ICU Management & Practice, Volume 23 - Issue 5, 2023
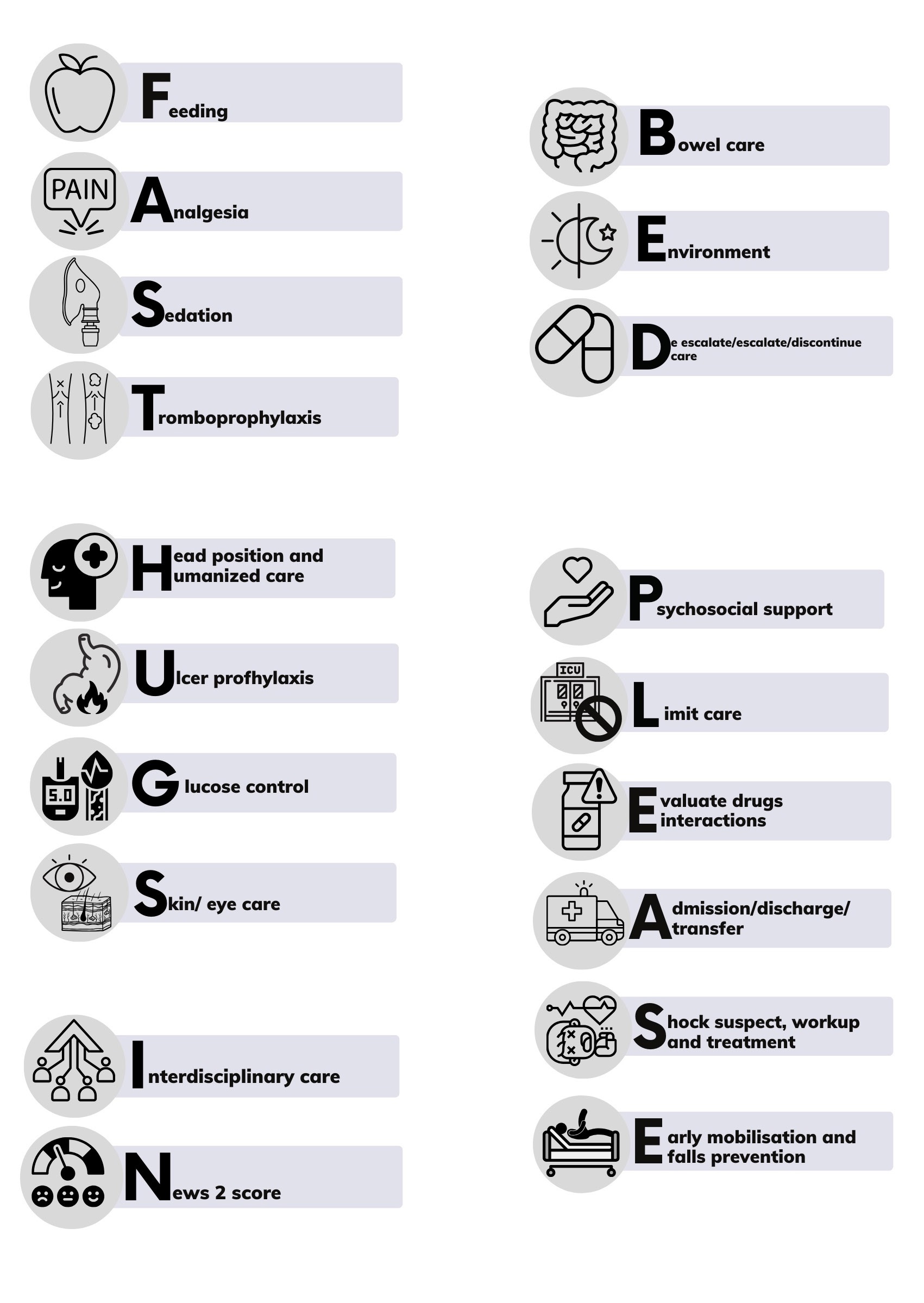
In the ICU, providing better care with less is the holy grail. This mnemonic tries to resume a list of the key interventions for human, evidence-based and patient-centred care.
Background
In 2005, Prof Jean-Louis Vincent introduced the mnemonic "FAST HUG," advocating for a comprehensive approach to patient care encompassing seven key components: Feeding, Analgesia, Sedation, Thromboembolic prevention, Head-of-bed elevation to 30-45°, stress Ulcer prophylaxis, and Glucose control (Vincent 2005). This paradigm shift has had a profound impact within the critical care domain, fostering a patient-centred approach that prioritises mental well-being, reduces invasive interventions, and promotes judicious fluid management.
