Coronary artery calcium (CAC) serves as a crucial predictor of cardiovascular risk, particularly in asymptomatic individuals, but it's also valuable for assessing risk in symptomatic patients. Current methods for assessing CAC involve calcium scoring CT (CSCT), which calculates the Agatston score. However, spectral CT systems offer the potential to perform CAC scoring directly from coronary CT angiography (CCTA) scans by separating iodine and calcium. Photon counting CT (PCCT) is a promising technology in this regard, allowing for detailed material differentiation. Previous methods like virtual non-contrast (VNC) reconstructions have limitations in distinguishing calcium from iodine. A new approach involves virtual non-iodine (VNI) reconstructions, which show promise in enabling accurate CAC scoring from CCTA scans. However, existing studies have shown that CAC scores derived from CCTA may underestimate true values. Further research is needed to optimise reconstruction parameters for CCTA scans acquired on PCCT systems and to validate the accuracy of CAC scores obtained through this method compared to CSCT.
Mimicking Realistic Coronary Artery Imaging Conditions Using a Dynamic Phantom
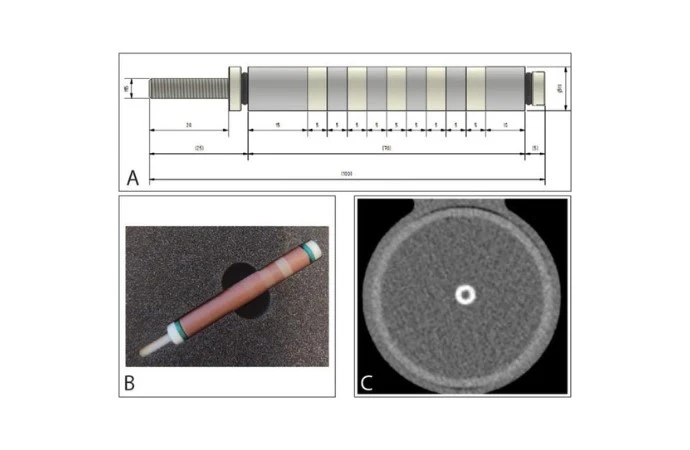
A hollow artificial artery was embedded within an anthropomorphic thorax phantom, which mimicked the structure of a human chest. To emulate large patient dimensions, a fat-tissue equivalent extension ring was placed around the thorax phantom. The artery, made of a solid substance with water density, contained cylindrical hydroxyapatite (HA) calcifications of varying densities. These calcifications had identical dimensions but differed in density levels: very low, low, medium, and high.
During calcium scoring CT (CSCT) scans, the artery lumen was filled with a mixture of water and glucose to replicate the density of blood, while for coronary CT angiography (CCTA) scans, iodinated contrast agent was additionally introduced. The contrast agent resulted in a certain Hounsfield Unit (HU) value at a virtual monoenergetic image (VMI) level, akin to conventional CT images.
To mimic the motion of coronary arteries during scanning, a robotic arm translated the artery horizontally at different velocities. The velocities corresponded to the mean in-vivo velocities of coronary arteries during various phases of the cardiac cycle, reflecting heart rates ranging from resting to elevated. The robotic arm's electrocardiogram (ECG) output was synchronised with the CT scanner's ECG input to ensure data acquisition during linear motion, without any abrupt changes in direction.
To account for inter-scan variability, each acquisition was repeated five times with manual repositioning of the setup between scans, involving slight translations and rotations. This setup aimed to simulate realistic conditions encountered during coronary artery imaging, considering both physiological motion and technical variability.
Imaging Protocol and Reconstruction Parameters for Calcium Scoring CT and Coronary CT Angiography
The study employed two types of scans: calcium scoring CT (CSCT) and coronary CT angiography (CCTA), both conducted on a dual-source photon counting CT system (NAEOTOM Alpha, Siemens Healthineers, Software version Syngo CT VA50).
For CSCT scans, the dynamic phantom was scanned without iodinated contrast. The protocol included a tube potential of 120 kVp, axial scan technique, 144 × 0.4 mm collimation, image quality level 16 (Care keV IQ), Quantum Iterative Reconstruction (QIR) off, virtual monoenergetic image (VMI) level of 70 keV, kernel Qr36, field-of-view 220 mm, matrix 512 × 512, and slice thickness/increment of 3.0/1.5 mm.
