ICU Management & Practice, ICU Volume 11 - Issue 3 - Autumn 2011
Introduction
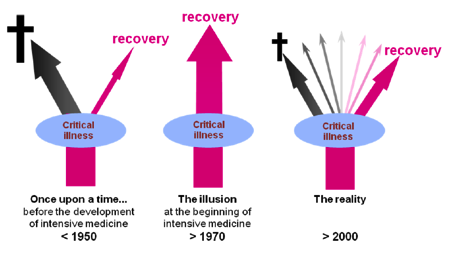
Intensive
care medicine is quite a recent medical discipline born around 1950. At the
beginning, the medical world held an illusion that new highly sophisticated
techniques would allow for the recovery of every single patient. A half century
later, the discipline has grown up and there is a realisation that while many
more lives can be saved and obviously fewer patients die, the many patients who
survive do so with variable degrees of disability; some acceptable, and some
less acceptable and unforeseen until recently (Figure 1). Additionally,
Intensive Care Units (ICU) are scarce resources that represent a large part of national
health expenditure and hospital budgets. ICU costs are growing and represents between
0.5 to 1% of the gross domestic product (Halpern and Pastores 2010).
Because ICU costs are important and outcomes may be poor, the aim of intensive medicine should be directed towards outcomes that could be considered more satisfactory to patients and societies’ perspectives. More than ICU mortality, long-term survival and patient-centred outcomes, such as functional status or Quality Of Life (QOL) should be considered and advised to be sought (Angus and Carlet 2003). Among all critically ill patients, elderly or chronic critically ill patients are especially prone to develop unsatisfactory outcomes.
The aim of the present article is to describe some of the major difficulties encountered by the patients after their stay in ICUs. Many of these difficulties are under reported, since patients and their relatives are so grateful towards the ICU caregivers that they would not dare to complain. However, the literature now shows evidence that there is room for improvement in their management and the targets start to be known.
Outcome After ICU: General Considerations
Mortality
can be described in different ways: ICU, hospital or follow up mortality. There
are multiple studies that are difficult to compare, because ICU or hospital
mortality depend on the organisation or structure of the hospital and can differ
among types of ICUs, hospitals and even countries (e.g. University vs non
university; paediatric vs adult ICU; general ICU vs specific ICU; presence of
intermediate care or lack of), as well as the case-mix and the timing of the
mortality assessment. Review articles describe ICU mortalities ranging from 8
to 33%, hospital mortalities from 11 to 64%, one-month mortalities from 15-21%
and follow-up mortalities at 12 months after ICU ranging from 26 to 63%.
Generally the most common mortality data used is the hospital or “28/30 day”
mortality. Only recently have ICU managers begun to focus their attention on long-term
mortality. Interestingly, mortality can be assessed at four different moments
(Figure 2). After discharge from the hospital, there are still further deaths
(the after-hospital excess mortality). Compared to an age- and gender-matched population,
higher mortality persists up to 15 years after ICU discharge. The factors associated
with one- year mortality are:
- Older age;
- Presence of co-morbidities;
- Presence of a new malignancy;
- Admission diagnosis;
- ICU admission severity, and
- The number of organ failures during ICU stay.
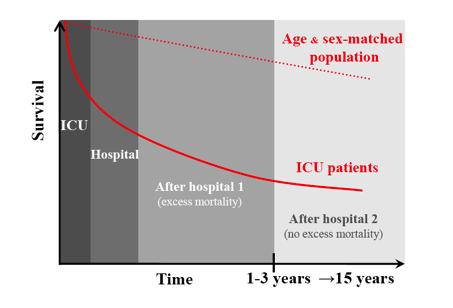
Additional factors, such as male gender and ICU length of stay are associated with an increased mortality up to 15 years after ICU discharge (Williams et al. 2010). Emergency admissions, functional status and the QOL before ICU admission may also impact on after-hospital mortality. The morbidity after ICU can be divided three main fields: Physical, non-physical and other impacts.
