Magnetic compression anastomosis (MCA), also known as Magnamosis, is a minimally invasive procedure used to treat obstructions in the biliary, oesophagal, colonic, and ureteric tracts, as well as for diversion procedures like gastrojejunostomy or jejunojejunostomy. The procedure involves two steps: first, placing rare-earth magnets at the ends of the obstruction, and second, traversing the occlusion using a guiding catheter once the magnets adhere to each other, confirmed by plain radiographs. MCA is noted for creating both anatomical and non-anatomical anastomoses, achieving full-thickness connections with serosal apposition, rapid epithelisation, and reduced inflammation, suggesting longer-lasting results. Despite its growing popularity and demonstrated efficacy, particularly in reducing stricture recurrence, there is a need for more long-term follow-up data. Patients with obstructions due to malignant tissue infiltration may not be ideal candidates due to the limits of magnetic attraction.
A critical review published in Insights into Imaging provides a comprehensive review of magnetic compression anastomosis (MCA) applications, supported by illustrative cases. Magnets were delivered over wires, with sizes ranging from 5 to 18 F. Larger-sized magnets are utilised in oesophagal, colonic, and ureteroileal anastomosis obstructions compared to biliary and ureteral obstructions, enhancing magnetic adherence and improving success rates, particularly for longer obstructions.
Hepatobiliary Obstruction
The majority of the literature on magnetic compression anastomosis (MCA) focuses on its application in treating biliary obstructions. These obstructions are common in liver transplant recipients and can also result from iatrogenic injuries during procedures like cholecystectomy, leading to significant biliary stenosis or complete obstruction. MCA can be utilised in both native and transplanted livers, but thorough assessment of the obstruction is critical for success. Endoscopy is particularly important for MCA in hepatobiliary cases, more so than for oesophagal and ureteric obstructions. Key steps include retrograde catheterisation of the cystic duct in cases of clipped bile ducts and the afferent loop in Roux-en-Y hepaticojejunostomy.
Native Liver
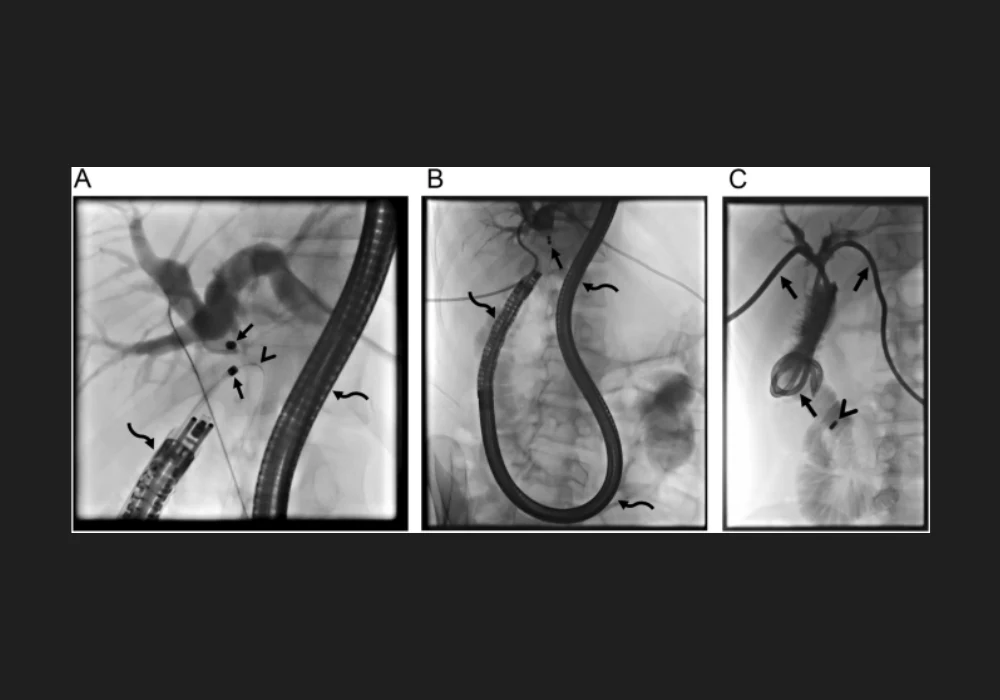
Magnetic compression anastomosis (MCA) is less commonly used for biliary obstructions in native livers compared to transplanted livers. Most cases involve post-surgical bilioenteric anastomosis strictures and traumatic injuries. Percutaneous biliary interventions are generally preferred for treating these strictures, as endoscopic retrograde cholangiopancreatography (ERCP) is challenging due to altered anatomy, such as in Roux-en-Y hepaticojejunostomy. Despite the difficulties posed by ERCP, MCA can be performed if access to the stricture site is achieved using a long endoscope (colonoscope or enteroscope). Bile duct injuries during cholecystectomy, especially in patients with anatomical variations, can lead to complete obstructions. Variations in the right accessory biliary duct are often responsible for these injuries. MCA can restore bile flow by creating a connection between the remaining part of the right accessory biliary truncus and the cystic duct. Direct injuries to the common bile duct may also result in obstructions, typically treated with hepaticojejunostomy if detected during surgery. Rapid intervention is crucial for post-surgical detection to prevent duct retraction, which could hinder MCA.