For CCTA scans, the dynamic phantom with iodinated contrast in the lumen was scanned using the same CT system. The protocol included the same tube potential, axial scan technique, collimation, field-of-view, and matrix as CSCT. However, image quality level was set to 65 (Care keV IQ), QIR was tested both off and on (QIR level 2), and two different kernels (Qr36 and Qr44f) were utilised. Slice thickness/increment were varied as 3.0/1.5 mm and 0.4/0.2 mm. All scans were reconstructed with virtual non-iodine (VNI, PURE Calcium, Siemens Healthineers) at 70 keV.
Agatston and volume scores were automatically determined using a validated automated scoring tool, with a threshold of 130 HU for calcium. Calcifications were categorised into five risk groups based on Agatston scores. To obtain CAC scores from CCTA acquisitions, various reconstruction settings were tested, including QIR off, Qr36f, and 3.0 mm slice thickness as standard CSCT reconstruction, as well as additional reconstructions at QIR level 2, Qr44f, and 0.4 mm slice thickness.
Calcium detectability was assessed, and each scan was verified for noise levels to prevent false positive scores. CAC scores from CCTA were categorised into risk groups based on agreement with CSCT scores, and the preferred reconstruction parameters for CCTA were determined based on the highest agreement in risk categorisation, measured using Cohen weighted linear κ.
Analysis of Calcification Detectability and Volume Scoring Agreement
The detectability analysis revealed that all calcifications were detected on calcium scoring CT (CSCT) scans, while most calcifications were also detected on coronary CT angiography (CCTA) reconstructions, except for very low and low-density calcifications with a 3.0 mm slice thickness.
Volume scores for very low and low-density calcifications were underestimated on static CSCT scans but overestimated for medium and high-density calcifications. The smallest difference between physical calcification volume and CCTA results was found with QIR off, Qr44f, and 0.4 mm slice thickness.
At different heart rates, volume scores showed consistent trends of underestimation for low-density calcifications and overestimation for medium and high-density calcifications. The best agreement in risk categorisation between CCTA and CSCT was achieved with QIR off, Qr44f, and 0.4 mm slice thickness, showing moderate agreement.
However, reconstruction settings with QIR level 2 and 3.0 mm slice thickness, as well as QIR off and 0.4 mm slice thickness, showed lower agreement in risk categorisation. These differences were not statistically significant.
Optimising Coronary Calcium Scoring with Photon-Counting CT: Promising Results and Considerations
This dynamic phantom study demonstrates that the performance of coronary calcium scoring using coronary CT angiography (CCTA) acquired from photon-counting CT (PCCT) with virtual non-iodine (VNI) reconstructions is promising. The study identifies optimal reconstruction parameters for CCTA, including QIR off, Qr44f reconstruction kernel, and 0.4 mm slice thickness, which significantly improve the detectability of low-density calcifications compared to standard reconstruction methods.
While the detectability of coronary calcium is excellent with these optimised parameters, discrepancies are observed in the Agatston and volume scores derived from CCTA compared to reference calcium scoring CT (CSCT) scans. Specifically, low-density calcifications tend to be underestimated in Agatston scores, while volume scores for very low and low-density calcifications are underestimated, and those for medium and high-density calcifications are overestimated. Despite these discrepancies, there is substantial agreement in risk classification between CCTA and CSCT.
The study discusses previous research findings on CCTA-based coronary artery calcium (CAC) scoring, noting consistent underestimations compared to CSCT, potentially due to limitations in calcium discrimination with VNI reconstruction. The improvements in calcium detectability observed in this study suggest the feasibility of CCTA-based CAC assessment on PCCT, but further refinement of reconstruction methods is necessary to enhance accuracy.
Limitations of the study include the use of relatively large calcifications compared to those typically observed in vivo, necessitating further validation in patient studies. Additionally, the application of 0.4 mm slice thickness deviates from traditional Agatston methodology, highlighting the need for novel calcium scoring methods that meet current technological capabilities.
While CCTA-based CAC assessment on PCCT with optimised reconstruction parameters shows promise, ongoing research efforts are needed to improve accuracy and clinical utility.
Source & Image Credit: European Radiology