Physical Impairments
The physical impairment can be addressed through specific organ dysfunctions or by a general assessment of the status using validated instruments. Studies indicate that the functionalstatus is already lower before ICU admission compared to an age- and gender-matched population (Hennessy et al. 2005). After ICU, functional status is similar to or only slightly reduced from status before ICU in two-thirds of patients. A great majority of patients will not need any help after ICU discharge. However, there may be huge differences between patients, depending on ICU admission diagnosis. Organ specific functional status is often assessed by instruments and is not explicitly developed for critically ill patients; therefore their reliability sometimes has to be questioned. Respiratory problems may persist, especially in ARDS patients, even after 24 months, with chronic dyspnea or sequelae from tracheotomies (Herridge et al. 2003). Polyneuropathies, weight loss and sexual dysfunctions may affect critically ill patients for years after ICU (Flaatten 2007).
Non-Physical Impairments
Concerning non physical impairments, up to 50% of ICU patients suffer pain after ICU (Boyle et al. 2004). Cognitive disorders are described in half of the general, and in up to three-quarters of an ARDS population. Half of ICU patients may suffer depression, delusional memories, panic attacks or insomnia (Granja et al. 2005; Flaatten 2007). Posttraumatic disorders have been described in 5-64% of patients, depending on the instrument used and on the type of patients included (Davydow et al. 2009a; Davydow et al. 2009b). Younger age, male gender, traumatic and delusional memories of the ICU as well as previous depression seem to be risk factors associated with their occurrence. The QOL of ICU patients is already reduced before ICU admission, as is functional status when compared to an age- and gendermatched population. After ICU, most patients regain their pre-ICU QOL in 6-12 months. ARDS and traumatic brain injury patients may take up to 24 months to stabilise and regain pre-ICU QOL. Even elderly patients seem to recover as fast as younger ICU patients (Hennessy et al. 2005).
Other Impacts
If we look at other outcomes, we have to emphasise that 75-90% of patients surviving ICU, even the older ones, will be able to go back to their homes within 12 months after ICU (Conti et al. 2011). Up to 60-80% of the previously working population who survived will be able to go back to their work, however, ICU admission diagnoses play a role in the differing results. There is very little data regarding other areas of major life events, such as divorces, violence, and economic strains after ICU. Such fields also directly address patient-centred outcome and may warrant more interest in future studies.
Chronic Critically Ill
Chronic critically ill or long-term ICU patients are often defined according to their length of stay. These LOS guidelines often differ:
• More than 96 hours (Zilberberg and Shorr 2008),
• More than 7 days (Weissman 2000),
• More than 28 days (Estenssoro et al. 2006) or
• More than 30 days (Friedrich et al. 2006).
They can also be conceptually defined as patients who survive the acute phase and who remain dependent on the ICU technology and skills. For the last decade, probably due to the increasing proficiency of intensive medicine, this population has grown rapidly, whereas the number of patients reaching hospital discharge did not increase as much (Zilberberg and Shorr 2008). In our institution, patients remaining in ICU for more than 7 days had higher ICU and hospital mortality (17 and 34 % respectively). On a threemonth follow-up, a third of these patients had died, another third remained in hospital longer or were institutionalised (personal unpublished data), but the good news is that a third could return home. Although the survival rate seems lower than for general ICU population, chronic critically ill patients seem to achieve a long-term quality of life that seems similar (Stricker et al. 2005). However the amount of knowledge regarding this population remains poor.
Elderly Patients
Occidental countries are characterised by a demographic aging. The proportion of elderly patients is also growing in ICUs. This growing patient group consumes more than half of all ICU days (Pronovost et al. 2001). Elderly patients represent a peculiar population since they are more prone to develop chronic diseases such as diabetes, hypertension or atherosclerosis. This biological aging progresses in a continuum leading to the development of the frailty syndrome (Inouye et al. 2007). Therefore elderly patients may have a limited physiological reserve and their capacity to heal may be somewhat altered, resulting in less favourable outcome than that of younger patients after an acute severe illness.
Depending on the definition of elderly patients and after correction of confounding factors, chronological age itself has a limited effect on mortality (Boumendil et al. 2007). However, when elderly patients survive ICU, they remain at a high risk of death especially during the first months (Kaarlola et al. 2006).