Subsequently, in 2009, William Vincent and Kevin Hatton refined the mnemonic to "FAST HUGS BID", tailoring it for surgical patients. This expanded version incorporates additional elements: Fluid management, consideration of Spontaneous breathing trials, meticulous Bowel care, timely removal of Indwelling catheters, and prudent De-escalation of antibiotic use (Vincent and Hatton 2009).
In a more contemporary context, 2021 saw Chris Nickson's contribution through the "Life in the Fast Lane" blog, wherein the mnemonic was further enhanced to "FAST HUGS IN BED Please". This iteration takes into account the intricacies of care in the emergency department, encompassing Fluid therapy and Feeding; Adequate Analgesia, administration of Antiemetics, and provision of Diphtheria booster/vaccine; thoughtful Sedation and consideration of Spontaneous breathing trials; Thromboprophylaxis measures; Tetanus prophylaxis; Head elevation (30°) for intubated patients; proactive Ulcer prophylaxis; vigilant Glucose control; thorough Skin and Eyecare, along with proper suctioning; management of Indwelling catheters; Nasogastric tube maintenance; meticulous Bowel care; Environment optimisation (including temperature control and conducive surroundings for delirium management); De-escalation strategies (pertaining to end-of-life decisions and cessation of unnecessary treatments); and comprehensive Psychosocial support for patients, families, and staff (Nickson 2021). This updated rendition provides a more encompassing framework, rendering it a highly practical tool. Within our medical practices, it has been embraced across the spectrum - from the intensive care unit to the emergency department and hospital wards.
Administering Care to Critically Ill Patients with FAST HUGS IN BED PLEASE
We present a revised iteration of the mnemonic, incorporating often overlooked aspects:
F: Feeding
Conduct a thorough nutritional assessment and provide support as required. Emphasise the importance of adequate nourishment, as prolonged fasting can detrimentally impact outcomes. Even in surgical scenarios, short fasting is the prevailing practice. In the emergency department, proactive measures can be taken to ensure meal provision and, if necessary, consultation with nutrition specialists for patients with specific needs such as diabetes, hypermetabolic conditions (e.g., burns, hyperthyroidism), or malnutrition (Compher et al. 2022). Comprehensive nutritional evaluation and suitable oral or enteral diets are advantageous for critically ill and most hospitalised patients, with parenteral routes reserved for select cases (Weimann et al. 2021; Singer et al. 2019).
A: Analgesia and Antiemetic Agents
Pain management ranks among the prime concerns for patients seeking medical attention. Systematic pain assessment, regardless of intubation status, should be undertaken employing validated scoring systems such as the critical care pain observation tool (CPOT) or the behavioural pain scale (BPS). Effective analgesia markedly influences the perception of care quality and enhances outcomes across a spectrum of cases, ranging from minor bruises to postsurgical and critically ill ventilated patients. Optimal approaches encompass a blend of opioid and non-opioid agents, including acetaminophen, non-steroidal anti-inflammatory drugs (NSAIDs), antineuritic medications, and, where applicable, interventional analgesic techniques (Devlyn 2018). Antiemetic agents such as ondansetron or alcohol in cotton swabs can be contemplated for patients grappling with nausea triggered by analgesic use or underlying medical conditions.
S: Sedation and Spontaneous Breathing Trial
Administer sedation only as necessary and strive for prompt withdrawal. Prioritise optimal analgesia and anxiolysis, favouring short-acting medications over benzodiazepines. Caution should be exercised with agents like propofol and dexmedetomidine (Escamilla et al. 2022; Narayan and Petersen 2022). Incorporating awakening and spontaneous breathing trials into the care regimen is pivotal, especially for mechanically ventilated patients whose intubation cause is controlled. These interventions contribute to a judicious balance between patient comfort and their progression towards self-regulated respiration.
T: Thromboprophylaxis
Thromboembolic occurrences persist as significant contributors to morbidity and mortality within the inpatient setting. Utilising scoring systems such as Caprini and Padua offers insights to tailor optimal prophylactic strategies for each individual. From early mobilisation to employing parenteral thromboprophylactic agents like enoxaparin or compression pneumatic stockings, tailored approaches are pivotal. Specialised evaluation considering orthopaedic, cancer, autoimmune, critically ill, and surgical contexts play a pivotal role in averting thromboembolic complications. Recognising that a universal approach doesn't suffice, it becomes imperative to individualise interventions for enhanced efficacy (Sebaaly and Covert 2018; Amer et al. 2023).