Transplant Liver
Following liver transplant surgery, various risk factors contribute to biliary complications. These include small or multiple anastomoses, post-surgical adhesions or inflammation, and hepatic artery-related issues like decreased blood supply or occlusion. Bile leaks can also lead to biliary stricture formation, potentially progressing to complete obstruction. Biliary strictures post-transplantation can be anastomotic or non-anastomotic, with anastomotic ones being more common and generally more manageable through percutaneous and endoscopic procedures. Non-anastomotic strictures have a poorer prognosis and may arise from different causes. Management varies based on the type of anastomosis performed during transplantation. Endoscopic procedures are commonly used for anastomotic strictures, with percutaneous interventions reserved for failed endoscopic attempts or hepaticojejunostomy anastomoses. Complete biliary obstructions are not uncommon post-transplantation, and magnetic compression anastomosis (MCA) presents a potential alternative to revision surgery, which is the conventional treatment option in such cases.
Urinary Obstruction
Recent literature highlights the successful application of magnetic compression anastomosis (MCA) in treating ureteric obstructions. While most ureteral obstructions can be traversed with guidewires, some may be impassable. Unlike with biliary occlusions, endoscopic guidance is typically unnecessary for MCA in ureteral obstructions. Technical advancements have facilitated catheterisation of the distal ureter under imaging guidance with minimal steps and basic tools. One concern regarding MCA for urinary obstructions is infection related to long-standing nephrostomy catheters, which may be encountered to some extent in hepatobiliary obstructions but not expected in gastrointestinal obstructions due to the absence of drainage catheters.
Native Ureter
Radiotherapy used in the treatment of gynaecological malignancies can lead to a significant narrowing of the ureters. During catheterisation of ureteral strictures, caution is necessary to prevent disruption of ureteral integrity and the creation of false lumens, which may result in total ureteral occlusion. Finding the true lumen beyond the stricture can be challenging once a false lumen forms. Ureterovaginal fistula (UVF) is another complication observed in patients post-gynecological surgery or radiotherapy. Surgical treatment is generally avoided, with preference for less invasive options like imaging or cystoscopically guided procedures. Timely diagnosis is crucial to prevent fistula maturation, and interventions should be promptly initiated upon identification. In chronic cases, wire access beyond the fistula may fail to establish urinary diversion, but magnetic compression anastomosis (MCA) can potentially restore the connection between the bladder trigone and the caudal part of the ureter, even in chronic UVFs.
Post-Surgical Urinary Anastomosis
Cystectomy with ileal conduit is a surgical procedure for bladder cancer patients where the ureters are connected to a reconstructed bladder in the lower abdomen. Strictures in the ileoureteral anastomosis can occur due to inflammation, urinary leaks, or surgical errors. These strictures can be managed with antegrade or retrograde access via nephrostomy or existing ostomy. Care must be taken during catheterisation to prevent ureteral distraction, which could lead to permanent nephrostomy placement. Surgery is generally avoided for these obstructions, with interventional radiologists playing a crucial role in management. The use of an ileal pouch with an existing ostomy allows for the insertion of larger magnets in MCA, making it suitable for treating severe strictures. MCA has also shown effectiveness in treating total ureteral obstructions in renal transplant recipients.
Gastrointestinal System Obstruction
Esophageal obstructions, arising from head and neck cancer treatment or esophageal atresia in adults and paediatric patients, respectively, are often managed with dilation or stenting. Surgical resection may be necessary in cases of failure, posing challenges due to patient's condition and surgical complexity. Magnetic compression anastomosis (MCA) has been applied in gastrointestinal obstructions, including paediatric cases. Access for oesophagal obstructions can be facilitated through a gastrostomy tube for enteral nutrition and endoscopy or fluoroscopy-guided wire insertion. MCA is also effective for small and large intestinal obstructions, providing a minimally invasive option for reconstruction, such as gastrojejunostomy. While the use of metallic stents post-MCA in small intestine obstructions is debated, caution is advised to prevent premature dilation and potential perforation. MCA is particularly advantageous in impassable colonic obstructions, offering a minimally invasive alternative to revision surgery, often needed due to previous surgeries or radiotherapy. In colonic obstructions, MCA can be performed with magnets inserted through the anus and an existing enterostomy.
Techniques, Tips, and Tricks During MCA
Patient selection is crucial for successful magnetic compression anastomosis (MCA). Long segment obstructions can lead to technical failures and complications during magnet removal. Evaluation of stricture length is best achieved with both cranial and caudal wire accesses to the stricture site. Once wire accesses are established, magnets are pushed over the wires to the stricture site, with daily radiographs to monitor magnet apposition. Spontaneous magnet fall should be expected in gastrointestinal obstructions, delaying attempts at wire access beyond the obstruction until this occurs to prevent perforation. In cases of failure, magnets placed in safe locations like the distal main bile duct or rectum pose less risk, while magnets in risky areas like intrahepatic bile ducts, oesophagus, or urinary system should be promptly removed. A modified Nelaton catheter can aid in magnet removal under fluoroscopy. Correct magnet orientation is essential to prevent repulsion; a guiding catheter can be used to adjust magnet position if needed. Procedure delay is advised in cases of extravasation to prevent magnet migration into the abdominal cavity.
Source & Image Credit: Insights into Imaging