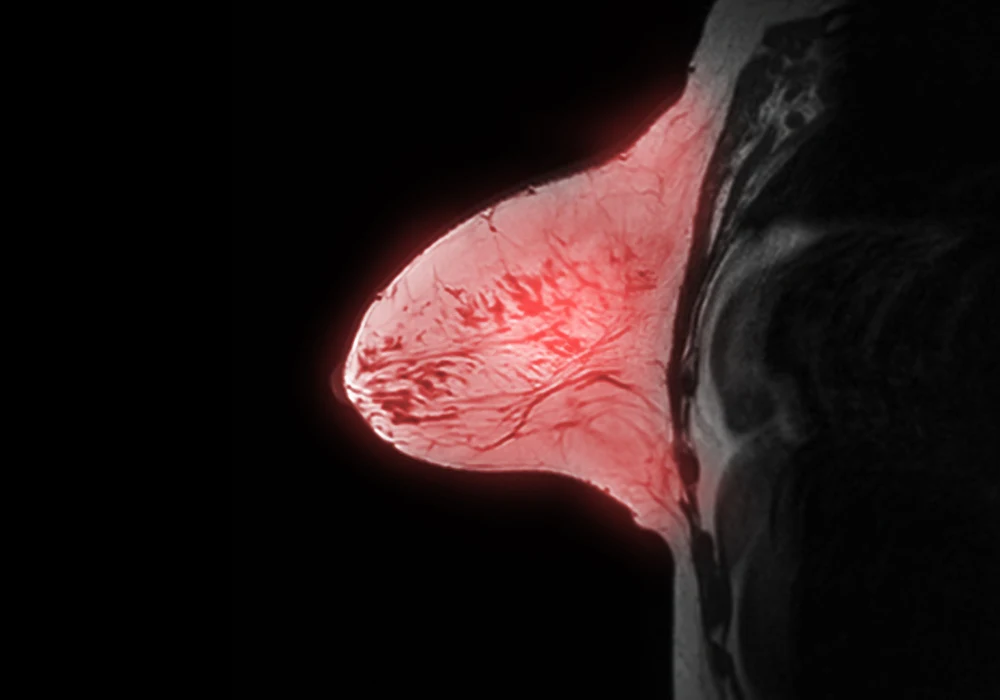
Magnetic resonance imaging (MRI) offers high sensitivity in detecting breast cancer, especially among women at elevated risk. However, the method’s effectiveness is hindered by high false-positive rates, which increase workload and anxiety while reducing efficiency. Artificial intelligence has been proposed as a solution, but existing models often fail to perform well in low-prevalence populations and lack interpretability. A fully convolutional data description (FCDD) anomaly detection model has been developed to address these challenges, aiming to improve accuracy and explainability in both high- and low-prevalence breast MRI screening contexts.
Addressing Limitations of Conventional Models
Most prior AI models for breast MRI have been evaluated using balanced datasets that do not reflect real-world prevalence, where malignant findings are rare. Such conditions tend to inflate performance metrics and reduce applicability in clinical settings. Additionally, binary classification approaches often struggle with the heterogeneity of malignant lesions, including variation in type, size and histological characteristics, which are frequently underrepresented in datasets. These models also tend to produce saliency maps of limited accuracy, hampering trust and clinical adoption.
Anomaly detection offers a different approach by focusing on learning the characteristics of normal breast MRI scans, enabling better identification of abnormalities even when malignant cases are scarce. The FCDD model applies this principle to dynamic contrast-enhanced MRI data, generating pixel-level anomaly scores that can be aggregated into breast-level predictions. This method avoids reliance on secondary interpretability techniques and does not require lesion annotations, allowing for more direct and robust heat maps of suspected malignancy.
Must Read: Shortening Breast MRI Time Without Missing Cancer
Methodology and Evaluation
The model was developed using 9567 MRI examinations from 5026 patients collected over a decade, with two defined detection tasks: a balanced scenario including all cases and an imbalanced scenario reflecting realistic cancer prevalence. Internal testing employed a separate set of 171 examinations, and external validation used a multicentre public dataset of 221 examinations. Imaging was processed into maximum intensity projections (MIPs), separated by breast and analysed using the FCDD model alongside comparison models, including binary cross-entropy (BCE) classification and hypersphere classification (HSC).
Performance metrics included the area under the receiver operating characteristic curve (AUC), area under the precision-recall curve (AUPR), specificity, sensitivity and positive predictive value (PPV). Explainability was measured through pixelwise agreement with radiologist-provided reference annotations. Statistical significance was determined with the Wilcoxon signed-rank test.
Across both balanced and imbalanced detection tasks, FCDD consistently outperformed BCE in AUC and AUPR, while HSC showed similar performance to FCDD in some scenarios. At operating points prioritising high sensitivity, FCDD achieved higher specificity, indicating a capacity to reduce false positives. In the imbalanced detection setting, its PPV was double that of BCE. Heat maps generated by FCDD exhibited significantly greater alignment with radiologist annotations than those from comparison models, suggesting stronger localisation of suspicious areas.
Key Findings and Clinical Implications
The model demonstrated generalisability, maintaining strong performance on the external multicentre dataset without retraining. Balanced detection AUC reached 0.86, surpassing both HSC and BCE. Explanation maps showed superior spatial accuracy and specificity, supporting their potential use in assisting radiologists during interpretation. Although pixelwise performance was lower for nonmass enhancements and in situ cancers—likely due to their subtler imaging features—FCDD performed well across most lesion types and stages.
By reducing false positives and offering interpretable outputs, the model could serve as a triage tool, rapidly excluding normal scans and directing radiologist attention to regions of concern. This capability may improve efficiency, particularly in screening programmes where the majority of cases are normal. The heat maps also act as a form of visual validation, helping radiologists assess the reliability of AI suggestions.
In scenarios with realistic cancer prevalence, FCDD’s higher PPV and reduced false positives could translate to fewer unnecessary follow-ups, lowering patient anxiety and healthcare costs. The approach aligns with trends in AI adoption that emphasise transparency and clinician oversight rather than opaque decision-making systems.
The fully convolutional data description anomaly detection model represents a significant step forward in breast MRI screening, addressing both the performance drop seen in low-prevalence settings and the interpretability gap of prior AI approaches. It demonstrated superior detection accuracy, robust generalisability and explanation maps closely matching radiologist annotations. While further validation in larger, lesion-annotated datasets and prospective clinical trials is needed, the model shows promise for enhancing breast MRI workflows, reducing false positives and improving diagnostic confidence.
Source: Radiology
Image Credit: iStock