Besides mortality, the two major determinants to predict long-term outcome for the elderly population are the condition of the patient at the completion of their ICU stay and their QOL. As for the mortality, the data are difficult to interpret and subject to a pessimistic or optimistic point of view (Hennessy et al. 2005). The functional status is obviously diminished after an ICU stay, whereas the self-reported QOL seems to be as good as similar-age general population (Ricou and Merlani 2008). Their recovery rate seems not longer than that of younger patients (Capuzzo et al. 2006).
Finally some studies about elderly patients’ preferences regarding their outcome after ICU seem to suggest that the most unsatisfying issue for them is a discharge to a nursing home. Most patients are "very unwilling" or "would rather die". Although many suffer of a decreased functional status, most of the elderly ICU survivors are able to go back to their
home and most, relatively rapidly after their hospital discharge (Conti et al. 2011).
What Can be Done in ICU to Improve Long-Term Outcomes After ICU?
Two main axes seem to offer possibilities of action to improve the QOL after ICU, namely: physical strength and neuropsychological recovery. Increased care for adequate nutrition decreases the length of mechanical ventilation and ICU stay and may shorten the recovery phase (Thibault and Pichard 2010). Longterm mortality and prolonged physical impairment are closely related to the ICU acquired paresis that may be prevented or treated earlier during the ICU stay by precocious mobilisation and careful nutrition (Merlani 2008). Neuropsychological outcomes such as post traumatic stress disorder impact heavily on patients’ QOL (Granja et al. 2005). Related associated factors such as prolonged sedation and physical restraints seem to offer some targets to improvement, as do the utilisation of intensive care diaries (Jones et al. 2010).
Conclusion
There
are numerous unrecognised or underestimated problems after ICU regarding
physical and psychological recovery, as well as family, social, employment and
housing aspects. However, given the present state of knowledge, prevalence is
given to focus on the two main axes for improving life after ICU: Attempting to
increase physical strength and support neuropsychological recovery. Further
studies are clearly needed to extend our knowledge about other aspects of
patients’ long-term outcomes, so that strategies to affect and improve these
issues can also be incorporated into future recovery plans.
References:
ANGUS, D. C., KELLEY, M. A., SCHMITZ, R. J., WHITE, A. & POPOVICH, J., JR. (2000) Caring for the critically ill patient. Current and projected workforce requirements for care of the critically ill and patients with pulmonary disease: can we meet the requirements of an aging population? Jama, 284, 2762-70.
BOUMENDIL, A., SOMME, D., GARROUSTE-ORGEAS, M. & GUIDET, B. (2007) Should elderly patients be admitted to the intensive care unit? Intensive Care Med, 33, 1252-62.
BOYLE, M., MURGO, M., ADAMSON, H., GILL, J., ELLIOTT, D. & CRAWFORD, M. (2004) The effect of chronic pain on health related quality of life amongst intensive care survivors. Aust Crit Care, 17, 104-6, 108-13.
BROOMHEAD, L. R. & BRETT, S. J. (2002) Clinical review: Intensive care follow-up--what has it told us? Crit Care, 6, 411-7.
CAPUZZO, M., MORENO, R. P., JORDAN, B., BAUER, P., ALVISI, R. & METNITZ, P. G. (2006) Predictors of early recovery of health status after intensive care. Intensive Care Med.
CONTI, M., FRIOLET, R., ECKERT, P. & MERLANI, P. (2011) Home return 6 months after an intensive care unit admission for elderly patients. Acta Anaesthesiol Scand, 55, 387-93.
DAVYDOW, D. S., KATON, W. J. & ZATZICK, D. F. (2009a) Psychiatric morbidity and functional impairments in survivors of burns, traumatic injuries, and ICU stays for other critical illnesses: A review of the literature. International Review Of Psychiatry, 21, 531-538.
DAVYDOW, D. S., ZATZICK, D. F., RIVARA, F. P., JURKOVICH, G. J., WANG, J., ROY-BYRNE, P. P., KATON, W. J., HOUGH, C. L., KROSS, E. K., FAN, M.-Y., JOESCH, J. & MACKENZIE, E. J. (2009b) Predictors of posttraumatic stress disorder and return to usual major activity in traumatically injured intensive care unit survivors. General Hospital Psychiatry, 31, 428-435.
