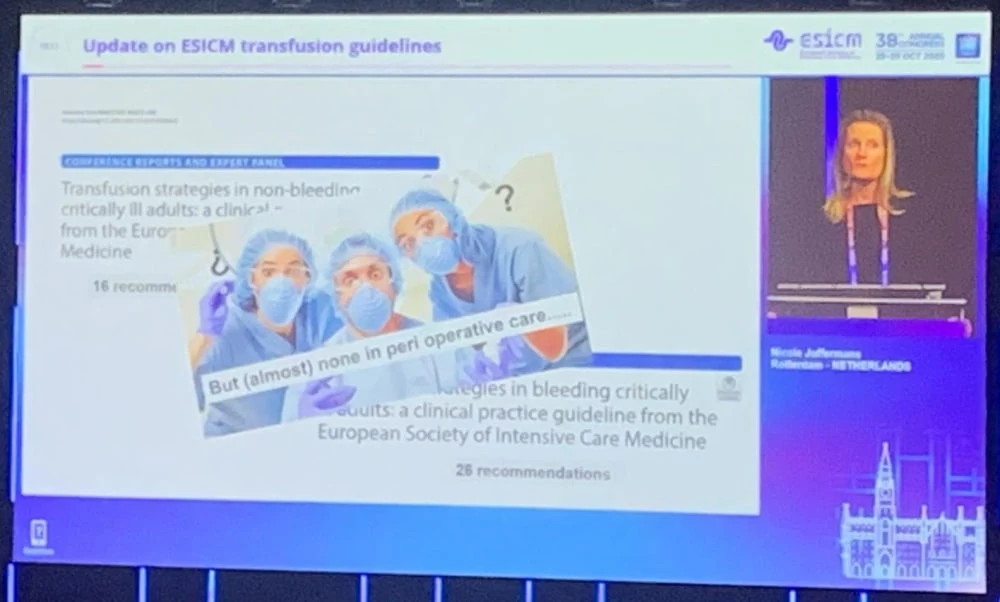
At #LIVES2025, Nicole Juffermans, Professor of Translational Intensive Care Medicine at the University of Amsterdam Faculty of Medicine, provided an update on ESICM transfusion guidelines.
While transition guidelines from 2020 and 2021 provided recommendations for transfusion practices, the perioperative setting has remained largely without updates. However, recent large trials have shed new light on transfusion thresholds for patients with specific conditions, particularly those with cardiac and neurological morbidities.
The body employs several mechanisms to compensate for anaemia. Most tissues increase their oxygen extraction ratio, stimulate endogenous haemoglobin production, and become more efficient with available oxygen. The heart compensates by increasing heart rate and contractility to produce greater cardiac output.
However, the heart is uniquely vulnerable during anaemia for two reasons. First, unlike other tissues, the myocardium operates at near-maximal oxygen extraction at all times and cannot increase this ratio further. Second, the compensatory mechanisms that increase cardiac output simultaneously increase the heart's own oxygen consumption, creating a precarious balance.
For cardiac surgery, the 2020 guidelines strongly recommended a restricted transfusion threshold of 7.5 g/dL. However, for acute coronary syndrome, recommendations showed more variability and uncertainty.
The REALITY trial with approximately 700 patients with acute myocardial infarction compared transfusion triggers of 8 g/dL versus 10 g/dL. The trial was designed as a non-inferiority study, meaning both strategies should prove equally effective. Surprisingly, the liberal group (10 g/dL trigger) experienced more major cardiovascular ischaemic events, contradicting expectations.
Five times larger than REALITY, the MINT trial enrolled 3,500 patients with acute coronary syndrome and used the same comparison of 8 g/dL versus 10 g/dL triggers. The practical implications are significant: a liberal strategy of 10 g/dL would mean transfusing virtually all patients, while a restrictive threshold of 8 g/dL would dramatically reduce transfusion rates.