H: Head Position and Humanised Care
Adapting the head position to suit individual needs is paramount. Varied positions offer unique benefits, and even a single patient can derive advantage from different orientations at distinct phases of care. Meticulous assessment and adherence to guidelines not only enhance patient comfort but also ensure their safety. Individuals vulnerable to or exhibiting cranial hypertension, particularly those on mechanical ventilation, may find positioning at an incline of 35-45° advantageous (Maschmann et al. 2019; Dabrowski et al. 2021). Humanised care and improving communication can empower the patient and family and promote personal care and hygiene. The use of hearing aids, glasses, and dentures are feasible and established recreation strategies (Wilson et al. 2019).
U: Ulcer Prophylaxis
Gastrointestinal ulcer prophylaxis, while not linked to reduced mortality, effectively mitigates the risk of gastrointestinal bleeding. Indications for commencing prophylaxis should encompass patients enduring positive pressure ventilation exceeding 48 hours, those reliant on extracorporeal life support, individuals with a platelet count below 50x10^9/L, INR surpassing 1.5, aPTT exceeding twice the norm, history of recent gastrointestinal bleeding within the past year, acute traumatic brain injury or spinal cord injury, and substantial thermal injuries covering more than 35% of total body surface area (Saeed 2022). The early initiation of enteral nutrition, even in the presence of significant risk factors, contributes to reducing the likelihood of gastrointestinal bleeding, while the incorporation of proton pump inhibitors (PPIs) brings benefits to the aforementioned patient groups (El-Kersh et al. 2018).
G: Glucose Control
The ADA annually publishes guidelines that outline glucose thresholds for hospitalised patients. These recommendations categorise patients based on their vulnerability to hypoglycaemia and hyperglycaemia. Adherence to these guidelines, combined with vigilant management of glucose fluctuations, places significant emphasis on preventing hypoglycaemia while concurrently addressing hyperglycaemic episodes. This approach yields positive outcomes by substantially reducing the risks of morbidity and mortality, including conditions like decompensation, infections, and electrolyte imbalances. Integrating nutritional and rehabilitative interventions further enhances control by considering energy provision and anticipated expenditure (American Diabetes Association 2023). It's noteworthy that while insulin is commonly used to manage hospital hyperglycaemia, euglycaemic agents such as metformin and GLP-1 receptor agonists can also prove valuable.
S: Skin/Eye Care
Dermatological complications often emerge during hospitalisation, contributing to significant morbidity even if not typically life-threatening. Manifestations like pressure sores, intertrigo, and symmetrical peripheral gangrene underscore the importance of skin and eye care. Additionally, careful skin evaluation can aid in the identification of adverse drug reactions (Bromley et al.ulcers, which pose a significant challenge for immobilised patients. Implementing standardised prevention protocols involving healthcare professionals across the spectrum, from doctors to auxiliary staff, is essential to mitigate this concern (Mervis and Phillips 2019). Simultaneously, ocular health demands attention, with corneal epithelial defects occurring in 20-42% of ICU patients. Impaired tear production and reduced blinking heighten the risk of eye injury. The adoption of standardised eye care protocols has demonstrated efficacy in reducing complication rates and safeguarding ocular health (Hearne et al. 2018).
I: Interdisciplinary Care
Specialised care administered by interdisciplinary teams comprising doctors, nurses, pharmacists, physical therapists, and nutritionists yields improved patient outcomes. Contrasting the multidisciplinary approach, where specialists operate within their defined domains, the interdisciplinary model orchestrates comprehensive patient assessment and synthesis of information to devise a unified and cohesive care strategy (Choi et al. 2006). Central to this approach is the collaboration of diverse specialists who collectively scrutinise patient cases. This cohesive teamwork enables the creation of a comprehensive care plan, encompassing inputs from all relevant disciplines (Giusti et al. 2017). The value of early engagement with suitable specialists cannot be overstated. Prompt consultations expedite interventions when required. For instance, infectious disease consultations have demonstrated their capacity to reduce mortality rates in both critically ill and non-critically ill patients within the intensive care unit (Jiménez et al. 2019). Similarly, oncology team involvement coupled with general surgery consultations has proven instrumental in enhancing long-term outcomes for patients newly diagnosed with cancer (Hujits et al. 2021; Butt et al. 2015). By embracing an interdisciplinary approach, healthcare teams synergise their expertise to provide holistic, timely, and tailored care, thereby augmenting patient well-being and treatment efficacy.