DE JONGHE, B., SHARSHAR, T., LEFAUCHEUR, J. P., AUTHIER, F. J., DURAND-ZALESKI, I., BOUSSARSAR, M., CERF, C., RENAUD, E., MESRATI, F., CARLET, J., RAPHAEL, J. C., OUTIN, H. & BASTUJI-GARIN, S. (2002) Paresis acquired in the intensive care unit: a prospective multicenter study. Jama, 288, 2859-67.
DOWDY, D. W., EID, M. P., SEDRAKYAN, A., MENDEZ-TELLEZ, P. A., PRONOVOST, P. J., HERRIDGE, M. S. & NEEDHAM, D. M. (2005) Quality of life in adult survivors of critical illness: A systematic review of the literature. Intensive Care Medicine, 31, 611-620.
ESTENSSORO, E., REINA, R., CANALES, H. S., SAENZ, M. G., GONZALEZ, F. E., APREA, M. M., LAFFAIRE, E., GOLA, V. & DUBIN, A. (2006) The distinct clinical profile of chronically critically ill patients: a cohort study. Crit Care, 10, R89.
FLAATTEN, H. (2007) Long-term outcomes after ICU. IN KUHLEN, R., MORENO, R., RANIERI, M. & RHODES, A. (Eds.) 25 years of progress and innovation in IC medicine.
Berlin, Medizinische Wissenschaftliche Verlagsgesellschaft.
FRIEDRICH, J. O., WILSON, G. & CHANT, C. (2006) Long-term outcomes and clinical predictors of hospital mortality in very long stay intensive care unit patients: a cohort study. Crit Care, 10, R59.
GRANJA, C., LOPES, A., MOREIRA, S., DIAS, C., COSTA-PEREIRA, A. & CARNEIRO, A. (2005) Patients' recollections of experiences in the intensive care unit may affect their quality of life. Crit Care, 9, R96-109.
HALPERN, N. A. & PASTORES, S. M. (2010) Critical care medicine in the United States 2000-2005: an analysis of bed numbers, occupancy rates, payer mix, and costs. Crit Care Med, 38, 65-71.
HAYES, J. A., BLACK, N. A., JENKINSON, C., YOUNG, J. D., ROWAN, K. M., DALY, K. & RIDLEY, S. (2000) Outcome measures for adult critical care: a systematic review. Health Technol Assess, 4, 1-111.
HENNESSY, D., JUZWISHIN, K., YERGENS, D., NOSEWORTHY, T. & DOIG, C. (2005) Outcomes of elderly survivors of intensive care - A review of the literature. Chest, 127, 1764-1774.
HERRIDGE, M. S., CHEUNG, A. M., TANSEY, C. M., MATTE-MARTYN, A., DIAZ-GRANADOS, N., AL-SAIDI, F., COOPER, A. B., GUEST, C. B., MAZER, C. D., MEHTA, S., STEWART, T. E., BARR, A., COOK, D. & SLUTSKY, A. S. (2003) One-year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med, 348, 683-93.
INOUYE, S. K., STUDENSKI, S., TINETTI, M. E. & KUCHEL, G. A. (2007) Geriatric syndromes: clinical, research, and policy implications of a core geriatric concept. Journal of the American Geriatrics Society, 55, 780-91.
JACOBS, P. & NOSEWORTHY, T. W. (1990) National estimates of intensive care utilization and costs: Canada and the United States. Crit Care Med, 18, 1282-6.
JONES, C., BACKMAN, C., CAPUZZO, M., EGEROD, I., FLAATTEN, H., GRANJA, C., RYLANDER, C. & GRIFFITHS, R. D. (2010) Intensive care diaries reduce new onset post traumatic stress disorder following critical illness: a randomised, controlled trial. Critical Care, 14.
JONES, C., BACKMAN, C., CAPUZZO, M., FLAATTEN, H., RYLANDER, C. & GRIFFITHS, R. D. (2007) Precipitants of post-traumatic stress disorder following intensive care: a hypothesis generating study of diversity in care. Intensive Care Med, 33, 978-85.
KAARLOLA, A., PETTILA, V. & KEKKI, P. (2003) Quality of life six years after intensive care. Intensive Care Med, 29, 1294-9.
