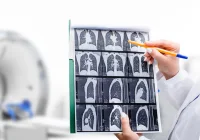
Low-dose computed tomography (LDCT) has emerged as a vital tool for lung cancer screening, particularly for individuals with a high risk due to tobacco use. While its primary aim is to detect early-stage lung cancer and reduce mortality, LDCT also frequently reveals incidental findings unrelated to lung cancer. These findings can both enhance early diagnosis of other conditions and create potential for overdiagnosis and increased healthcare burden. A large-scale study conducted between 2016 and 2021 across Australian and Canadian sites as part of the International Lung Screen Trial (ILST) sought to assess the type and frequency of such incidental findings, as well as the consistency of their clinical reporting. The study’s findings provide critical insights as Australia prepares to implement a national lung cancer screening programme.
High Frequency of Incidental Findings
The study enrolled over 4400 participants across five Australian and one Canadian site, all of whom were aged 55–80 years and had significant smoking histories. Baseline LDCT scans revealed at least one incidental finding in nearly 73% of participants, with 10.3% requiring clinical follow-up. The most common incidental findings included coronary artery calcification and emphysema, both highly prevalent in individuals with a history of smoking. Interestingly, most participants with these findings reported no prior diagnosis of related conditions such as chronic obstructive pulmonary disease or coronary artery disease, suggesting LDCT’s potential for revealing previously undetected health risks.
Must Read: The Challenge of Incidental Findings in LDCT
Marked geographic differences were observed, with 16.7% of Australian participants versus only 4.5% of Canadian participants having incidental findings deemed to require clinical follow-up. These disparities were attributed to both variations in smoking history and differences in radiology reporting practices. Canadian results were generated by a single radiologist, while several radiologists contributed reports in Australia. This variability underlines the influence of local practices on clinical decision-making and points to the need for standardisation.
Inconsistency in Clinical Reporting
One of the most striking observations from the study was the inconsistency in how incidental findings were reported to treating physicians. The researchers reviewed clinical reports from two Australian sites and found significant variation in how and whether findings were mentioned. For instance, only 12% of cases of radiological emphysema were flagged as requiring action, even though more severe findings were more likely to be included in the report conclusion. Similarly, severe coronary artery calcification was mentioned in only 46% of cases within report conclusions, leaving room for undercommunication of potentially serious issues.
Findings related to thyroid abnormalities, liver issues, vertebral fractures and other organ systems were also inconsistently reported, with some clinically actionable conditions omitted entirely. These discrepancies reflect a lack of clear guidance and standardisation, leading to subjective decision-making by radiologists. The absence of a unified template or protocol for clinical communication may result in missed opportunities for timely intervention or, conversely, unnecessary investigations.
Implications for Screening Programmes and Policy
The findings carry significant implications for the design and operation of national lung cancer screening programmes, especially as Australia prepares to launch its own. Standardising the reporting of incidental findings through structured templates could improve clarity and consistency in clinical communication. International models such as the Lung–RADS S classification and European guidelines already advocate for such practices, emphasising the inclusion of concise management recommendations in screening reports.
Moreover, the study highlighted how incidental findings can both inform better care and increase resource demands. While identifying undiagnosed emphysema or coronary calcification could prompt beneficial interventions, unstructured reporting and unclear clinical pathways may lead to overburdened primary care providers and unnecessary anxiety for patients. A thoughtful balance is needed, where only clinically significant findings are communicated, and appropriate care pathways are defined.
Tailoring recommendations to local healthcare infrastructure is equally important. For example, moderate to severe emphysema might warrant respiratory referral in one setting, while in another, primary care follow-up may suffice. Engaging primary care providers in the design of screening pathways can help ensure feasibility and adherence to guidelines. Further, transparency with patients about the possibility of incidental findings may help manage expectations and foster informed participation in screening.
As low-dose computed tomography becomes a cornerstone of lung cancer screening, understanding and managing incidental findings is essential to maximise benefit and minimise harm. The ILST substudy conducted in Australia and Canada reveals a high prevalence of incidental findings and a lack of uniformity in their clinical reporting. These insights underscore the necessity for structured reporting protocols, informed by local context and international best practice, to guide the implementation of Australia’s forthcoming national screening programme.
Source: The Medical Journal of Australia
Image Credit: iStock