N: NEWS2 Score
The implementation of early warning systems, exemplified by the NEWS2 score, holds a pivotal role within hospital settings, functioning akin to a triage mechanism. As patients traverse their hospital journey, these systems adeptly detect shifts in their clinical trajectory, facilitating timely adjustments in the level of care, including potential transfer to the ICU. Moreover, they serve as triggers for rapid response teams to promptly address critical situations, thereby substantially elevating patient safety and overall outcomes (Scott et al. 2020). The integration of specialised rapid response teams, accompanied by tailored protocols, emerges as a cornerstone for bolstering adherence to standardised procedures. This concerted effort yields a marked enhancement in clinical outcomes across a spectrum of medical domains. Illustrative examples encompass sepsis, myocardial infarction, obstetric emergencies, paediatric crises, respiratory complications, and both ischaemic and haemorrhagic strokes (Girotra et al. 2022). Through such deliberate implementation, hospitals cultivate an environment characterised by efficient and coherent responses, culminating in a pronounced enhancement of patient well-being.
B: Bowel Care
Comprehensive bowel care necessitates evaluating the suitability of oral or enteral routes for medication and diet tailored to individual needs and circumstances. Rigorous monitoring of bowel movements and assessment of stool characteristics are paramount, accompanied by proactive management of constipation or diarrhoea. Should concerns arise regarding intrabdominal pressure, its measurement assumes significance while mitigating the potential risks associated with bacterial translocation (Bowel Care in Critical Care 2020).
E: Environment
Crafting a conducive environment holds pivotal importance in ensuring patient comfort. Sustaining an appropriately warm room temperature fosters well-being. Meticulous modulation of light and noise, aligned with circadian rhythms, alongside regulated exposure to natural sunlight, establishes essential day-night routines. Frequent reorientation, active family engagement, and accessible critical care spaces coalesce to avert delirium, resulting in heightened patient perception of quality and enhanced clinical outcomes (Saran et al. 2020; Horsten et al. 2018).
D: De-escalate/Escalate/Discontinue Care (Chronic and Acute Treatments)
The timely initiation of antibiotics, especially in cases of sepsis, is paramount. Innovative microbiological molecular diagnostics implemented within the initial hours can inform judicious antibiotic use, given their ability to provide insights into resistance genes. Swift and aggressive control of the infection source significantly enhances patient outcomes. Subsequent adjustment or discontinuation, guided by culture antibiograms and protein C and procalcitonin levels, facilitates the reduction of antibiotic usage, consequently diminishing the risk of resistant infections and overexposure. This approach leads to a reduction in ICU and hospital stays (Honda et al. 2010; Butt et al. 2015). For vasopressors, mechanical ventilation, sedation, and all therapeutic agents, a careful evaluation is imperative to determine the continuation, adjustment, or discontinuation of IV lines based on the patient's clinical status and prognosis. Peripheral lines can often suffice for patients who require IV treatment, while peripheral-inserted central catheters (PICCs) are suitable for prolonged therapies. Central venous access, which is reserved for specific cases, serves as an option for drugs that can damage vessels or involve high osmolarity solutions. The use of ultrasound guidance should be emphasised for both central and peripheral venous access. It's critical to limit unnecessary central access, as even peripheral lines benefit from ultrasound-guided insertion. Implementing catheter clinics specialising in complications prevention not only enhances outcomes but also curtails morbidity, underscoring the importance of prompt line removal (Lakbar et al. 2020). Invasive devices, including extracorporeal support, Foley catheters, and nasogastric tubes, should be promptly removed once their necessity diminishes. This approach aligns with the principle of minimising unnecessary interventions, a practice that improves patient outcomes and reduces complications (Benjamin et al. 2017; Nollen et al. 2023).
P: Psychosocial Support
Providing comprehensive psychosocial support, encompassing patients, families, and staff, is a fundamental aspect that extends to the implementation of a standardised suicide protocol. The hospital environment frequently witnesses challenges of anxiety and depression among patients, particularly those facing prolonged stays, issues such as stomas, limb amputations, disabilities, and chronic or catastrophic diseases. Swift intervention from mental health specialists proves pivotal, enhancing patient outcomes and well-being. For critically ill patients, vigilant depression screening is essential, considering its significant prevalence (Fernando et al. 2022). The establishment of a suicide protocol represents a crucial step towards rendering holistic care for individuals with suicidal tendencies. This protocol should extend its reach to encompass the mental well-being of the patient's family. Regrettably, such events can also impact hospital staff, making their mental health equally relevant. The comprehensive approach underscores the interconnectedness of well-being within the hospital environment, embracing patients, families, and staff alike (Liao et al. 2020).
