ICU Management & Practice, Volume 22 - Issue 3, 2022
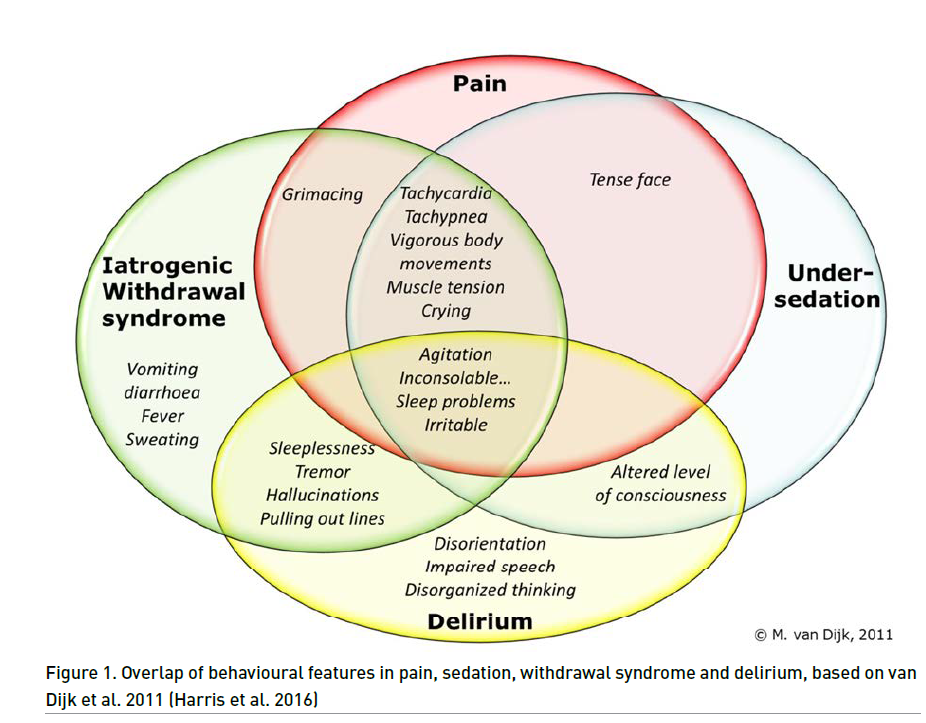
Critically ill paediatric patients often suffer from pain secondary to trauma, complex medical procedures, invasive testing monitoring devices and illness-induced discomfort. Although the gold standard for assessing patient comfort is self-report, in paediatrics it may be quite difficult due to the wide spectrum of ages, weights, variability in developmental stages as well as the interplay between sedative and analgesic drugs. In addition, it should not be forgotten that clinical signs of iatrogenic withdrawal or delirium may coexist (Harris et al. 2016). That is why standardised assessment tools have been proposed and validated for intubated and preverbal patients in order to limit avoidable variability in assessment.
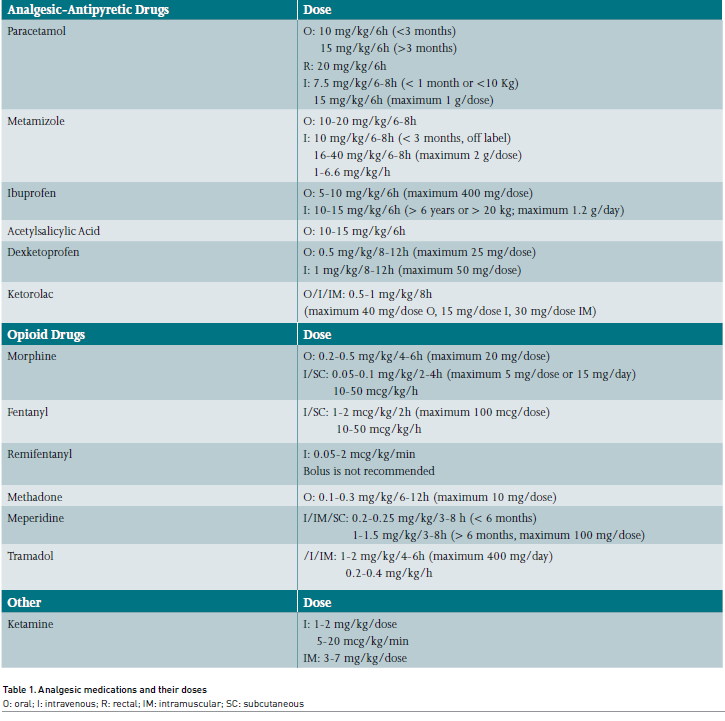
The aim of this article is to provide a general overview of the current and most used pain treatment options that are available in paediatric intensive care units (PICU), as well as to highlight some observations about their use in paediatrics. The doses are collected in the attached tables.