KAARLOLA, A., TALLGREN, M. & PETTILA, V. (2006) Long-term survival, quality of life, and quality-adjusted life-years among critically ill elderly patients. Critical Care Medicine, 34, 2120-2126.
KVALE, R. & FLAATTEN, H. (2002) Changes in intensive care from 1987 to 1997 - has outcome improved? A single centre study. Intensive Care Medicine, 28, 1110-1116.
MATTIMORE, T. J., WENGER, N. S., DESBIENS, N. A., TENO, J. M., HAMEL, M. B., LIU, H., CALIFF, R., CONNORS, A. F., JR., LYNN, J. & OYE, R. K. (1997) Surrogate and physician understanding of patients' preferences for living permanently in a nursing home. J Am Geriatr Soc, 45, 818-24.
MERLANI P, V. M., PERNEGER T, RICOU B. (2008) Clinical events during ICU stay are related to the QOL of patients 1 year after. Swiss Medical Forum, 8, Supp 42.
PRONOVOST, P. J., WATERS, H. & DORMAN, T. (2001) Impact of critical care physician workforce for intensive care unit physician staffing. Curr Opin Crit Care, 7, 456-9.
RICOU, B. & MERLANI, P. (2008) What limits for acute care in the elderly? Curr Opin Anaesthesiol, 21, 380-5.
RUBENFELD, G. D., ANGUS, D. C., PINSKY, M. R., CURTIS, J. R., CONNORS, A. F., JR. & BERNARD, G. R. (1999) Outcomes research in critical care: results of the American Thoracic Society Critical Care Assembly Workshop on Outcomes Research. The Members of the Outcomes Research Workshop. Am J Respir Crit Care Med, 160, 358-67.
SOMME, D., MAILLET, J. M., GISSELBRECHT, M., NOVARA, A., RACT, C., FAGON, J. Y. & ELY, E. W. (2003) Critically ill old and the oldest-old patients in intensive care: short- and long-term outcomes. Optimizing outcomes for older patients treated in the intensive care unit. Intensive Care Med, 29, 2137-43.
STRICKER, K., ROTHEN, H. U. & TAKALA, J. (2003) Resource use in the ICU: short- vs. long-term patients. Acta Anaesthesiol Scand, 47, 508-15.
STRICKER, K. H., CAVEGN, R., TAKALA, J. & ROTHEN, H. U. (2005) Does ICU length of stay influence quality of life? Acta Anaesthesiol Scand, 49, 975-83.
THIBAULT, R. & PICHARD, C. (2010) Nutrition and clinical outcome in intensive care patients. Curr Opin Clin Nutr Metab Care, 13, 177-83.
VILLET, S., CHIOLERO, R. L., BOLLMANN, M. D., REVELLY, J. P., CAYEUX, R. N. M., DELARUE, J. & BERGER, M. M. (2005) Negative impact of hypocaloric feeding and energy balance on clinical outcome in ICU patients. Clin Nutr, 24, 502-9.
WEISSMAN, C. (2000) Analyzing the impact of long-term patients on ICU bed utilization. Intensive Care Med, 26, 1319-25.
WILLIAMS, T. A., DOBB, G. J., FINN, J. C., KNUIMAN, M. W., GEELHOED, E., LEE, K. Y. & WEBB, S. A. R. (2008) Determinants of long-term survival after intensive care. Critical Care Medicine, 36, 1523-1530.
WILLIAMS, T. A., DOBB, G. J., FINN, J. C. & WEBB, S. A. R. (2005) Long-term survival from intensive care: a review. Intensive Care Medicine, 31, 1306-1315.
WILLIAMS, T. A., HO, K. M., DOBB, G. J., FINN, J. C., KNUIMAN, M. & WEBB, S. A. R. (2010) Effect of length of stay in intensive care unit on hospital and long-term mortality of critically ill adult patients. British Journal Of Anaesthesia, 104, 459-464.
ZILBERBERG, M. D. & SHORR, A. F. (2008) Prolonged acute mechanical ventilation and hospital bed utilization in 2020 in the United States: implications for budgets, plant and personnel planning. BMC Health Serv Res, 8, 242.





