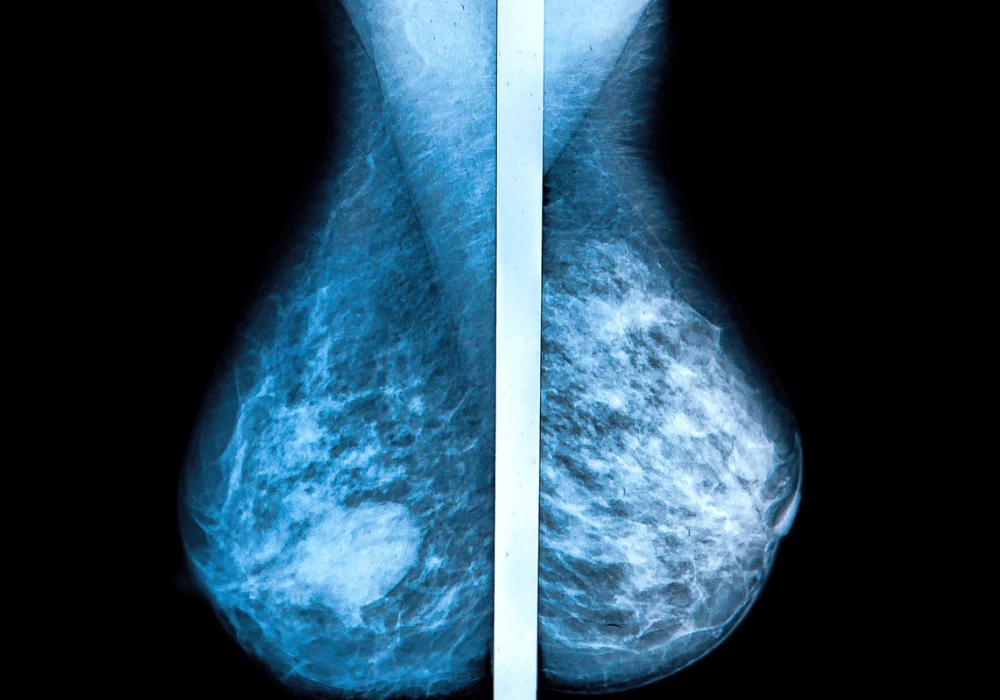
Digital breast tomosynthesis (DBT) has demonstrated improved breast cancer detection rates compared to traditional digital mammography (DM). However, cancers can still go undetected during screening, raising concerns about the accuracy and interpretation of results. The Malmö Breast Tomosynthesis Screening Trial (MBTST) investigated the effectiveness of one-view DBT versus two-view DM and explored the reasons behind non-detected cancers. This study aimed to identify the characteristics of missed cases, analyse radiographic patterns and understand the factors influencing non-detection, contributing to ongoing research into optimising breast cancer screening methods.
Characteristics of Non-Detected Cancers
The MBTST study analysed 89 cancers not detected during DBT screening, comprising interval cancers, those identified in the subsequent screening round and those detected only by DM. These cases were further classified into true negatives, false negatives and non-visible cancers. False negatives, accounting for 25% of the missed cases, were primarily due to normal-appearing densities that masked tumour presence. Comparatively, DM screening revealed a slightly lower false-negative rate of 18%.
A significant factor influencing non-detection was breast density. False negatives were more commonly observed in women with lower breast density (36% compared to 61% in true positives). Additionally, spiculated densities were less frequent in false negatives than in true positives, contributing to the challenges in detection. These findings underscore the complex nature of breast tissue characteristics and their impact on screening outcomes. Understanding how these factors interplay is essential for developing better imaging techniques and improving detection rates.
Radiographic Features and Imaging Challenges
Radiographic analysis revealed distinct patterns in non-detected cancers. False negatives often exhibited benign-appearing densities, spiculated features and indistinct densities, making them harder to identify during initial screenings. Notably, cancers with calcifications and architectural distortions were also frequently misinterpreted. The study emphasised that standard screening views might not always provide sufficient visual clarity, leading to misinterpretations or oversight.
Imaging interpretation errors also played a significant role in non-detection. Many cancers classified as minimal signs or non-visible had subtle features that were either overlooked or misclassified as non-suspicious. The reliance on a single DBT view further limited the detection of certain tumour presentations, suggesting the need for enhanced imaging protocols or multiple views for improved accuracy.
Implications for Screening Practices
The MBTST findings reveal essential insights for improving breast cancer screening strategies. The slightly higher false-negative rate in DBT screening compared to DM highlights the importance of continuous refinement in DBT techniques and the need for further studies on optimal screening methods. Incorporating additional imaging angles, synthetic mammography or advanced image processing could potentially reduce false negatives.
Furthermore, the study suggests a promising role for artificial intelligence (AI) in enhancing screening accuracy. AI tools could assist radiologists in identifying subtle patterns and reducing interpretation errors, particularly in cases with minimal or benign-appearing densities. Additionally, radiologist training focused on recognising challenging radiographic features, such as spiculated densities and calcifications, could further improve detection rates.
Another consideration is the need for personalised screening protocols. Women with lower breast density and specific tumour characteristics may benefit from different screening approaches or more frequent follow-ups. Screening strategies must evolve to address varying patient profiles, ensuring optimal detection rates across diverse populations.
While one-view DBT offers enhanced breast cancer detection capabilities compared to traditional DM, undetected cancers remain a concern due to imaging limitations and tissue characteristics. The MBTST study underscores the need for ongoing improvements in imaging protocols, radiologist training and the potential integration of AI tools. By addressing these challenges and exploring technological advancements, breast cancer screening accuracy can be further enhanced, ultimately leading to earlier detection, improved treatment outcomes and better survival rates for patients.
Source: European Radiology
Image Credit: iStock