The Analgesic Therapy
The main goal of analgesic therapy is to provide comfort, reduce the physiological stress response and minimise associated adverse events such as respiratory depression, risk of addiction, haemodynamic instability and end organ injury (Egbuta and Mason 2021). Sedative, analgesic and local anaesthetics are important components of appropriate analgesic regiments, but behavioural techniques should not be forgotten since they can be relevant for addressing the emotional component of pain. Finding the optimal analgesic and sedative therapy require a continuous patient assessment with validated tools as pain scales, attending that many analgesic drugs are synergistic with sedating agents (Georgiou et al. 2020). The Premature Infant Pain Profile (PIPP) scale in neonates and the COMFORT behaviour scale, Face, Legs, Activity, Cry and Consolability scale (FLACC) and the Multidimensional Assessment of Pain Scale are the most commonly used pain scales in the intensive care settings (Harris et al. 2016).
Non-Pharmacological Measures
The emotional component of pain is particularly strong in children, so the non-pharmacological measures have a vital role in their treatment. They are commonly focused on decreasing patients’ anxiety and, consequently, they may reduce the need of analgesic and sedative drugs.
They are usually based on nursing care and environmental measures like relaxing techniques, music therapy, hypnosis, distraction techniques and cognitive therapies addressed to explain the illness or the invasive procedures to the patient. It is important to promote the sleep-wake cycle adapting the lighting to the time of day and avoiding noises or procedures during the sleep. Also, the presence of the parents during the admission and the performance of invasive medical procedures is essential for decreasing anxiety and the discomfort inherent at the intensive care unit admission process. In this same sense, the presence of family pictures or toys in the child’s environment can also be useful. In neonates, the use of sucrose via oral and the skin-to-skin contact is significantly effective (Chumpitazi et al. 2022).
Analgesic Medications
Non-Opioid Drugs
These are drugs with limited analgesic effect and no-dose dependent (increasing the dose above a certain level does not produce more analgesia). There are two groups: analgesics-antipyretics and non-steroidal anti-inflammatory drugs (NSAIDs).
Analgesics-Antipyretics
These drugs have an analgesic and antipyretic effect, but they do not exert an anti-inflammatory action. They are usually used, together with opiates, in moderate or severe pain, if there is a risk of bleeding or in case of minor surgery. Within this group we find drugs such as paracetamol or metamizole. Paracetamol has no toxicity at therapeutic doses but it can develop hepatic and renal toxicity in case of overdose. Metamizole is especially useful for the management of colic pain. It causes few side effects, but it can produce hypotension when administered in fast bolus, especially in hypovolaemic patients. Moreover, it has been related with the appearance of aplastic anaemia and agranulocytosis, which is why it is not marketed in some European countries (Egbuta and Mason 2021).
NSAIDs
These drugs have an analgesic, antipyretic and anti-inflammatory effect, so they are mainly used in presence of mild or moderate pain with an inflammatory component, as well as in minor surgeries together with opiates. In general, they have more analgesic activity than paracetamol. They should be administered orally or intravenously because rectal absorption is erratic. There have been reported side effects over the gastric mucosa (gastritis, gastric ulcer, digestive bleeding) and platelet aggregation.
