Breast cancer is the most common cancer in women, with significant global incidence and mortality rates. The TNM classification system is crucial for accurately determining the extent and progression of the disease, guiding treatment decisions and improving patient outcomes. Currently, ultrasound is the primary method for assessing axillary lymph nodes in breast cancer, but it lacks standardised criteria for evaluation. Other imaging techniques, like CT and MRI, also face challenges in standardising lymph node assessment. Despite these limitations, accurate staging, particularly of lymph node involvement, is critical for treatment planning. The eighth edition of TNM provides detailed guidelines for measuring lymph node metastases, aiming to enhance consistency in assessment. The presence of lymph node metastases significantly influences cancer management decisions, particularly in identifying candidates for neoadjuvant chemotherapy. To improve radiologic evaluation, Elsholtz et al introduced Node-RADS, a scoring system based on size and configuration criteria, initially developed for various cancers but not yet extensively studied in breast cancer. This study recently published in European Radiology aims to fill this gap by retrospectively reviewing preoperative CE-MRI scans from breast cancer patients, assessing Node-RADS scores' potential to predict lymph node invasion.
CE-MRI and Node-RADS Evaluation in Predicting Lymph Node Involvement in Breast Cancer
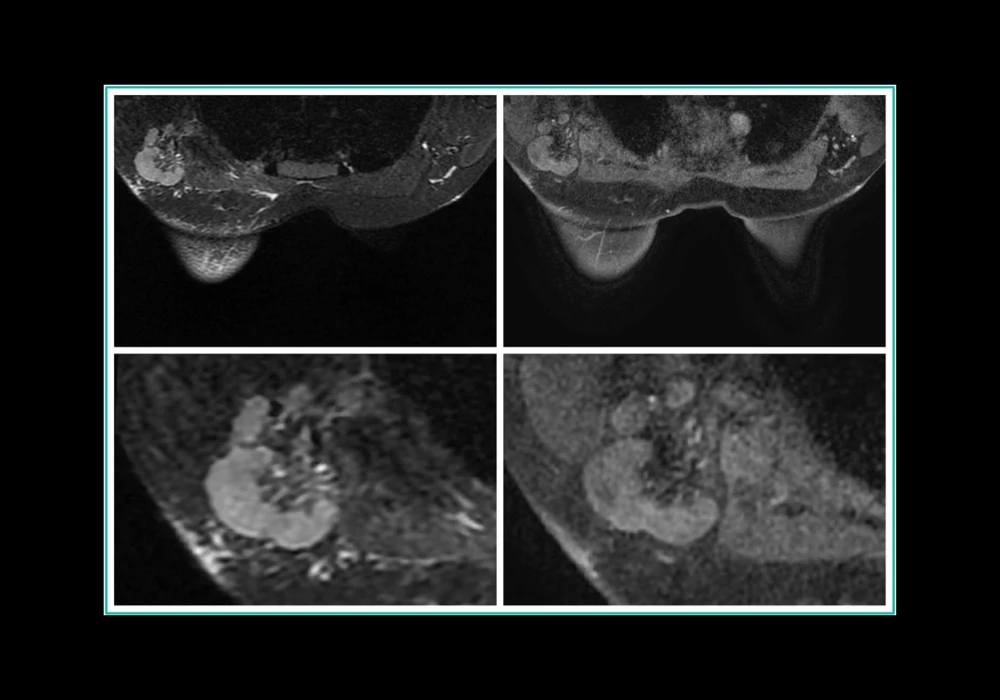
This retrospective study focused on patients diagnosed with invasive breast carcinoma or high-risk DCIS, who underwent preoperative CE-MRI, breast surgery, and lymphadenectomy at a single institution from January 2020 to July 2023. Patients receiving neoadjuvant therapy preoperatively were excluded. The study utilized a specialized CE-MRI protocol involving 3-T MRI with specific sequences for imaging enhancement and lymph node assessment. Three experienced radiologists independently evaluated the images using Node-RADS criteria, which categorize lymph nodes based on size and configuration into a score indicating the likelihood of metastasis. Axillary lymph nodes were assessed anatomically, including supraclavicular and internal mammary nodes, though the surgical focus was on level-I and level-II axillary nodes. Pathological examination of lymph nodes categorized findings as benign, micrometastasis, or macrometastasis. The study aimed to correlate Node-RADS scores from CE-MRI with pathological results to assess predictive accuracy in determining lymph node involvement.
