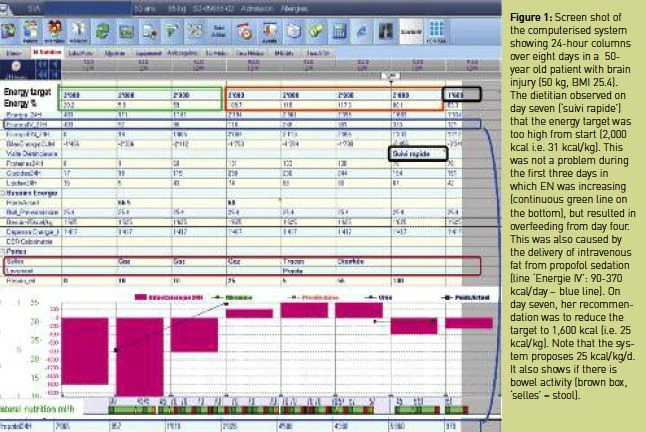
ICU Management & Practice, ICU Volume 12 - Issue 1 - Spring 2012
Many experts have shown that nutritional therapy improves intensive care unit (ICU) outcomes. In particular, the use of early enteral nutrition (EN), as recommended by ESPEN guidelines (2006), is associated with a reduction in mortality in the sickest patients (Artinian et al. 2006). Paradoxically, enteral feeding is most difficult to perform in the sickest patients, and several studies have revealed very slow progression with this form of feeding (Alberda et al. 2009; Finfer et al. 2009; Casaer et al. 2011). The difficulties encountered are maximal during the first week, putting these patients at high risk of undernutrition (Villet et al. 2005). Indeed, underfeeding is frequent in this population but should not be considered as a matter of fact. Many actions can be undertaken to improve nutrition care management and achieve important clinical improvements. The introduction of a nutrition protocol in the ICU belongs to this process, and integration of dietitians with specific training in the ICU contributes to quality of care improvements.
Improving Nutrition Therapy in the Critically Ill
Even if some data are controversial, the great majority of studies have observed an improvement in the quality of nutrition support provided when a protocol is in place, reflected by:
• Better adaptation of nutrition to patients’ needs (Heyland et al. 2004; Soguel et al. 2012);
• Higher rate of nutrition support (Doig et al. 2008; Soguel et al. 2012) or enteral nutrition (Barr et al. 2004);
• More early applications of enteral feeding and days on nutrition (Doig et al. 2008).
Findings with regard to the impact of feeding protocols on clinical evolution have been positive or neutral, with some studies reporting a beneficial impact on organ function (Doig et al. 2008), length of mechanical ventilation and ICU mortality (Barr et al. 2004), though no impact on length of ICU and hospital stay has been indicated (Barr et al. 2004; Doig et al. 2008; Longchamp et al. 2007).
Soguel et al. (2012) suggested that the positive impact of the protocol will be reinforced by the integration of a dietitian in the ICU team. Indeed, the presence or absence of a dietitian may even explain the different results between studies measuring the impact of a nutrition protocol implementation. To implement a protocol is challenging: when it is poorly practice integrated, it has limited effects (Longchamp et al. 2007; Soguel et al. 2012). The ICU dietitian will act as a facilitator by adapting guidelines to local practice, teaching staff, functioning as an opinion leader, and lowering barriers to protocol adherence (Jones et al. 2007).
Integration of a Dietitian in the ICU
Nowadays, ICU teams are multidisciplinary; the complexity of the patients requires manifold competences to improve metabolic therapy. Dietitians will support physicians and nurses in their daily practice and bring specific nutritional knowledge to discussions. They will especially be involved in patients with the most complex pathologies, applying numerous steps of care: nutrition assessment, diagnosis, intervention, monitoring and evaluation (American Dietetic Association 2008). Several actions can be undertaken by ICU dietitians, as indicated in Table 1. They will be involved in improving the overall quality of care through:
• Maintenance of knowledge and consistency in the care process, especially in teaching hospital ICU staff;
• Continuous adaptation of nutrition protocols in light of new evidence;
• Teaching and introducing practical tools; and
• Promotion of nutrition research.
To enable the benefits, clinical dietitians should be integrated into the daily routine of the unit. They will have to work very closely with other members of staff, particularly with those working at the bedside all day long.
Specific ICU Awareness Required by the Dietitian
Besides the specific nutrition competences that are part of dietitians’ pre- or post-grade education programmes, time for integration is required to become an efficient dietitian in the intensive care field. The critically ill patient is a highly complex entity, so coming from a dietetics initial education programme, it will take dietitians several weeks to get familiar with the challenges. Recognition of life-saving treatments and optimal intervention times is not easy. Impact of fluid balances, of vasoactive drugs, of sedatives on weight and gut function are very specific, as are those of an intense inflammatory response on all visceral proteins used for nutritional assessment. Every change from normal must be put into perspective, and specific requirements must all be integrated in order to respond with a clinically adapted proposal. Participation in multiple case discussions is crucial to develop these competences.
