ICU Management & Practice, Volume 20 - Issue 4, 2020
The Post Intensive Care Syndrome (PICS): Definition and Prevalence
There is more to life than measuring death.
At first, there was only survival or death. Critical care is a relatively new branch of medicine that emerged in the 1950s during the large polio epidemic in Northern Europe. For decades, the primary objective of intensive care was to save as many lives as possible, regardless of the severe disabilities that could ensue and then weigh on the residual life of the patients. In the 1970s, though, critical care outcomes after ICU discharge have increasingly reported. Particularly significant is a 1976 article ("Survival, hospitalisation costs, and follow-up results in critically ill patients") published in NEJM (Cullen et al. 1976) about 1-year follow-up outcomes of ICU survivors. The article described a novel approach to treatment in ICU, more focused also on post ICU outcomes. In this study on 226 critically ill survivors, the one-year mortality rate was as high as 73%. Moreover, only 42% of the one-year survivors had the same functional level as before, while 16% had a partial recovery and were in a nursing home. Cullen et al. (1976) also demonstrated, as expected, a profound negative effect of age (≥65 years) on survival and long-term cognitive decline. It is noteworthy that this first comprehensive analysis on outcomes related to post-discharge items revealed many problems that ICU survivors still have to deal with today (Cullen et al. 1976). Since then, our awareness on long-term sequelae increased and in the 2012 the concept of post intensive care syndrome (PICS) was established to indicate the overall chronic disabilities that plague ICU survivors and their caregivers (PICS-Family) (Rawal et al. 2017).
Current evidence shows that this syndrome can affect up to 50% of patients discharged from ICU. Cognitive impairments of different grade of severity and duration occur in up to 30-80% of ICU survivors (Harvey and Davidson 2016; Pandharipande et al. 2013). Psychiatric disorders, such as anxiety, depression, or post-traumatic stress disorder (PTSD) often lasting for years can occur in 8-57% of patients (Harvey and Davidson 2016). A new physical disability can also be developed by 25-80% of patients (Griffiths et al. 2013), and new symptoms such as dyspnoea, pain, sexual dysfunction, or impaired exercise tolerance may be experienced as well.
PICS prevalence is also related to the admission diagnosis; among critically ill septic shock patients, PICS can reach 70% with long-term cognitive impairments observed more frequently than in post-surgical patients (Brück et al. 2018).
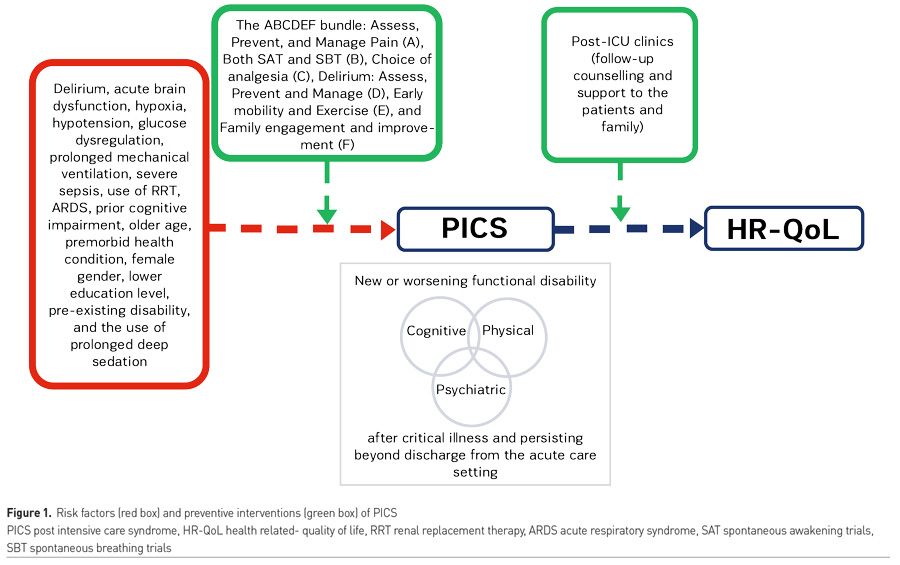
The ICU Patient Identikit: Risk Factors and Prevention Strategies
Broadening perspectives in daily practice.
Even though a growing number of reports on PICS occurrence and epidemiology are available, the risk factors and biologic mechanisms involved and the applicable preventive and treatment strategies have yet to be completely clarified.