Insights from a Single-Institution Study
The study included 192 female breast cancer patients selected from a total of 1553 who underwent preoperative CE-MRI between January 2020 and July 2023. Exclusions were made based on incomplete imaging data or missing documentation, resulting in a median age of 56 years for the eligible patients. Surgical procedures predominantly involved quadrantectomy (80.21%) over mastectomy (19.79%). Histological analysis of surgical specimens revealed various breast cancer subtypes, including luminal A, luminal B HER-, luminal B HER2+, HER2−, and triple-negative cases. A total of 1134 lymph nodes were surgically removed, with 372 (32.8%) showing metastatic involvement (221 macrometastatic and 151 micrometastatic). The overall rate of lymph node invasion (LNI) was 49% among the studied population.
The study evaluated the Node-RADS scoring system's diagnostic performance across three experienced readers, showing significant association between Node-RADS scores and LNI (p < 0.001). Receiver operating characteristic (ROC) analysis indicated high area under the curve (AUC) values for all readers (0.93-0.97), suggesting strong predictive capability. By adjusting Node-RADS cut-offs, specificity and positive predictive value (PPV) increased substantially while sensitivity and negative predictive value (NPV) decreased. Logistic regression confirmed Node-RADS as an independent predictor of LNI after adjusting for age and cT stage. Inter-reader agreement for Node-RADS scoring was substantial to excellent across different cut-off subclasses, as measured by Cohen’s Kappa.
Overall, the study underscores Node-RADS as a robust tool for predicting lymph node involvement in breast cancer patients undergoing CE-MRI evaluation, supported by strong inter-reader agreement and significant diagnostic accuracy metrics.
Node-RADS: Enhancing Predictive Accuracy for Lymph Node Involvement in Breast Cancer Imaging
This study highlighted a strong correlation between Node-RADS scores and lymph node invasion in breast cancer patients. A Node-RADS score > 2 was identified as the optimal threshold for predicting lymph node involvement, with scores of 3, 4, or 5 indicating a high likelihood of metastatic disease. This information is crucial for guiding patient management decisions, including the consideration of further diagnostic procedures such as ultrasound-guided biopsy for higher Node-RADS scores before surgery.
Lymph node involvement is a critical prognostic factor in breast cancer, significantly impacting disease-free and overall survival rates. Current methods for evaluating lymph nodes, primarily ultrasound, are specific but lack standardized criteria, contributing to variability in assessments. Cross-sectional imaging modalities like CT and CE-MRI also face challenges in accurately defining lymph node involvement.
The TNM staging system remains fundamental in breast cancer management, providing a baseline risk assessment at diagnosis and after surgery. Despite recent updates enhancing the precision of lymph node measurement, there is still no standardised scoring system for diagnosing lymphadenopathy through imaging.
Node-RADS, introduced to address this gap, has shown promise in various cancers by improving diagnostic accuracy and facilitating consistent radiological reporting. In this study, Node-RADS demonstrated significant utility in predicting lymph node involvement independently of other variables. Its ability to establish different cut-off values enhances its clinical applicability, particularly in distinguishing benign from malignant lymph nodes.
Inter-reader agreement among radiologists was substantial, supporting the reliability and reproducibility of Node-RADS scores across different clinical scenarios. However, the study's retrospective design and relatively small cohort size suggest the need for further validation in larger, more diverse populations to confirm its robustness.
Node-RADS represents a valuable tool for evaluating regional lymph nodes in breast cancer patients undergoing surgical treatment. It offers a standardised approach to assessing lymph node status, aiding in personalised treatment decisions and potentially reducing unnecessary procedures. Continued research and validation are essential to fully establish its role in clinical practice and enhance its impact on patient care.
Source & Image Credit: European Radiology