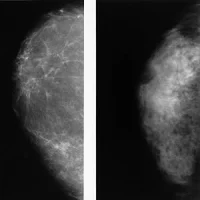
Breast cancer is the most common cancer diagnosed in women, excluding skin cancer, and is the second leading cause of cancer deaths in women. Mammography utilisation has the greatest impact on reduction (up to 59%) in breast cancer deaths. Breast cancer survival is related to many factors, but stage at diagnosis is a critical determinant, with greater survival at a lower stage at diagnosis.
The current study included 445 patients diagnosed with breast cancer from 2010 to 2014. Percentages of invasive cancers, stage 0 + I of total cancers, and stage I of invasive cancers, were calculated based on stage at diagnosis and Surveillance, Epidemiology, and End Results (SEER) database stage mortality estimates. Programme categories defined included an Annual Programme, based on the ACR (annual screening age 40 and above), a Biennial Programme, based on the U.S. Preventative Services Taskforce (biennial screening ages 50 to 74 years), and a Hybrid Programme, based on the American Cancer Society (annual screening ages 45 to 54 years, then biennially at ages 55 and above), including respective interval cancers.
Comparing programme categories, the Annual Programme had the lowest percentage of invasive cancers (75.3%), highest percentages of stage 0 + I of total cancers (75.3%) and stage I of invasive cancers (67.1%), and the lowest 5-year estimated overall (10.1%) and stage I to IV (12.0%) mortalities. Estimated overall and stage I to IV mortalities for the Annual Programme was 37.3% and 30.6% less, respectively, than the Biennial Programme, and 31.8% and 26.8% less, respectively, than the Hybrid Programme.
"Tumour stage is a determinant of long-term survival, with reduced cancer deaths from screening, which was demonstrated in this study by observing a significant reduction in the percentage of invasive cancers, higher percentages of stage 0 + I of total cancers, and higher percentage of stage I invasive cancers for screening-detected cancers compared with nonscreening-detected cancers," Dr. Patel notes.
The results also show that the number of interval cancers (nonscreening detected) increases with a longer interval between screenings and is associated with increased breast cancer mortality.
The study has several limitations, including retrospective design, single institution, and a relatively short time frame of five years for review. Also, overall and stage I to IV mortalities were estimated based on SEER data, as opposed to utilisation of actual observed mortality. Utilisation analysis based on family history, personal history of high-risk lesion or presence of breast cancer genes associated with increased breast cancer risk, referring physician preference for frequency of mammography recommendation, and socioeconomic status, was not performed, which could influence mammography utilisation and subsequent stage at diagnosis.
Image Credit: Pixabay
References:
Patel SB (2018) Estimated Mortality of Breast Cancer Patients Based on Stage at Diagnosis and National Screening Guideline Categorization. J Am Coll Radiol 2018; Available online 21 May 2018 https://doi.org/10.1016/j.jacr.2018.04.010
Latest Articles
Mammography, breast cancer, breast cancer screening
Based on stage at diagnosis of breast cancer, the greatest mortality reduction is achieved with mammography utilisation starting at the age of 40. This is the main finding of a study that compared estimated 5-year mortalities of patients diagnosed with br