ICU Management & Practice, ICU Volume 12 - Issue 1 - Spring 2012
Introduction
Non-invasive ventilation (NIV) provides safe and effective assistance to patients with acute respiratory failure (ARF) from various causes (Garpestad et al. 2007). The main reason for applying NIV is to avoid the complications of endotracheal intubation, according to Evans et al. (2000). The ventilator setting generally used to apply NIV is Pressure Support Ventilation (PSV), delivered via an oronasal mask (Garpestad et al. 2007); however, the application of NIV through a mask can be complicated by other problems, causing discomfort such as major air leaks, eye irritation, skin breakdown and patient-ventilator asynchrony. Carlucci et al. (2001) reported that discomfort is one of the major determinants of NIV failure, therefore, in the past decade both researchers and manufacturers have been working to increase patient comfort during NIV, both by improving conventional interfaces and developing new interfaces, such as the helmet.
Advantages of Helmet Ventilation
The helmet, consisting of a transparent, latex-free, polyvinyl chloride (PVC) hood, joined by a plastic ring to a soft collar, has been proposed to deliver continuous positive airway pressure (CPAP) and NIV.
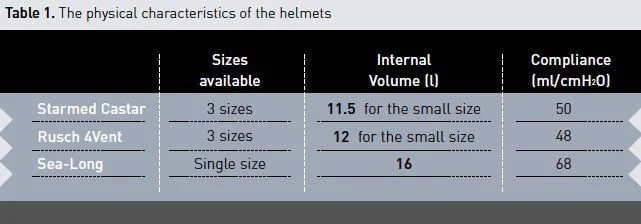
Several models of helmet with different designs and materials are available for clinical use: the Starmed Castar (Mirandola, Italy), the Rusch 4Vent (Mirandola, Italy), the Sea-Long (Louisville, Kentucky, USA), etc.
Helmet ventilation has the unique feature of avoiding direct contact with the facial skin. The lack of pressure points on the face increases patient comfort and reduces the risk of skin breakdown. In recent nonrandomised studies the helmet PSV ventilation method improved gas exchange with a better tolerance and a lower rate of complications than the mask PSV ventilation method, both in hypoxemic (Antonelli et. al 2002) and hypercapnic (Antonelli et. al 2004) ARF. It also increased the number of hours of continuous NIV use. Furthermore, the helmet can be applied to any patient regardless of their facial contour, decreasing air leaks and lowering nurse workload.
Disadvantages of Helmet Ventilation
The physical characteristics of the helmet (i.e. the large internal volume and the highly compliant soft collar: see Table 1) may over-damp the pressure rise inside the helmet itself, affect both the inspiratory trigger and the inspiration-to-expiration switch algorithms of the ventilator, and favour carbon dioxide (CO2) accumulation, leading to patient-ventilator asynchrony, impaired unloading efficacy of the respiratory muscles, and CO2 re-breathing (Racca et al. 2005; Costa et al. 2005; Taccone et al. 2004).
Patient-Ventilator Asynchrony
The inspiratory flow inside the helmet exceeds more than threefold the subject’s inspiratory flow (Racca et al. 2005). Because the algorithms regulating the beginning and end of PSV are pressure and flow based, an influence of the helmet’s characteristics on the ventilator triggering functions should be expected. Moreover, the highly compliant soft collar over-damps the pressure rise inside the helmet. Indeed, Racca et al. (2005) and Navalesi et al. (2007) have shown that:
1) The inspiratory trigger delay was significantly higher during helmet ventilation than during mask ventilation, indicating that the helmet has poor trigger sensitivity;
2) The speed of pressurisation was significantly lower during helmet ventilation than during mask ventilation;
3) The ventilator assistance was cycled off by the changes in flow caused by the mechanical characteristics of the helmet rather than by the changes in flow caused by the subject’s mechanical characteristics and muscle effort; thus, the termination of ventilator support could anticipate or follow the termination of the subject’s inspiratory effort; and
4)Wasted efforts and autocycled breaths occurred more frequently with the helmet ventilation than with the oronasal mask.
A comparative bench study carried out by Costa et al. (2008) suggested that different types of helmet may perform differently in delivering PSV.