As far as physical impairment is concerned, literature highlights the critical role of Intensive Care Unit-Acquired Weakness (ICU-AW). ICU-AW is defined as the acute muscle weakness of the extremities in a symmetric pattern, related to critical illness, which may be classified as critical illness polyneuropathy (CIP), critical illness myopathy (CIM), critical illness neuromyopathy (CINM), and muscle deconditioning (Latronico and Bolton 2011).
The incidence of ICU-AW is 40% in critically ill adult patients (Appleton et al. 2015), with CIP being the most common category (Bednarik et al. 2003). The physiopathological mechanism is multifactorial (Latronico): microvascular ischaemia, catabolism, and immobility can lead to skeletal muscle wasting, while microvascular injury with nerve ischaemia, dysfunction of sodium channels, and mitochondria injury could contribute to critical illness-related neuropathy, myopathy, or both. Risk factors for ICU-AW and consequently for long term physical impairment have been identified as female sex, sepsis, catabolic state, multiorgan failure, systemic inflammatory response syndrome (SIRS), long duration of mechanical ventilation (MV), immobility, hyperglycaemia, glucocorticoids, and neuromuscular blocking agents (Latronico and Bolton 2011).
Critically ill patients may experience not only physical stress but also psychological derangements. This type of stress may generate new cognitive impairments or worsen pre-existing conditions lasting months to years, resulting in a reduced quality of life (Wolters et al. 2013). Cognitive impairments include impaired memory, executive function, language, attention, and visual-spatial abilities. Hypoglycaemia, as well as hyperglycaemia, delirium, and other acute stress symptoms, have been identified as risk factors for persistent cognitive impairment (Hopkins et al. 2010; Pandharipande et al. 2013; Davydow et al. 2008). There is a strong evidence that patients with delirium are at greater risk of long-term adverse cognitive outcomes (Katz et al. 2001; Guerra et al. 2015).
Long ICU stays can represent a traumatising event. With regards to mental health, anxiety, depression, and Post Traumatic Stress Disorder (PTSD) are the most frequent psychiatric disorders observed in ICU survivors, respectively in 70%, 30%, and 10% (Davydow et al. 2008; Garrouste et al. 2012). The risk of PTSD after ICU care is higher for women. Other risk factors for acquired mental illness include pre-existing depression, anxiety, a lower education level, and alcohol abuse (Davydow et al. 2008).
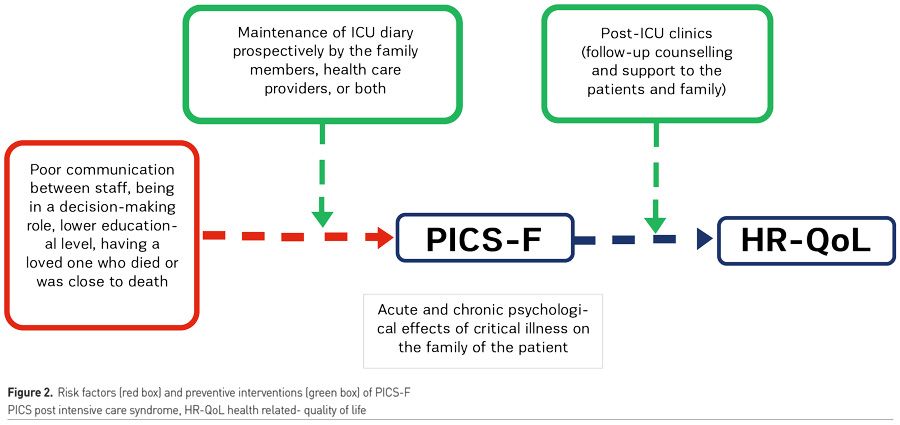
In daily clinical practice, preservation of health-related quality of life (HRQoL) must be routinely pursued. With this aim a bundle of intervention has been elaborated:
The ABCDE is the bundle for sedation, delirium, and immobility management in ICU patients. ABCDE is composed of:
A: Airway management, assessment, prevention, and management of pain;
B: Breathing trials, including daily interruptions of mechanical ventilation, spontaneous awakening trials and spontaneous breathing trials;
C: Choice of analgesia and sedation, coordination of care, and communication;
D: Delirium assessment, prevention, and management;
E: Early mobility and exercise.