The primary composite outcome of myocardial infarction or death showed that patients receiving restrictive transfusion had fewer adverse events. All subgroup analyses pointed in the same direction, with restricted transfusion showing benefits across multiple outcomes, including myocardial death, heart failure, and revascularisation needs.
Two subgroups showed unexpected results. Patients with type 1 myocardial infarction and those with heart failure appeared to benefit from a liberal transfusion strategy, contrary to the overall trend.
The heart compensates for anaemia primarily through coronary vasodilation. When obstructive coronary disease prevents this mechanism, restricting transfusion may drive the heart toward ischaemic complications and cardiac death.
Sub-analyses of the MINT trial supported this physiological model. Patients with type 1 myocardial infarction had worse outcomes with restrictive transfusion and experienced more cardiac deaths. Similarly, patients who did not undergo revascularisation benefited from liberal transfusion, as they retained their coronary obstruction.
The explanation appears to be that type 1 MI patients, with their higher incidence of cardiac death, need the additional oxygen-carrying capacity that liberal transfusion provides when coronary vasodilation is compromised.
The same logic applies to heart failure patients who cannot increase cardiac output through enhanced contractility. A MINT sub-analysis comparing patients with ejection fractions below 45% to those with normal function found that heart failure patients benefited from liberal transfusion, while those with normal heart function showed no difference between strategies.
It's important to note that heart failure patients in this analysis were older and had more comorbidities, including kidney injury and hypertension, which may have influenced results.
While the 2020 guidelines provided clear recommendations for sepsis, weaning, and oncology patients (generally 7 g/dL), significant uncertainty remained for patients with acute brain injury.
The healthy brain compensates for anaemia by increasing cerebral blood flow through vasodilation, similar to the heart. However, as anaemia becomes severe, oxygen extraction must increase. In injured brains, this vasodilatory capacity is severely diminished due to lower vessel density in damaged areas, making the brain more dependent on oxygen extraction, which may also be impaired.
Three trials have examined liberal versus restrictive transfusion in brain injury:
HEMOTION Study (Traumatic Brain Injury): Compared triggers of 7 g/dL versus 10 g/dL using neurological outcome scales. The liberal group showed a 5.4% reduction in poor neurological outcomes, though this fell short of the pre-specified 10% threshold for statistical significance.
TRAIN Study (Traumatic Brain Injury): Compared 7 g/dL versus 9 g/dL with similar outcome measures. The liberal group achieved a statistically significant reduction in poor outcomes.
Subarachnoid Hemorrhage Study: Compared 8 g/dL versus 10 g/dL, finding a 4.5% reduction in poor outcomes with liberal transfusion, though not reaching statistical significance. This group also experienced less new ischaemia and less vasospasm.
While two trials did not reach statistical significance, the trialists argue that all point estimates consistently favour liberal transfusion, and a 5% reduction in poor neurological outcomes represents a clinically meaningful improvement from a patient perspective. They also note that adverse outcomes were consistently lower with liberal strategies.
Based on current evidence, potential guideline updates could include:
- Type 1 myocardial infarction: Consider liberal transfusion threshold
- Patients not undergoing revascularization: Liberal transfusion threshold
- Heart failure patients: Liberal transfusion threshold
- Type 2 myocardial infarction: Maintain restrictive threshold of 8 g/dL
For patients with acute brain injury, including traumatic brain injury and subarachnoid haemorrhage, evidence supports transitioning to a more liberal threshold of 9 g/dL. This recommendation may reasonably extend to patients with other forms of acute brain damage.
The landscape of transfusion medicine continues to evolve as new evidence emerges. While restrictive transfusion strategies remain appropriate for many patients, specific subgroups, particularly those with compromised coronary vasodilation or acute brain injury, appear to benefit from more liberal approaches. The key is understanding the underlying physiology and recognising which patients lack the compensatory mechanisms necessary to tolerate anaemia safely.
Source & Image Credit: ESICM