ICU Management & Practice, ICU Volume 12 - Issue 2 - Summer 2012
Metabolic nutritional support is a cornerstone in the management of seriously ill patients. Election of the route of nutritional administration – parenteral nutrition (PN), enteral nutrition (EN) or mixed – depends on the condition and integrity of the digestive tract as well as the diagnosis and condition of the patient.
If the gastrointestinal tract is functional and the haemodynamic status of the patient is adequate, EN must be the first choice in the nutritional therapy of seriously ill patients. Many benefits have been proposed to justify the administration of enteral nutrients as quickly as possible (Table 1), although based on international practice guidelines, there are considerations to be taken for the implementation of early EN (in the first 24 - 48 hours).
The critically ill patient is in a constant hypermetabolic state, resulting in an impending loss of protein and quickly occurring protein malnutrition, which is why the administration of exogenous nutrients in the early hours is critical to preventing the loss of visceral structure, protein reserves and circulating proteins.
With the rate of malnutrition in these patients based on protein, we must consider alterations in metabolism that are caused by other macronutrients – lipid and carbohydrate – so that we can carefully calculate their required administration. In this way, we can avoid side effects and minimise the risk of metabolic complications that are most common with this type of support.
Early EN is Not Always the Best Choice
Despite numerous proposed benefits of early EN, contraindications to enterally administered nutrients exist, which are divided into absolute and relative. Absolute contraindications are usually mechanistic. Within these are persistent ileus, intestinal obstruction, peritonitis, massive gastrointestinal haemorrhage, splanchnic hypoperfusion and high-output fistulae. Among the relative contraindications are intolerance of enteral route intestinal resection, moderate-output fistulae, pancreatitis, and inflammatory bowel disease. A recent anastomosis is not considered as a contraindication to initiation of the enteral route.
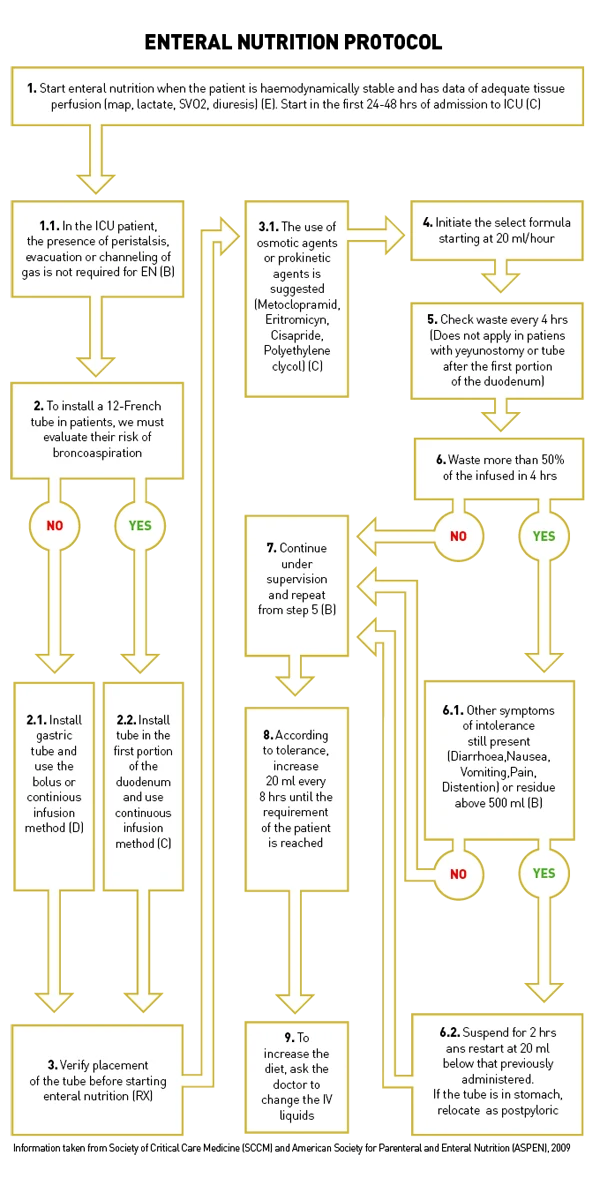
Enteral Nutrition Protocol
A protocol should be followed to consider the best possible nutritional route for a patient, taking numerous factors into consideration. Guidelines for the Provision and Assessment of Nutrition Support Therapy in the Adult Critically III Patient (Society of Critical Care
Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (ASPEN) 2009) provides suggestions for a broad range of scenarios, with recommendations graded from A to E, depending on the level of evidence available. The flow diagram in Figure 1 presents a simplified version of the guidelines, which aims to further facilitate the decision-making process. The protocol provides an effective strategy for maximising the benefits and minimising the risks of enteral nutrition in critically ill patients, and automating its provision, with recommendations; although it should be considered that studies are continually being completed and recommendations are evolving.
Full clinical nutrition clinical care guidelines and further information from ASPEN can be viewed at www.nutritioncare.org