The ABCDE bundle has been recently complemented with FGH for PICS prevention. FGH includes:
F: Family involvement, follow-up referrals;
G: Good handoff communication;
H: Handout materials on PICS and PICS-Family (Devlin et al. 2018).
Besides, guidelines focus on other strategies such as environmental management, nursing care, diary and, mostly, nutritional therapy, which has become a cornerstone for PICS prevention, especially for ICU-AW (Inoue et al. 2019). A proper nutritional strategy should target muscle volume and strength while avoiding overfeeding (McClave et al. 2016; Singer et al. 2018) that could induce autophagy and worsen ICU-AW (Casaer et al. 2013). Avoiding muscle catabolism and lean body mass loss through adequate energy delivery and protein intake (Phillips SM, Kim IY) has proven to reduce long-term mortality (Demling et al. 2009). While in healthy individuals muscle protein synthesis is maximised with exercise, in critically ill patients appropriate rehabilitation exercises, and adequate nutrition are both necessary (Morton et al. 2018).
The Post-ICU Patient Identikit. What Monitoring Tools?
The Post-ICU management: a new target for the intensivist.
Despite efforts in identifying risk factors and implementing prevention strategies, PICS remains underdiagnosed mainly due to:
• Lack of specific follow-up programmes
• Discharge documents focused exclusively on organ-specific damage: physical and/or cognitive deficits, possibly acquired or newly detected during hospitalisation, are usually not emphasised
•Lack of universally validated tools for PICS screening and diagnosis
While some categories of patients, e.g., stroke survivors or Chronic Obstructive Pulmonary Disease (COPD) patients, usually fall under a structured programme of rehabilitation because of their chronic diseases, ICU survivors suffering from PICS are not recognised as 'chronically ill’ and often do not have follow-up schemes.
Van der Schaaf et al. (2015) underlines that the optimal timing of first visit after ICU discharge are lacking in the literature (between 1 to 12 months after discharge). However, a panel of Dutch experts has suggested that the optimal timing is about 12 weeks after hospital discharge (Van Der Schaaf 2015). This period of time seems long enough to rule out all ICU survivors who face early hospital readmission or death. It also appears to be an adequate time period for any physical, cognitive, and psychological sequelae to emerge and be noticed by family members or caregivers and, therefore, be reported at the follow-up consultation as significant impairment for quality of life.
With reference to the duration of the follow up, some studies suggest up to 10 months after discharge for those patients who report sequelae related to ICU admission disease and up to 1 year for family members or caregivers who develop psychological repercussions from their family member’s experience (Griffiths et al. 2013).
Currently, organisational models are not univocal and different tools are adopted to measure physical, psychological, or cognitive disabilities. Some literature examples are the Modified Rankin Scale (MRS) and the Medical Research Council (MRC) scale for physical dysfunction, the Hospital Anxiety and Depression Scale (HADS) and the Post Traumatic Stress Disorder (PTSD) Checklist for psychological disorders, the Mini-Mental State Examination (MMSE) for cognitive alterations. EuroQol-5 Dimension (EQ-5D) is a widely used HRQoL measurement tool (Brooks et al. 2003) which consists of two distinct sections. The first one evaluates five subjective dimensions (mobility, self-care, daily activities, pain/discomfort, and anxiety/depression). The second section includes a visual analogue assessment (VAS) of perceived health level. A specific algorithm finally obtains a synthetic score.
Based on global literature data, the follow-up schemes could be structured as follows:
• First step during ICU stay: prevention measures and early rehabilitation interventions according to ABCDEFGH protocol.
• Second step before hospital discharge: recovery path description and enrolment for follow-up clinics
• A three-six-month follow-up visit with a direct physical examination, vital signs recording, and quality of life measurement.
• One-year last follow-up visit for those who had shown PICS symptoms at the first visit.
Moreover, the first follow-up visit represents an early opportunity to identify any physical, psychological, and/or cognitive deficits. Hence, the need to create a post-intensive support network, including physiotherapists, psychologists, psychiatrists, and others, to guarantee continuous assistance to post-critical patients.