L: Limiting Care
In some instances, patients may reach a stage where the benefits of ICU or hospital care are limited. Acknowledging this juncture is crucial, enabling open discussions among the medical team and family to navigate end-of-life considerations. At this stage, palliative measures such as benzodiazepines and opioids can be employed to provide comfort and ease symptoms associated with the advanced disease stage. This compassionate approach encompasses the physical and emotional well-being of the patient, ensuring a dignified and supportive transition (Nieto et al. 2015).
E: Evaluate Drug Interactions and Avoid Potentially Inappropriate Medications
Vigilantly assessing drug interactions and steering clear of potentially inappropriate medications is a critical aspect of patient care. Conducting medication reconciliation yields multifaceted benefits, not only curbing secondary hospital-related morbidity but also curtailing the length of stay and associated costs. Continuation of chronic drug regimens serves to prevent decompensation in patients with chronic illnesses, further underlining its significance (Bosma et al. 2018). Medication reconciliation is pivotal in averting drug interactions and potential adverse effects, translating into a reduction in secondary hospital-associated complications, thereby curbing the length of stay and expenses. Ensuring the continuation of chronic medications is instrumental in preventing the exacerbation of chronic illnesses (Nieto et al. 2015). In specific circumstances, the ongoing use of chronic treatments may be deemed appropriate, while in other cases, adjustment might be necessary even if the treatment isn't directly linked to the primary cause of hospitalisation. For example, anticoagulation drugs, antibiotics, immunosuppressants, antihypertensives, and thyroid medication could necessitate adaptation when a patient is dealing with severe illness or undergoing major surgeries. Similarly, diabetes medication generally remains suitable for most patients, although it may require modification to ensure optimal management during the hospital stay. This tailored approach to medication management ensures that patient health and safety are upheld in diverse clinical scenarios. Detecting medications that are contraindicated for a patient is feasible, particularly in the geriatric population. Beer's criteria, STOPP/V2, or EU(7) protocols can be referenced to identify inappropriate medications (Wilson et al. 2019). This conscientious approach to medication management enhances patient safety and well-being.
A: Admission/Discharge/Transfer
The emergency department often presents an environment conducive to delirium, characterised by noise, constant illumination, high activity levels, and occasional chaos. Timely admission is crucial as delaying it can heighten the risk of delirium, especially in predisposed patients. Similarly, delaying discharge can lead to anxiety and discomfort due to the same environmental factors while also potentially congesting patient flow within the emergency department. Transferring patients to specialised units promptly has been shown to enhance outcomes, particularly evident in cases of acute myocardial infarction, stroke, cerebral haemorrhage, or severe trauma (Rosa et al. 2020; Yang et al. 2016; Escamilla et al. 2022).
S: Shock (Suspect, Workup, and Treatment)
Early detection of severe conditions is pivotal to ensure optimal care delivery. Adhering to current treatment recommendations not only improves outcomes but also curtails hospitalisation days and resource utilisation. The various types of shock—septic, hypovolaemic (haemorrhagic and non-haemorrhagic), obstructive, cardiogenic, and distributive (metabolic, toxic, medullary, neurogenic, anaphylactic)—all necessitate specific workups and tailored treatments. However, accurate suspicion and confirmation of shock are imperative to initiate these targeted interventions. (Narayan et al. 2022).
E: Early Mobilisation and Falls Prevention
Commencing early rehabilitation from day one proves instrumental in bolstering muscle strength and facilitating early mobilisation. This practice not only diminishes the risk of delirium but also mitigates the likelihood of deep vein thrombosis (DVT), thereby contributing to reduced ICU and hospital stays. Furthermore, it aids in facilitating successful weaning and enhancing discharge outcomes (Menges et al. 2021). Implementation of standardised protocols for fall prevention is pivotal. This encompasses comprehensive patient and family education, provision of anti-slip shoes, execution of transfer protocols involving specialised technicians, and even the incorporation of bed sensors for high-risk patients. Such a multifaceted approach effectively minimises the risk of falls, spanning from the emergency department to the discharge phase (Benjamin et al. 2017).
