ICU Management & Practice, Volume 24 - Issue 5, 2024
Shortening the weaning process of children receiving non-invasive ventilation (NIV) is challenging. We present the results of implementing a nurse-guided weaning protocol in our PICU.
Introduction
Given the low mortality rate in paediatrics, the management of acute respiratory insufficiency with non-invasive support has improved the variables resulting from the duration of ventilatory support and length of stay in the Paediatric Intensive Care Unit (PICU). Some studies estimate a 2-day shortening in adults.
The weaning of the support can account for 40% of the time in mechanical ventilation (MV) in the intubated patient. Despite not having data concerning patients in non-invasive ventilation (NIV), it is possible that different strategies for weaning from NIV have an influence on the variables mentioned above.
MV protocols guided by doctors/nurses/physiotherapists exist. These protocols have a positive influence on shortening patient time in MV. The literature lacks descriptions of NIV weaning protocols in children. In both adults and paediatrics, we have not found published protocols of treatment in nursing-driven NIV weaning.
The weaning strategies are not very detailed either. The existing bibliography recommends some progressive reduction of parameters, other intermittent rests of the NIV support, or even the mixing of options. The objectives and criteria for restarting ventilatory support are rarely explained.
In recent years, the introduction of high-flow oxygen therapy (HFNC) in the initial management of the hypoxaemic patient has been followed by its incorporation in the weaning process of the intubated patient and the weaning of the NIV. Studies in adults don’t show different intubation rates of HFNC compared to NIV. There is data against HFNC effectiveness in weaning in paediatrics. Some data from neonatal unit studies suggest an increase in stay without alternative advantages after introducing HFNC. A recent systematic review of preterm babies failed to show the benefits of weaning to HFNC compared to directly removing CPAP.
In paediatrics, we do not have data that suggests the need for bilevel weaning to necessarily involve a step by step support in CPAP and even less the step to HFNC, despite this being a routine rapidly becoming widespread in many centres. This lack of protocolisation or the inclusion in the routine of the HFNC pass may imply an extension of stays in the critical care units.
This led us to develop a protocol for NIV weaning five years ago, which gives nursing staff a decision-making capacity for frequent pathologies in uncomplicated patients.
Protocol Description
This protocol for NIV weaning was designed for paediatric patients suffering from acute respiratory failure without underlying conditions, so mainly bronchiolitis, pneumonia, and asthma diagnoses. Patients receiving palliative care, previous home ventilation, affected by neuromuscular disease or diaphragmatic palsy, airway obstruction, or underlying cardiac disease were excluded.
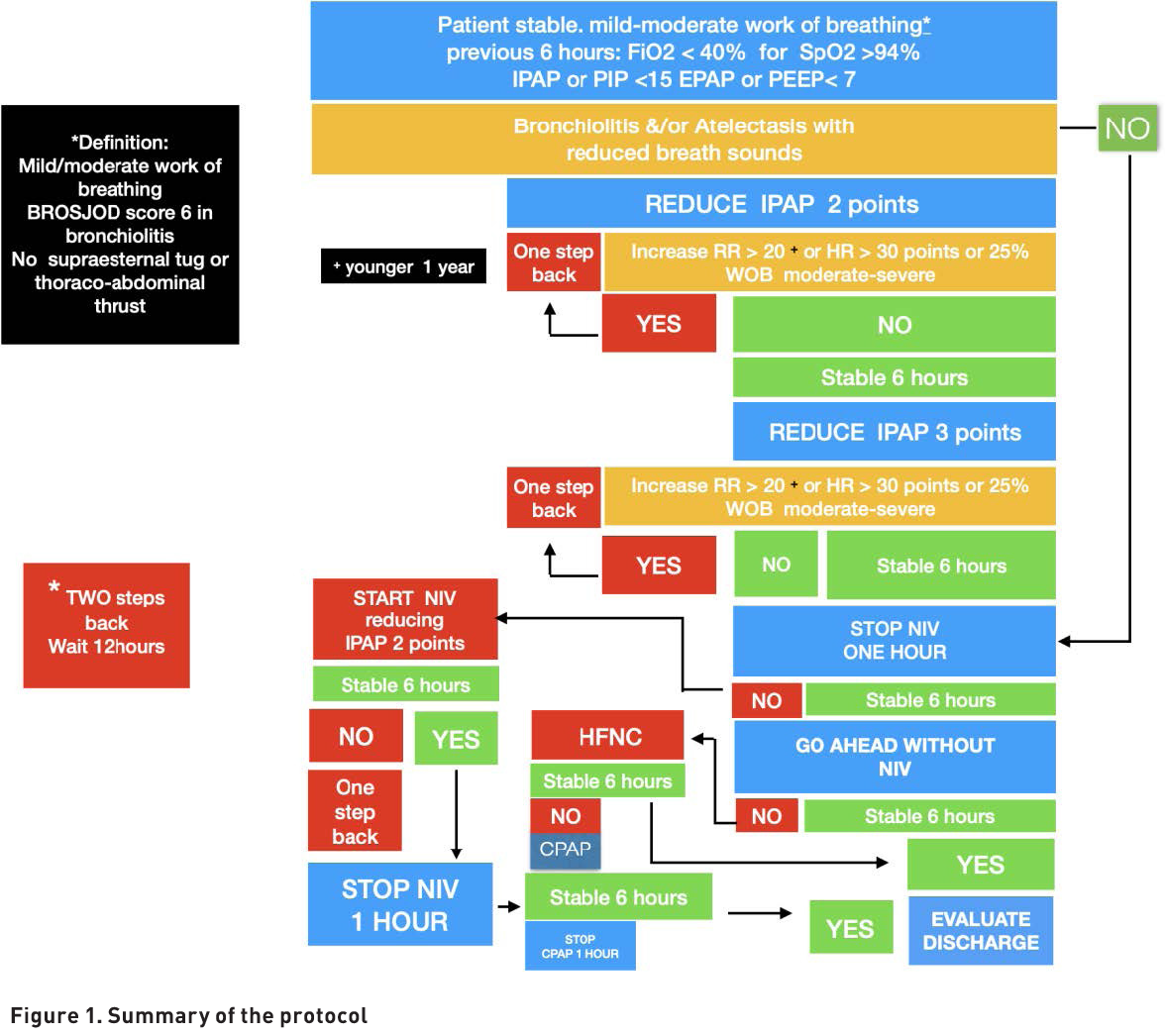
The starting point of weaning was considered after 24 hours of stabilisation when the patient fulfilled these criteria (IPAP inferior to 16 cm H2O, EPAP inferior to 7 cm H2O, FiO2 inferior to 0.4) for at least six hours (Figure 1).