Within this group are available drugs such as ibuprofen, dexketoprofen or ketorolac. Ibuprofen is the most used since it is generally well tolerated and it entails less risk of digestive bleeding in comparison with other NSAIDs, although the gastrointestinal complications are the most common. On the other hand, it is not recommended to use dexketoprofen for more than five days or if there is kidney failure (López-Herce et al. 2019).
Acetylsalicylic acid is also included in this group. Despite being a drug classically widely used in paediatrics, it is currently not recommended for patients under 16 years of age with viral infections due to its association with Reye syndrome. As a consequence, its current use is limited as platelet antiaggregant.
Opioid Drugs
Opioids exert their effect by interacting with opioid receptors. They mainly act over μ receptors (analgesia, miosis, respiratory depression), which are found in presynaptic terminals on central nervous system (brain, spinal cord), peripheral tissue and in other tissues like the adrenal medulla and myenteric plexus. Opioids pose a dose-dependent respiratory depression with increased risk if used with other sedatives. In this sense, naloxone acts as an antidote for the reversal of the effects produced by opiates. Also, they exhibit a risk of dependence and withdrawal, so it is recommended to wean them slowly in those patients who have received high doses of opioid (Barr et al. 2013). In children under six months, the dose should be reduced by 25-50% and the interval between doses should be doubled or tripled the lower the age (López-Herce et al. 2019).
There are many useful opiates in paediatrics such as morphine, fentanyl, methadone or others. Morphine is the oldest of the opiates and it is especially useful for pain management in polytraumatised, burn, post-surgery patients and sickle cell crises. Morphine induces a histaminic release that can explain the appearance of vasodilation, pruritus or hypotension that sometimes appear after its administration. Besides, it has been related with risk of seizures in neonates when used at high doses.
Fentanyl is a synthetic morphine derivative but with better haemodynamic tolerance. It is mainly used during short painful procedures, such as intubation procedure, and for the analgesic maintenance during mechanical ventilation. The duration of its effect is prolonged up to 30 minutes when administered intravenously, but when the administration is continuous and prolonged it can accumulate in peripheral compartments increasing its half-life. Despite being a rare effect, with rapid large doses (> 5 mcg/kg) there is a risk of chest wall rigidity that can result in a respiratory failure especially in neonates and small infants.
Remifentanyl is a synthetic opioid specially recommended in patients with renal or hepatic dysfunction since it is quickly metabolised by plasma esterases. Besides, it can be useful in those patients in whom it is necessary to abruptly interrupt the sedative and analgesic therapy to assess their mental status. However, as other opioids, it can cause respiratory and haemodynamic failure (it is recommended not to administer in bolus) and it has been suggested that it has a high risk of tolerance and withdrawal when it is used at high doses or for long periods of time.
Other opiates of interest in paediatrics are meperidine, which is especially useful in patients with biliary pathology or pancreatitis (due to its anticholinergic effect over the bile ducts), or tramadol, whose special interest lies in the management of neuropathic pain. It has been related with mild side effects like nausea, vomiting or constipation.
Methadone is a synthetic μ receptor agonist equipotent to morphine. In the PICU setting it is mainly used to prevent opioid withdrawal for those patients who have received continuous infusions. It has been related with some life-threatening adverse effects, like significant bradycardia or arrhythmias (QT interval prolongation) in those patients with structural heart disease (Egbuta and Mason 2021).
Patient-Controlled Analgesia
This is a method of analgesic administration through an automatic pump controlled by the patient, looking for better pain control. The main indication for patient-controlled analgesia (PCA) is acute pain (especially of post-surgical origin) or pain related with oncological process. It usually uses the intravenous route and the drugs most used in paediatrics are morphine and fentanyl, although there are also guidelines described with tramadol and combinations of analgesics with sedatives (López-Herce et al. 2019).