Impaired Unloading Efficacy of the Respiratory Muscles
Some studies found the helmet to be less efficient than the mask in reducing inspiratory effort (Racca et al. 2005; Navalesi et al. 2007). Indeed, a substantial portion of the inspiratory flow serves to expand the helmet, whose large inner volume and high compliance lead to dissipation of the inspiratory pressure delivered by the ventilator. Moreover, during helmet ventilation, subjects had to double minute ventilation to maintain values of end-tidal PCO2 similar to those observed during mask ventilation (Racca et al. 2005). Finally, some portion of inspiratory effort is unassisted by the positive pressure boost delivered by the ventilator because of patient- ventilator uncoupling (Racca et al. 2005; Navalesi et al. 2007)
CO2 Rebreathing
There exists some concern about CO2 rebreathing during helmet application: with every breath, the CO2 expired by the patient does not completely leave the system, but partly dilutes within the internal volume of the helmet and is subsequently re-inhaled. As a matter of fact, for patients with acute exacerbations of chronic obstructive pulmonary disease, the helmet was less efficient than the face mask in CO2 elimination, identified Antonelli et al. (2004). Recently, Taccone et al. (2004) and Mojoli et al.(2008) demonstrated that during both CPAP and NIV delivered by helmet, the magnitude of rebreathing is directly related to the patient’s CO2 production and inversely related to the total flow passing through the helmet. Therefore, it has been suggested that only the helmet with high (40 to 60 L/min) continuous-flow CPAP systems be used (Taccone et al. 2004). However, in contrast to CPAP, during NIV the fresh gas flow applied to the helmet is limited (i.e. it is always lower than 40 L/min) and typically intermittent, leading to significant CO2 rebreathing (Racca et al. 2005).
Possible Solutions
Specific Ventilator Settings
All the physiologic studies comparing the helmet and the mask were performed using the same ventilator settings for the two interfaces. Recently, a study conducted by Vargas et al. (2009) and Costa et al. (2010) noted a significant improvement in patient–ventilator interaction and patient tolerance when delivering helmet PSV ventilation with specific settings.
Vargas et al. (2009) applied helmet PSV to patients requiring early NIV after extubation, increasing by 50% the baseline inspiratory and expiratory pressures used to deliver NIV through the oronasal mask, and applying the fastest pressurisation rate. They observed that, when used with specific settings, helmet PSV provided similar unloading to mask PSV and improved the inspiratory triggering delay. These results were attributed to an improved pressure and flow transmission, and lower helmet compliance due to higher positive end-expiratory pressure (PEEP).
Cycling off the ventilator is also an important component of the synchrony between the patient and the ventilator. In a physiological study, Costa et al.(2010) showed that the choice of a fast inspiratory ramp and a fast expiratory trigger (i.e. a cycling-off threshold of 60% of the peak inspiratory flow) can improve patient– ventilator interaction, especially when there is a high respiratory rate (RR).
In a recent paper, Mojoli et al. (2008) showed that CO2 rebreathing can be lowered during helmet ventilation by increasing inspiratory pressure or adding a flowby (i.e., a flow-by of 8-L/min). Indeed, these ventilator manipulations produced a progressive increase in the minute ventilation of the whole system.
Using a different ventilator modality such as biphasic positive airway pressure (BIPAP) results in further improvements, indicated Racca et al. (2009). Helmet BIPAP provided by ICU ventilators was successfully used as an alternative to helmet PSV in neuromuscular patients. Here, helmet PSV caused significant patient-ventilator asynchrony, leading to NIV intolerance. Thus, the ventilator was switched to helmet BIPAP with a RR and Ti set as close as possible to patient’s RR and timing. This ventilator setting improved gas exchange and patient-ventilator interaction, allowing successful NIV.
Finally, Isgrò et al. (2010) applied periodical high pressure breaths (SIGH) during helmet CPAP in patients with acute ARF, using a recently developed electromechanical expiratory valve, which is time cycled between two customisable PEEP levels. When compared to basal CPAP, SIGH induced a further significant increase in partial pressure of oxygen (PaO2).
