Young people are often told by their parents or guardians not to give in to peer pressure. Interestingly, a recent study showed that social or peer pressure might be the key to boosting hand-hygiene adherence in hospitals. Results of the study have been published in Infection Control and Hospital Epidemiology.
Researchers from the University of Iowa's Carver College of Medicine (USA) devised an automated hand-hygiene monitoring system to observe healthcare staff in a 20-bed medical intensive care unit (ICU) at a large university hospital. The system detected whether healthcare workers washed their hands on entering and exiting a patient's room. It also determined the location of other healthcare workers with respect to the workers coming into or out of room.
According to authors, they identified 47,694 hand-hygiene opportunities for a 10-day period. Their key findings include:
The authors explained that compliance could be higher since the numbers recorded by the automated monitoring system did not include dispensing events inside the patient's room.
In addition, researchers observed that compliance increased with the number of nearby healthcare workers, leading them to conclude that presence and proximity of co-workers was associated with higher hand-hygiene adherence rates.
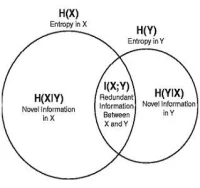
"Our results speak to the importance of the social environment in healthcare," the authors said, and "may have implications for disease modelling, a field that is increasingly stressing the importance of human behaviour on the spread of diseases."
Hospitals Taking Proactive Approach
More and more hospitals have taken a proactive approach to hand-hygiene compliance, FierceHealthcare reported. For example, MetroHealth Medical Center in Cleveland (OH, USA) hired four hand-washing monitors, whose job was to track who washed their hands as they stepped in and out of patient rooms. After this initiative, ventilator-associated pneumonia fell 71 percent, surgical site infections decreased by 64 percent, and central line-associated bloodstream infections dropped 35 percent. In addition, hospital-acquired infections at MetroHealth as a whole fell 38 percent.
The hand-washing campaign started in 2010 after a bacterial infection spread from patient to patient, and the hospital experienced a problem with the antibiotic-resistant organism Acinetobacter baumannii, said Al Connors, MetroHealth's chief medical officer. "People were good at coming up with excuses why they didn't need to wash hands," Connors noted. "But when you walk into a patient's room, you never know what's going to happen."
Source: FierceHealthcare.com
Image Credit: Flickr.com
Researchers from the University of Iowa's Carver College of Medicine (USA) devised an automated hand-hygiene monitoring system to observe healthcare staff in a 20-bed medical intensive care unit (ICU) at a large university hospital. The system detected whether healthcare workers washed their hands on entering and exiting a patient's room. It also determined the location of other healthcare workers with respect to the workers coming into or out of room.
According to authors, they identified 47,694 hand-hygiene opportunities for a 10-day period. Their key findings include:
- When a healthcare worker was alone, the observed adherence rate was 20.85 percent;
- When other healthcare workers were nearby, the adherence rate was higher at 27.9 percent; and
- Adherence was slightly higher at night and higher among nurses than doctors.
The authors explained that compliance could be higher since the numbers recorded by the automated monitoring system did not include dispensing events inside the patient's room.
In addition, researchers observed that compliance increased with the number of nearby healthcare workers, leading them to conclude that presence and proximity of co-workers was associated with higher hand-hygiene adherence rates.
"Our results speak to the importance of the social environment in healthcare," the authors said, and "may have implications for disease modelling, a field that is increasingly stressing the importance of human behaviour on the spread of diseases."
Hospitals Taking Proactive Approach
More and more hospitals have taken a proactive approach to hand-hygiene compliance, FierceHealthcare reported. For example, MetroHealth Medical Center in Cleveland (OH, USA) hired four hand-washing monitors, whose job was to track who washed their hands as they stepped in and out of patient rooms. After this initiative, ventilator-associated pneumonia fell 71 percent, surgical site infections decreased by 64 percent, and central line-associated bloodstream infections dropped 35 percent. In addition, hospital-acquired infections at MetroHealth as a whole fell 38 percent.
The hand-washing campaign started in 2010 after a bacterial infection spread from patient to patient, and the hospital experienced a problem with the antibiotic-resistant organism Acinetobacter baumannii, said Al Connors, MetroHealth's chief medical officer. "People were good at coming up with excuses why they didn't need to wash hands," Connors noted. "But when you walk into a patient's room, you never know what's going to happen."
Source: FierceHealthcare.com
Image Credit: Flickr.com
Latest Articles
bacterial infections, hand hygiene, hand washing, intensive care unit
Young people are often told by their parents or guardians not to give in to peer pressure. Interestingly, a recent study showed that social or peer pressur...