A systematic review concludes that different imaging modalities, except for positron emission tomography (PET), have comparable sensitivity, specificity and diagnostic accuracy for the diagnosis of pancreatic ductal adenocarcinoma. The findings are published in European Journal of Radiology.
See Also: Benefit-Risk Assessment in Diagnostic Imaging
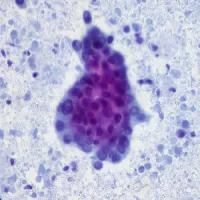
Pancreatic cancer, primarily pancreatic ductal adenocarcinoma (PDAC), accounts for 2.4 percent of cancer diagnoses and 5.8 percent of cancer death annually. The imbalance between incidence and mortality in pancreatic cancer can be partially explained by the fact that these cancers are often clinically silent until advanced stages, often following metastases. Patients who are diagnosed with localised disease have a 26 percent 5-year survival, while only 2 percent of patients diagnosed with advanced disease survive at 5 years. Thus, any improvement in detection will significantly improve survival in pancreatic cancer through earlier intervention.
Previous reviews of diagnostic imaging modalities used PDAC, the most common form of pancreatic cancer, have been undertaken. However these reviews have not taken into account the rapid advancement in imaging technology in their analysis. For example, it is inappropriate to compare modern nuclear imaging techniques such as PET to computed tomography (CT) or magnetic resonance imaging (MRI) technology from 20 years earlier. The current review aimed to determine the sensitivity, specificity and diagnostic accuracy of the available imaging modalities for the detection of PDAC.
A systematic search was applied to PubMed/MEDLINE, EMBASE, Cochrane and CINAHL from January 2004 to June 2015 in order to identify all publications that reported on the accuracy of MRI, CT, PET, PET/CT, or ultrasound in the diagnosis of PDAC. Proportional meta-analysis was performed for each modality.
A total of 5,399 patients, 3,567 with PDAC, from 52 studies were included in the analysis. The sensitivity, specificity and diagnostic accuracy were 93%, 89% and 90% for MRI; 90%, 87% and 89% for CT; 89%, 70% and 84% for PET; 91%, 86% and 89% for endoscopic ultrasound (EUS); and 88%, 94% and 91% for transabdominal ultrasound (TAUS).
"The results of this meta-analysis stand in contrast to the previously published literature reviews on this topic. A 2005 meta-analysis found helical CT to be the most sensitive and specific modality and ultrasound to be the least useful. Because the literature search in the 2005 review was restricted to studies conducted prior to December 2003, there is no overlap with the current review, which found higher sensitivities and specificities for all modalities (most significantly for ultrasound). While these differences may simply reflect technological advances in pancreatic imaging, the very nature of this evolution warrants repeated review," the authors write.
Further research is needed to systematically evaluate the other aspects of each imaging modality, such as cost and adverse effect profile, which were outside the scope of this review, the authors add.
Source: European Journal of Radiology
Image Credit: Lee Health
References:
Toft, James et al. (2017) Imaging modalities in the diagnosis of pancreatic adenocarcinoma: A systematic review and meta-analysis of sensitivity, specificity and diagnostic accuracy. European Journal of Radiology; DOI: http://dx.doi.org/10.1016/j.ejrad.2017.04.009
Latest Articles
pancreatic cancer, positron emission tomography, PET, pancreatic ductal adenocarcinoma
A systematic review concludes that different imaging modalities, except for positron emission tomography (PET), have comparable sensitivity, specificity and diagnostic accuracy for the diagnosis of pancreatic ductal adenocarcinoma.