PICS is gaining more and more importance as a consequence of COVID-19 pandemic, both because of the elevated number of ICU survivors and because of the significant likelihood that COVID-19 ICU patients will evidence a greater incidence of PICS. In fact, the long sedation that these patients require to allow mechanical ventilation is a risk factor for delirium, which is closely related to cognitive impairment. Additionally, due to infection control bundles, family members are restricted from in-person visiting and even health care staff may reduce the time they spend in contact with patients. This reduction in human interaction causes a decrease in cognitive stimulation, reorientation and reassurance to patients, causing further anxiety, depression and demoralisation. This creates a vicious circle of mental health impairment (Hosey et al. 2020). Considering the crucial role of evaluating COVID-19 long-term effects, technological advances should be leveraged to facilitate remote follow-up and comply with social distancing measures (Warnakulasuriya et al. 2020).
Conclusion
PICS is a widespread but under-recognised syndrome that can involve up to 80% of patients surviving acute respiratory failure who have received mechanical ventilation in ICU. Therefore, especially during this COVID-19 pandemic, it is of utmost importance for intensivists to implement evidence-based interventions (ABCDE) and to establish rehabilitation programmes that begin in ICU and continue after discharge. These actions can optimise survivorship experience and minimise long-lasting physical, cognitive and mental health impairments which cause profoundly disabling functional problems such as persistent fatigue, chronic pain, sleep dysfunction and overall low health- related quality of life.
“If you do not know what you are doing and how well you are doing it, you have no right to be doing it at all,"Professor Sir Bruce Keogh, NHS Medical Director 
References:
Allingstrup MJ, Kondrup J, Wiis J et al. (2017) Early goal-directed nutrition versus standard of care in adult intensive care patients: the single-centre, randomised, outcome assessorblinded EAT-ICU trial. Intensive Care Med, 43:637–47.
Appleton RT, Kinsella J, Quasim T (2015) The incidence of intensive care unit-acquired weakness syndromes: a systematic review. J. Intensive Care Soc, 16: 126–36.
Bednarik J, Lukas Z, Vondracek P (2003) Critical illness polyneuromyopathy: the electrophysiological components of a complex entity. Intensive Care Med, 29: 1505–14.
Brooks R et al. (2003) The Measurement and valuation of health status using EQ-5D: a European prospective. London: Kluwer Academic Publishers Dordrecht.
.
Brück E, Schandl A , Bottai M, Sackey P (2018) The impact of sepsis, delirium and psychological distress on self related cognitive function in ICU survivors-a prospective cohort study. J Intensive Care,.8;6:2. doi: 10.1186/s40560-017-0272-6.
Casaer MP, Wilmer A, Hermans G et al. (2013) Role of disease and macronutrient dose in the randomized controlled EPaNIC trial: a post hoc analysis. Am. J. Respir. Crit. Care Med, 187: 247–55.
Colbenson GA, Johnson A, Wilson ME (2019) Breathe (Sheff).Post-intensive care syndrome: impact, prevention, and management.15(2):98-101. doi: 10.1183/20734735.0013-2019
Connolly B, Salisbury L, O’Neill B et al. (2015) Exercise rehabilitation following intensive care unit discharge for recovery from critical illness. Cochrane Database Syst. Rev, CD008632.
Cullen DJ, Ferrara L, Briggs B, et al. (1976) Survival, hospitalization charges and follow-up results in critically ill patients. NEJM. 294:982–7.
Davydow DS, Gifford JM, Desai SV, Needham DM, Bienvenu OJ (2008) Posttraumatic stress disorder in general intensive care unit survivors: a systematic review. Gen. Hosp. Psychiatry, 30: 421–34.
Davydow DS, Zatzick D, Hough CL, Katon WJ (2013) In-hospital acute stress symptoms are associated with impairment in cognition 1 year after intensive care unit admission. Ann. Am. Thorac. Soc, 10: 450–7
Demling RH (2009) Nutrition, anabolism, and the wound healing process: an overview. Eplasty, 9: e9.
Devlin JW et al. (2018) Clinical Practice Guidelines for the Prevention and Management of Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption in Adult Patients in the ICU. Crit Care Med,.46(9):e825-e873. doi: 10.1097/CCM.0000000000003299.
EQ-5D 3L Users Guide (2018) Version 6.0.
Garrouste-Orgeas M, Coquet I, Perier A et al. (2012) Impact of an intensive care unit diary on psychological distress in patients and relatives*. Crit. Care Med, 40: 2033–40.