Neural Triggered Helmet Ventilation
An evaluation by Sinderby et al. (1999) concluded that new methods for neural triggering and cycling-off, using the diaphragm electrical activity (EAdi), can be used to initiate and terminate ventilatory assistance in synchrony with inspiratory efforts. Measurement of the EAdi requires that a catheter be inserted transnasally into the stomach. Because the ventilator is directly triggered by EAdi, the synchrony between neural and mechanical inspiratory time is guaranteed both at the onset and at the end of inspiration, regardless of the physical characteristics of the helmet. Indeed, Moerer et al. (2008) demonstrated in healthy subjects that patient–ventilator synchrony, trigger effort, and breathing comfort with a helmet interface are considerably less impaired during increasing levels of PSV and RR, and with neural triggering and cycling-off, compared to conventional pneumatic triggering and cycling- off. However, adding an oesophageal catheter is uncomfortable and this insertion could be difficult in patients with ARF. Furthermore, several doubts remain regarding the long-term stability of the EAdi signal during NIV.
The New Helmet
Researchers and manufactures are working to develop a new helmet. A decrease of the inner volume and/or use of less compliant materials should be made in order to improve patient-ventilator synchrony and the unloading efficacy of respiratory muscles during helmet ventilation.
Conclusion
Although, we believe that the helmet can completely replace the mask to apply CPAP, its use for application of NIV should, at present, only be recommended as part of a rotating strategy of different interfaces in order to reduce NIV side effects and allow NIV application for a higher number of continuous hours, primarily in hypoxemic patients. It is also worth highlighting the need to increase the value of inspiratory and expiratory pressure, and to choose a fast inspiratory ramp and a fast expiratory trigger when switching from the mask to the helmet. Should helmet PSV failure occur, despite specific ventilator settings, BIPAP or neural triggered ventilation may be used to provide helmet ventilation.
References:
Antonelli M et al. New treatment of acute hypoxemic respiratory failure: Noninvasive pressure support ventilation delivered by helmet—A pilot controlled trial. Crit Care Med (2002); 30:602–608.
Antonelli M et al. Noninvasive positive pressure ventilation using a helmet in patients with acute exacerbation of chronic obstructive pulmonary disease: A feasibility study. Anesthesiology (2004); 100:16–24.
Carlucci A et al. Noninvasive versus conventional mechanical ventilation. An epidemiologic survey. Am J Respir Crit Care Med (2001); 167:874–880.
Costa R et al. Comparative evaluation of different helmets on patient–ventilator interaction during noninvasive ventilation Intensive Care Med (2008); 34:1102–1108.
Costa R et al. Influence of ventilator settings on patient–ventilator synchrony during pressure support ventilation with different interfaces Intensive Care Med (2010); 36:1363–1370.
Garpestad E et al. Noninvasive Ventilation for Critical Care. Chest (2007); 132:711–720
Evans TW. International Consensus Conferences in Intensive Care Medicine: Noninvasive positive pressure ventilation in acute respiratory failure. Intensive Care Med (2000); 27:166–178.
Isgrò S et al. Continuous flow biphasic positive air way pressure by helmet in patients with acute hypoxic respiratory failure: effect on oxygenation Intensive Care Med (2010);36:1688–1694.
Moerer O et al. Subject ventilator synchrony during neural versus pneumatically triggered non-invasive helmet ventilation. Intensive Care Med (2008); 34:1615–1623 .
Mojoli F et al. Carbon dioxide rebreathing during non-invasive ventilation delivered by helmet: a bench study. Intensive Care Med (2008); 34:1454-1460.
Navalesi P et al. Noninvasive ventilation in chronic obstructive pulmonary disease patients: Helmet versus facial mask. Intensive Care Med (2007); 33:74–81.
Racca F et al. Effectiveness of mask and helmet interfaces to deliver noninvasive ventilation in a human model of resistive breathing. J Appl Physiol (2005); 99:1262–1271.
Racca F et al. Helmet ventilation for acute respiratory failure and nasal skin breakdown in neuromuscular disorders. Anesth Analg (2009); 109:164–167.
Sinderby C et al. Neural control of mechanical ventilation in respiratory failure. Nat Med (1999); 5:1433–1436.
Taccone P et al.. Continuous positive airway pressure delivered with a "helmet": effects on carbon dioxide rebreathing. Crit Care Med. (2004); 32(10):2090-6.
Vargas F et al. Helmet with specific settings versus facemask for noninvasive ventilation. Crit Care Med (2009); 37:1921–1928.