Conclusion
The critical care unit demands a patient-centred approach that extends beyond addressing the disease itself, encompassing the holistic well-being of the individual. Embracing the key principles highlighted in this mnemonic aids in streamlining care, minimising unnecessary interventions, and maximising beneficial outcomes. Keeping these essential pearls in mind during medical rounds serves to curtail oversights and avoid undue interventions. In today's medical practice, the adage "less is more" rings true, underlining the significance of discontinuing treatments and removing invasive devices once they no longer contribute to patient well-being. By adhering to this principle, positive outcomes are paralleled in their impact to that of timely interventions. Refraining from initiating unnecessary treatments bears the potential to avert complications, shorten ICU or hospital stays, and enhance patient recovery. It is essential to recognise that this mnemonic functions not as a prescriptive "to-do" list but as a gentle reminder to consider the unique needs and circumstances of each patient. The aim is to foster a comprehensive and personalised approach to care that optimises patient outcomes and well-being.
Acknowledgements
We would like to extend our heartfelt gratitude to Prof Jean-Louis Vincent for his daily inspiration in the management of critical patients. His contributions have greatly enriched our understanding and approach to medical care. We would also like to thank Heber Alejandro Pérez-Arreguin for his valuable ideas and insights.
Conflict of Interest
None.
References:
Alarcon JD, Rubiano AM, Okonkwo DO et al. (2017) Elevation of the head during intensive care management in people with severe traumatic brain injury. Cochrane Database Syst Rev. 12(12):CD009986.
Al-Awad NI, Wosomu L, Al Hassanin EA et al. (2000) Immediate discontinuation of intravenous fluids after common surgical procedures. J Family Community Med. 7(1):69-73.
Al Kadri HM (2010) Obstetric medical emergency teams are a step forward in maternal safety! J Emerg Trauma Shock. 3(4):337-341.
Amer M, Alshahrani MS, Arabi YM et al. (2023) Saudi Critical Care Society clinical practice guidelines on the prevention of venous thromboembolism in adults with trauma: reviewed for evidence-based integrity and endorsed by the Scandinavian Society of Anesthesiology and Intensive Care Medicine. Ann Intensive Care. 13(1):41.
American Diabetes Association. Standards of Care in Diabetes (2023) Abridged for Primary Care Providers [published correction appears in Clin Diabetes. 41(2):328]. Clin Diabetes. 41(1):4-31.
Bassett R, Adams KM, Danesh V et al. (2015) Rethinking critical care: decreasing sedation, increasing delirium monitoring, and increasing patient mobility. Jt Comm J Qual Patient Saf. 41(2):62-74.
Benjamin E, Roddy L, Guiliano KK (2017) Management of patient tubes and lines during early mobility in the intensive care unit. Human Factors in Healthcare. 2.
Bennett EE, VanBuren J, Holubkov R et al. (2018) Bratton SL. Presence of Invasive Devices and Risks of Healthcare-Associated Infections and Sepsis. J Pediatr Intensive Care. 7(4):188-195.
Best Practice Guidance – Bowel Care in Critical Care (2020) Collaborative Regional Benchmarking Group.
Bluestein D, Javaheri A (2008) Pressure ulcers: prevention, evaluation, and management. Am Fam Physician. 2008;78(10):1186-1194.
Bosma LBE, Hunfeld NGM, Quax RAM et al. (2018) The effect of a medication reconciliation program in two intensive care units in the Netherlands: a prospective intervention study with a before and after design. Ann Intensive Care. 8(1):19.
Bromley M, Marsh S, Layton A (2021) Dermatological complications of critical care. BJA Educ. 21(11):408-413.
Butt AA, Al Kaabi N, Saifuddin M et al. (2015) Impact of Infectious Diseases Team Consultation on Antimicrobial Use, Length of Stay and Mortality. Am J Med Sci. 350(3):191-194.
Carpenter CR, Hammouda N, Linton EA et al. (2021) Delirium Prevention, Detection, and Treatment in Emergency Medicine Settings: A Geriatric Emergency Care Applied Research (GEAR) Network Scoping Review and Consensus Statement. Acad Emerg Med. 28(1):19-35.
Choi BC, Pak AW (2006) Multidisciplinary, interdisciplinarity and transdisciplinary in health research, services, education and policy: 1. Definitions, objectives, and evidence of effectiveness. Clin Invest Med. 29(6):351-364.
Compher C, Bingham AL, McCall M et al. (2022) Guidelines for the provision of nutrition support therapy in the adult critically ill patient: The American Society for Parenteral and Enteral Nutrition [published correction appears in JPEN J Parenter Enteral Nutr. 46(6):1458-1459]. JPEN J Parenter Enteral Nutr. 46(1):12-41.