Griffiths J, Hatch RA, Bishop J, et al. An exploration of social and economic outcome and associated health-related quality of life after critical illness in general intensive care unit survivors: a 12-month follow-up study. Crit Care 2013; 17: R100
Guerra C, Hua M, Wunsch H. Risk of a diagnosis of dementia for elderly medicare beneficiaries after intensive care. Anesthesiology 2015
Harvey MA, Davidson JE. Post-intensive care syndrome: right care, right now…and later. Crit Care Med 2016; 44: 381–385
Hopkins RO, Suchyta MR, Snow GL, Jephson A, Weaver LK, Orme JF. Blood glucose dysregulation and cognitive outcome in ARDS survivors. Brain Inj. 2010; 24: 1478–84
Hosey, M.M., Needham, D.M. Survivorship after COVID-19 ICU stay. Nat Rev Dis Primers 6, 60 (2020). https://doi.org/10.1038/s41572-020-0201-1
Inoue S, Hatakeyama J, Kondo Y, et al. Post‐intensive care syndrome: its pathophysiology, prevention, and future directions. Acute Med Surg. 2019 Jul; 6(3): 233–246
Katz IR, Curyto KJ, TenHave T, Mossey J, Sands L, Kallan MJ. Validating the diagnosis of delirium and evaluating its association with deterioration over a one-year period. Am. J. Geriatr. Psychiatry 2001; 9: 148–59.
Kim IY, Schutzler S, Schrader A et al. The anabolic response to a meal containing different amounts of protein is not limited by the maximal stimulation of protein synthesis in healthy young adults. Am. J. Physiol. Endocrinol. Metab. 2016; 310: E73–80.
Lambell KJ, King SJ, Forsyth AK, Tierney AC. Association of energy and protein delivery on skeletal muscle mass changes in critically ill adults: a systematic review. JPEN J. Parenter. Enteral Nutr. 2018; 42: 1112–22
Latronico N, Bolton CF. Critical illness polyneuropathy and myopathy: a major cause of muscle weakness and paralysis. Lancet Neurol. 2011; 10: 931–41.
Mandebvu F, Kalman M. The 3 Ds, and newly acquired cognitive impairment: issues for the ICU nurse. Crit. Care Nurs. Q. 2015; 38: 317–26
McClave SA, Taylor BE, Martindale RG et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: society of critical care medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). JPEN J. Parenter. Enteral Nutr. 2016; 40: 159–211
Morton RW, Murphy KT, McKellar SR et al. A systematic review, meta-analysis and meta-regression of the effect of protein supplementation on resistance training-induced gains in muscle mass and strength in healthy adults. Br. J. Sports Med. 2018; 52: 376–84.
Pandharipande PP, Girard TD, Jackson JC, et al. Long-term cognitive impairment after critical illness. N Engl J Med 2013; 369: 1306–1316
Phillips SM. A brief review of critical processes in exerciseinduced muscular hypertrophy. Sports Med. 2014; 44(Suppl 1): S71–7.
Pisani MA, Redlich CA, McNicoll L, Ely EW, Friedkin RJ, Inouye SK. Short-term outcomes in older intensive care unit patients with dementia. Crit. Care Med. 2005; 33: 1371–6.
Rawal G, Yadav S and Kumar R. Post-intensive Care Syndrome: an Overview. J TranslInt Med. 2017 Jun; 5(2): 90–92.
Schofield-Robinson O J, Lewis S R, Smith A F, et al. Follow-up services for improving long-term outcomes in intensive care unit (ICU) survivors. Cochrane Library 2018
Singer P, Blaser AR, Berger MM et al. ESPEN guideline on clinical nutrition in the intensive care unit. Clin. Nutr. 2018; 38: 48–79
Ullman A J, Aitken L M, et al. Cochrane Database Syst Rev. 2014 Dec; 2014(12): CD010468. Diaries for recovery from critical illness.
Van Der SchaafMBakhshi-Raiez F, , Van Der Steen M, Dongelmans DA, De Keizer NF. Recommendations for intensive care follow-up clinics; report from a survey and conference of Dutch intensive cares.. Minerva Anestesiol. 2015 Feb;81(2):135-44.
Warnakulasuriya SR, Patel RC, Singleton GF, Moonesinghe SR. Patient-reported outcomes for ambulatory surgery.CurrOpinAnaesthesiol. 2020 Sep 29. doi: 10.1097/ACO.0000000000000921. Online ahead of print.PMID: 33002956
Wolters AE, Slooter AJ, van der Kooi AW, van Dijk D. Cognitive impairment after intensive care unit admission: a systematic review. Intensive Care Med. 2013; 39: 376–86