Others
Ketamine
Ketamine is a N-metil-D-Aspartate (NMDA) receptor antagonist, so it prevents the excitatory activity of glutamate. Small doses produce analgesia with amnesia, without impairing the airway protective reflexes. Moderate doses provide analgesia and sedation, while high doses produce general anaesthesia. Ketamine suffers liver metabolism and kidney excretion. Side effects include an increase of respiratory secretions by cholinergic stimulus (it could be attenuated with previous bolus of atropine), hallucinations (they can be attenuated with a benzodiazepine dose), tachycardia, hypertension and, despite having a bronchodilator effect, laryngospasm. Although classically it has been related to increases in intracranial pressure, the results are contradictory and recent studies suggest that it could even decrease it (Chan et al. 2022).
Local and topical anaesthetics
These are drugs that can temporarily prevent the nerve impulse conduction if they are used locally in high concentration. As an example of local anaesthetic, we have lidocaine (which can be used with epinephrine in order to extend its action) or bupivacaine. Also, there are available some topical anaesthetics that achieve local receptor insensitivity for pain in front of painful stimulus.
Only Analgesia?
Usually, in addition to analgesia, sedation should be administered to improve the comfort of the critically ill paediatric patient allowing, for example, adaptation to mechanical ventilation. In this context, it is not always easy to distinguish between pain and discomfort not caused by pain, especially in young children. It is vitally important to remember that sedatives do not provide analgesia. There are multiple sedatives available such as some benzodiazepines, propofol, alpha-2 adrenergic agonists or even ketamine itself.
The alpha-2 adrenergic agonists such as clonidine or dexmedetomidine have been increasingly used for sedation in the PICU over the last decade. They are an attractive choice for sedation since they do not decrease respiratory drive, but the main disadvantage is they can cause haemodynamic instability with bradycardia or hypotension, so they are not usually the first-line choice in young infants or cardiac patients.
Given that all of them are related to potential adverse effects and complications, such as withdrawal or delirium, their dosage should be titrated based on validated sedation scales as the Richmond Agitation Sedation Scale (RASS) or Paediatric Sedation State Scale (PSSS) (Laures et al. 2019).
Conclusion
In conclusion, critical paediatric patients often experience pain during their admission. It may be due to multiple reasons of the same disease process or hospitalisation and supposes a handicap to achieve an adequate adaptation to therapy and to the environment. In children, it is especially important to address the emotional component that usually accompanies pain, so non-pharmacological measures are essential and usually allow reducing the dose of analgesics. There are many analgesic drugs, each with their own characteristics and possible side effects, so their dosage must be titrated according to validated scales.
Conflict of Interest
None.
References:
Barr J, Fraser GL, Puntillo K et al. (2013) Clinical Practice Guidelines for the Management of Pain, Agitation, and Delirium in Adult Patients in the Intensive Care Unit: Crit. Care Med. 41:263–306.
Chan K, Burry LD, Tse C et al. (2022) Impact of Ketamine on Analgosedative Consumption in Critically Ill Patients: A Systematic Review and Meta-Analysis. Ann. Pharmacother. 106002802110696.
Chumpitazi CE, Chang C, Atanelov Z et al. (2022) Managing acute pain in children presenting to the emergency department without opioids. J. Am. Coll. Emerg. Physicians Open 3.
Egbuta C, Mason KP (2021) Current State of Analgesia and Sedation in the Pediatric Intensive Care Unit. J. Clin. Med. 10:1847.
Georgiou E, Paikousis L, Lambrinou E et al. (2020) The effectiveness of systematic pain assessment on critically ill patient outcomes: A randomised controlled trial. Aust. Crit. Care. 33:412–419.
Harris J, Ramelet A.-S, van Dijk M et al. (2016) Clinical recommendations for pain, sedation, withdrawal and delirium assessment in critically ill infants and children: an ESPNIC position statement for healthcare professionals. Intensive Care Med. 42:972–986.
Laures E, LaFond C, Hanrahan K et al. (2019) Pain Assessment Practices in the Pediatric Intensive Care Unit. J. Pediatr. Nurs. 48:55–62.
López-Herce J, Calvo Rey C, Rey Galán C, Rodríguez Núñez A (2019) Manual de Cuidados Intensivos Pediátricos, 5a. ed. Publimed, Madrid.