Economic Aspects
The presence of a dietitian in the ICU is considered as standard in some countries but is not yet generalised. The NHS in the UK made a staffing proposal but this has been poorly followed through, suggested Windle (2007). Salary costs are frequently considered an obstacle to hiring an ICU dietitian; administrators should be made aware that this is a truncated view of reality, forgetting the costs generated by poor nutrition support. The economic aspects of infectious complications prevention are not yet properly addressed. Both underand over-feeding cause increased infection rates and prolonged mechanical ventilation, generating very high costs: 32,254 US dollars per bloodstream infection (Kim et al. 2011) and 34 thousand US dollars per ventilator associated pneumonia (Zilberberg and Shorr 2011). The prevention of two to three costly bloodstream infections per year (Rubinson et al. 2004), the reduction by two to three days of intubation time, or the prevention of complications associated with the development of fatty liver, would easily pay the salary of the dietitian. Conversely, malnutrition has an important cost in the ICU, including after discharge, possibly resulting in further hospitalisation and rehabilitation, thus further costs.
Conclusion and Perspectives
Nutrition therapy is an important tool, which supports the success of other ICU therapies and should be assigned to a nutrition specialist who is integrated into the ICU team. It has been shown that the presence of a dietitian improves nutritional support, so this should play a part in modernising the working structure, as well as supporting increasingly exhausted staff. Furthermore, this presence should help to reduce staff’s uneasy feelings about nutrition competencies (Möwe et al. 2008).
References:
AMERICAN DIETETIC ASSOCIATION (ADA) (2008). Nutrition care process and model part I: the 2008 update. J Am Diet Assoc, 108:1113-7.
Alberda C et al. (2009). The relationship between nutritional intake and clinical outcomes in critically ill patients: results of an international multicenter observational study. Intensive Care Med, 35:1728-1737.
Artinian V et al. (2006). Effects of early enteral feeding on the outcome of critically ill mechanically ventilated medical patients. Chest, 129:960-967.
Barr J et al. (2004). Outcomes in critically ill patients before and after the implementation of an evidence-based nutritional management protocol. Chest, 125:1446-57.
Casaer MP et al. (2011). Early versus late parenteral nutrition in critically ill adults. N Engl J Med, 365:506-17.
Doig GS et al. (2008). Effect of evidence-based feeding guidelines on mortality of critically ill adults: a cluster randomized controlled trial. JAMA, 300:2731-41.
Finfer S et al. (2009). Intensive versus conventional glucose control in critically ill patients. N Engl J Med, 360:1283-97.
Heidegger CP et al. (2011). Supplemental parenteral nutrition (SPN) in intensive care unit (ICU) patients for optimal energy coverage: improved clinical outcome. Intensive Care Med, 37:S107.
Heyland DK et al. (2004). Validation of the Canadian clinical practice guidelines for nutrition support in mechanically ventilated, critically ill adult patients: results of a prospective observational study. Crit Care Med, 32:2260-6.
Jones NE et al. (2007). Implementation of the Canadian Clinical Practice Guidelines for Nutrition Support: a multiple case study of barriers and enablers. Nutr Clin Pract, 22:449-57.
Kim JS et al. (2011) Reduction of catheter-related bloodstream infections through the use of a central venous line bundle: epidemiologic and economic consequences. Am J Infect Control, 39:640-6.
Longchamp C et al. (2007). [Implementing a feeding protocol in an adult ICU (NUTSIA): success and pitfalls]. Rev Med Suisse, 3:2844-8.
Möwe M et al. (2008). Insufficient nutritional knowledge among health care workers? Clin Nutr, 27:196-202.
Rubinson L et al. (2004). Low caloric intake is associated with nosocomial bloodstream infections in patients in the medical intensive care unit. Crit Care Med, 32:350-7.
Soguel L et al. (2012). Energy deficit and length of hospital stay can be reduced by a two-step quality improvement of nutrition therapy: The intensive care unit dietitian can make the difference. Crit Care Med, 40:412-9.
Villet S et al. (2005). Negative impact of hypocaloric feeding and energy balance on clinical outcome in ICU patients. Clin Nutr, 24:502-9.
Windle EM (2007). Adequacy of dietetic service provision to adult critical care: a survey of 33 centres in Northern England. J Hum Nutr Diet, 20:111-9; quiz 119-20.
Zilberberg MD. and Shorr AF (2011). Ventilator-associated pneumonia as a model for approaching cost-effectiveness and infection prevention in the ICU. Curr Opin Infect Dis, 24:385-9.