Dabrowski W, Siwicka-Gieroba D, Robba C et al. (2021) The prone position must accommodate changes in IAP in traumatic brain injury patients. Crit Care. 25(1):132.
Darbyshire JL, Müller-Trapet M, Cheer J et al. (2019) Mapping sources of noise in an intensive care unit. Anaesthesia. 74(8):1018-1025.
Devlin JW, Skrobik Y, Gélinas C et al. (2018) Clinical Practice Guidelines for the Prevention and Management of Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption in Adult Patients in the ICU. Crit Care Med. 46(9):e825-e873.
Earle CC, Schrag D, Neville BA et al. (2006) Effect of surgeon specialty on processes of care and outcomes for ovarian cancer patients. J Natl Cancer Inst. 98(3):172-180.
El-Kersh K, Jalil B, McClave SA et al. (2018) Enteral nutrition as stress ulcer prophylaxis in critically ill patients: A randomized controlled exploratory study. J Crit Care. 43:108-113.
Escamilla-Ocañas CE, Torrealba-Acosta G, Mandava P et al. (2022) Implementation of systematic safety checklists in a neurocritical care unit: a quality improvement study. BMJ Open Qual. 11(4):e001824.
European Medicines Agency (2022). Dexmedetomidine: Increased risk of mortality in intensive care unit (ICU) patients ≤65 years. Available at https://www.ema.europa.eu/en/medicines/dhpc/dexmedetomidine-increased-risk-mortality-intensive-care-unit-icu-patients-65-years
Fernando SM, Qureshi D, Sood MM et al. (2021)
Suicide and self-harm in adult survivors of critical illness: population based
cohort study. BMJ. 2021;373:n973.
Fernando SM, Ranzani OT, Herridge MS (2022) Mental health morbidity, self-harm, and suicide in ICU survivors and caregivers. Intensive Care Med. 48(8):1084-1087.
Gitti N, Renzi S, Marchesi M et al. (2022) Seeking the Light in Intensive Care Unit Sedation: The Optimal Sedation Strategy for Critically Ill Patients. Front Med (Lausanne). 9:901343.
Girotra S, Jones PG, Peberdy MA et al. (2022) Association of Rapid Response Teams With Hospital Mortality in Medicare Patients. Circ Cardiovasc Qual Outcomes. 15(9):e008901.
Giusti EM, Castelnuovo G, Molinari E (2017) Differences in Multidisciplinary and Interdisciplinary Treatment Programs for Fibromyalgia: A Mapping Review. Pain Res Manag. 7261468.
Hearne BJ, Hearne EG, Montgomery H, Lightman SL (2018) Eye care in the intensive care unit. J Intensive Care Soc. 19(4):345-350.
Honda H, Krauss
MJ, Jones JC et al. (2010) The value of infectious diseases consultation in
Staphylococcus aureus bacteremia. Am J Med. 123(7):631-637.
Horsten S, Reinke L, Absalom AR, Tulleken JE (2018) Systematic review of the effects of intensive-care-unit noise on sleep of healthy subjects and the critically ill. Br J Anaesth. 120(3):443-452.
Huijts DD, Dekker JWT, van Bodegom-Vos L et al. (2021) Differences in organization of care are associated with mortality, severe complication and failure to rescue in emergency colon cancer surgery. Int J Qual Health Care. 33(1):mzab038
ICU admission linked to increased risk of future suicide and self-harm. (2021) BMJ. Available at https://www.bmj.com/company/newsroom/icu-admission-linked-to-increased-risk-of-future-suicide-and-self-harm/
Jamshidi R (2019) Central venous catheters: Indications, techniques, and complications. Semin Pediatr Surg. 28(1):26-32.
Jiménez-Aguilar P, López-Cortés LE, Rodríguez-Baño J et al. (2019) Impact of infectious diseases consultation on the outcome of patients with bacteraemia. Ther Adv Infect Dis. 6:2049936119893576.
Juneja D, Deepak D, Nasa P (2023) What, why and how to monitor blood glucose in critically ill patients. World J Diabetes. 14(5):528-538.
Lakbar I, De Waele JJ, Tabah A et al. (2020) Antimicrobial De-Escalation in the ICU: From Recommendations to Level of Evidence. Adv Ther. 37(7):3083-3096.
Liao KM, Ho CH,
Lai CC et al. (2020) The association between depression and length of stay in
the intensive care unit. Medicine (Baltimore). 99(23):e20514.
Maschmann C, Jeppesen E, Rubin MA, Barfod C (2019) New clinical guidelines on the spinal stabilization of adult trauma patients - consensus and evidence based. Scand J Trauma Resusc Emerg Med. 27(1):77.