This starting point was agreed upon due to previous clinical experience in the unit, which involved safely extubating most intubated patients to low-flow oxygen from these values.
Nurses were authorised to start and follow the protocol spontaneously in patients fulfilling inclusion criteria. A progressive reduction of IPAP was considered in patients with remaining atelectasis, like those with bronchiolitis. In patients with a low risk of de-recruiting, mainly asthma patients without significant atelectasis, it was possible to do a straightforward one-hour trial without NIV. Clear criteria for weaning failure were established, and how to proceed accordingly.
The main objectives were to confirm the protocol's safety and evaluate its impact on the length of stay in the PICU. A secondary objective of the study was to reduce the use of HFNC after removing NIV.
Results of Protocol Implementation
To evaluate the protocol implementation, a comparative study was performed on admitted patients in the PICU requiring NIV support due to acute respiratory failure during the implementation period (20.12.2019 to 31.03.2020) of the nurse-driven weaning protocol and the same period of the previous year.
The weaning protocol was implemented in 28 patients out of 59 during the study period. In the previous year, 88 patients received NIV without a planned weaning. So, we could compare the data of 119 non-protocolised patients to the data of 28 protocolised patients.
No significant clinical differences in age, respiratory, or heart rate were observed at the initiation of the protocol. The main results regarding safety were evaluated by measuring reintubation and readmission in the PICU during the first 24 hours due to respiratory failure. Zero reintubations and zero readmissions were observed. The setback percentage was 18% (5/28) in the protocolised group compared to 6% (21/119) in the non-protocolised group.
Efficiency was measured by comparing hours of treatment with NIV support and days of admission in the PICU and Hospital. The duration of NIV support was shortened by an average of 14 hours (52 to 38 hours), and the length of stay in the PICU was shortened by 21 hours. Hospital admission was also reduced by 3.8 days in the protocolised group. Although none of these data reached statistical significance, the trend supports a beneficial impact.
The use of HFNC didn't change between the two groups, around 60%; however, there was a statistically significant reduction of time (seven hours) in the PICU since HFNC was started after the protocol implementation.
Discussion
This study shows potential benefits; however, the small sample suggests caution with the results. Considering the limited sample, we would like to highlight that the protocol seems safe if strictly applied, and a potential early discharge from the PICU is not increasing readmissions. Additionally, all the data show positive clinical trends without reaching statistical significance.
As we observed, an active weaning protocol may increase the percentage of setbacks. Therefore, the protocol was modified, and patients having two or more setbacks should remain stable for 12 hours before restarting the weaning protocol.
Although the protocol does not reduce the use of HFNC, patients stable on HFNC are rapidly discharged after seven hours to the general ward without observing negative side effects.
The protocol implementation was below 50%. Several barriers were detected among the healthcare staff: doctors reluctant to give permission, nurses afraid of taking responsibility, and a nurse-patient ratio of 1:2. Ongoing training every year before the winter season has been introduced to address these problems and improve adherence.
Conclusion
Implementing a structured weaning protocol led by nurses or respiratory therapists may help shorten the length of ventilatory support and the length of the PICU stay in children without underlying conditions requiring NIV support.
Conflict of Interest
None.
References:
Balhareth Y, Razak A (2024) High Flow Nasal Cannula for Weaning Nasal Continuous Positive Airway Pressure in Preterm Infants: A Systematic Review and Meta-Analysis. Neonatology. 121(3):359-369.
Cassibba J, Freycon C, Doutau J et al. (2023) Weaning from non-invasive ventilatory support in infants with severe bronchiolitis: An observational study. Arch Pediatr. 30(4):201-205.
Loberger JM, Jones RM, Prabhakaran P (2020) A Respiratory Therapist-Driven Pathway Improves Timeliness of Extubation Readiness Assessment in a Single PICU. Pediatr Crit Care Med. 21(8):e513-e521.
Ramnarayan P, Richards-Belle A, Drikite L et al. (2022) Effect of High-Flow Nasal Cannula Therapy vs Continuous Positive Airway Pressure Following Extubation on Liberation From Respiratory Support in Critically Ill Children: A Randomized Clinical Trial. JAMA. 327(16):1555-1565.
van Delft B, Van Ginderdeuren F, Lefevere J et al. (2020) Weaning strategies for the withdrawal of non-invasive respiratory support applying continuous positive airway pressure in preterm infants: a systematic review and meta-analysis. BMJ Paediatr Open. 4(1).
Wang Q, Peng Y, Xu S et al. (2023) The efficacy of high-flow nasal cannula (HFNC) versus non-invasive ventilation (NIV) in patients at high risk of extubation failure: a systematic review and meta-analysis. Eur J Med Res. 28(1):120.