Menges D, Seiler B, Tomonaga Y et al. (2021) Systematic early versus late mobilization or standard early mobilization in mechanically ventilated adult ICU patients: systematic review and meta-analysis. Crit Care. 25(1):16.
McPeake J, Gilmour H, MacIntosh G (2011) The implementation of a bowel management protocol in an adult intensive care unit. Nurs Crit Care. 16(5):235-242.
Mervis JS, Phillips TJ (2019) Pressure ulcers: Prevention and management. J Am Acad Dermatol. 81(4):893-902.
Moura Junior V, Westover MB, Li F et al. (2022) Hospital complications among older adults: Better processes could reduce the risk of delirium. Health Serv Manage Res. 35(3):154-163.
Narayan S, Petersen TL (2022) Uncommon Etiologies of Shock. Crit Care Clin. 38(2):429-441.
Nickson C (2021). FAST HUGS IN BED Please! Available at https://litfl.com/fast-hugs-in-bed-please/
Nieto-Guindo P, Martin A, Mateo-Carrasco H et al. (2015) PS-012 Medicines reconciliation in the intensive care unit. European Journal of Hospital Pharmacy: Science and Practice. 22:A146-A147.
Nollen JM, Pijnappel L, Schoones JW et al. (2023) Impact of early postoperative indwelling urinary cath
Ogundele O, Yende S (2010) Pushing the envelope to reduce sedation in critically ill patients. Crit Care. 14(6):339.
Patterson J, Dusenbury W, Stanfill A et al. (2023). Transferring Patients From a Primary Stroke Center to Higher Levels of Care: A Qualitative Study of Stroke Coordinators’ Experiences. Stroke: Vascular and Interventional Neurology. 3. 10.1161/SVIN.
Porter KM, Dayan AD, Dickerson S, Middleton PM (2018) The role of inhaled methoxyflurane in acute pain management. Open Access Emerg Med. 10:149-164.
Rapid Response Systems (2020) Daniel D, Helen H, Jacind Bunch, Ed Salazar, Ernesto Arriaga-Morales, Steven B, et. al. s.l. : Patient Safety Movement APSS.
Rosa RG, Falavigna M, Robinson CC et al. (2020) Early and Late Mortality Following Discharge From the ICU: A Multicenter Prospective Cohort Study. Crit Care Med. 48(1):64-72.
Saeed M, Bass S, Chaisson NF (2022) Which ICU patients need stress ulcer prophylaxis? Cleve Clin J Med. 89(7):363-367.
Saran S, Gurjar M, Baronia A et al. (2020) Heating, ventilation and air conditioning (HVAC) in intensive care unit. Crit Care. 24(1):194.
Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine (2023) Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine.
Scott LJ, Tavaré A, Hill EM et al. (2022) Prognostic value of National Early Warning Scores (NEWS2) and component physiology in hospitalized patients with COVID-19: a multicenter study. Emerg Med J. 39(8):589-594.
Sebaaly J, Covert K (2018) Enoxaparin Dosing at Extremes of Weight: Literature Review and Dosing Recommendations. Ann Pharmacother. 52(9):898-909.
Singer P, Blaser AR, Berger MM et al. (2019) ESPEN guideline on clinical nutrition in the intensive care unit. Clin Nutr. 38(1):48-79.
Sivaram CA, Jarolim D, Nasser A (1996) Collaboration between a referring hospital and a tertiary care center in improving the transfer process for cardiac patients. Jt Comm J Qual Improv. 22(12):795-800.
Vincent JL (2005) Give your patient a fast hug (at least) once a day. Crit Care Med. 2005 33(6):1225-9.
Vincent WR 3rd, Hatton KW (2009) Critically ill patients need "FAST HUGS BID" (an updated mnemonic). Crit Care Med. 37(7):2326-7.
Ventriglio A, Watson C, Bhugra D (2020) Suicide among doctors: A narrative review. Indian J Psychiatry. 62(2):114-120.
Weimann A, Braga M, Carli F et al. (2021) ESPEN practical guideline: Clinical nutrition in surgery. Clin Nutr. 40(7):4745-4761.
Wilson ME, Beesley S, Grow A et al. (2019) Humanizing the intensive care unit. Crit Care. 23(1):32.
Yang S, Wang Z, Liu Z et al. (2016) Association between time of discharge from ICU and hospital mortality: a systematic review and meta-analysis. Crit Care. 20(1):390.












