ICU Management & Practice, Volume 21 - Issue 1, 2021
Impact of the Pandemic on Society
The 2019 Coronavirus Disease (COVID-19) pandemic has affected nearly all aspects of society, from family interactions to social activities to workplace structures. Travel restrictions and financial losses have fundamentally altered routine day-to-day undertakings for numerous businesses and millions of people. Standard practices have been altered in most large-scale enterprises, including healthcare.
Telemedicine is a Natural Fit for Remote Work
The use of telemedicine has accelerated at an unprecedented pace during the COVID-19 pandemic, primarily due to concerns regarding the safety of patients and their healthcare providers. In the larger society, where travel restrictions and policies to reduce person-to-person contact have been implemented to limit disease transmission, many activities have moved to an online environment, including standard office work and schooling. In healthcare, telemedicine has been adopted during the COVID-19 pandemic to promote “contactless” care.
At Mayo Clinic, the sudden and unanticipated disruption of the health care delivery model at the onset of the COVID-19 pandemic resulted in a rapid acceptance of telemedicine by providers and patients (Temesgen et al. 2020). The large-scale transition to telemedicine happened in a matter of days and represented one of the most rapid transformations of healthcare in history.
Status of Telemedicine Leading up to the Pandemic
Prior to the COVID-19 pandemic, telemedicine solutions had been used as components of disaster responses for over 30 years. For example, the US National Aeronautics and Space Administration (NASA), which had a long history of remote biologic monitoring, utilised telemedicine technologies to assist in relief efforts following earthquakes in Mexico City in 1985 and Armenia in 1988 (Nicogossian and Doarn 2011). In the years that followed, international initiatives were launched to leverage telemedicine in disaster preparedness.
In 2017, the North Atlantic Treaty Organization (NATO) established a Multinational Telemedicine System (MnTS) for use in disaster management, which allows for medical specialists to engage in disaster response across national borders (Doarn et al. 2018). In 2020, with decades of foundational experience, COVID-19 enabled design of a National Emergency Tele-Critical Care Network (NETCCN). As conceived, NETCCN would assist health care providers, wherever they are located, by obtaining real-time patient and supplies data, and by extending the reach of critical care specialists to areas of acute need (Scott et al. 2020).
Technological Enablers of Change and Barriers for Widespread Adoption
The American Telemedicine Association defines telemedicine (which is often used interchangeably with the term telehealth) as “the use of medical information, exchanged from one site to another via electronic communications, to improve patients’ health status". While this is a broad definition that could encompass phone calls or asynchronous uses of technology, the feature that truly distinguishes telemedicine from other remote health services is the presence of a real-time audiovisual communication tool that connects providers and patients across locations (Herasevich and Subramanian 2019). A second defining feature of telemedicine is the use of an electronic medical record (EMR) that offers remote providers access to patients’ clinical data. Tele-ICU comprises a subset of telemedicine, which may additionally include real-time remote access to monitoring tools and the ability to place orders remotely using Computerized Provider Order Entry (CPOE).
Advances in Tele-ICU have been intimately linked to advances in technology. The first use of a two-way audiovisual link in critical care was reported in 1977 (Grundy et al. 1977). However, it was not until 1997 that a practical use of telemedicine in ICU care was established, when a group of Johns Hopkins intensivists began monitoring a 10-bed surgical ICU in a hospital in Northern Virginia, relying in part on a telephone access system to transmit data from bedside monitors. As the remote hospital had no EMR, chart-based patient data such as clinical notes and bedside flow sheets needed to be scanned and transmitted digitally.
The system evolved, and ultimately led to the creation of the company VISICU in 1998 (Rosenfeld et al. 2000). The first modern Tele-ICU system was installed by VISICU in 2000 at Sentara Healthcare in Norfolk, Virginia. Tele-ICU practices expanded notably in 2005-2010, with expansion facilitated by improvements in network speed and bandwidth. During this early phase of Tele-ICU development, systems from VISICU and iMD Soft dominated the commercial market. These early systems used traditional models of administrative and technical structure, whereby, for example, networking programmes would utilise a single central hub to provide Tele-ICU for a remote location or a point-to-point programme within the same healthcare system. Technologically-current Tele-ICU systems use real-time/synchronous audiovisual links between remote clinicians and patients.
Presently, there are no practical barriers in terms of network speed or quality to establishing a Tele-ICU. Nonetheless, adoption of Tele-ICU in the years prior to the COVID-19 pandemic was relatively slow. Barriers to widespread adoption were as follows:
1) Cost
Start-up costs for a Tele-ICU command centre may be up to $5 million, when considering expenses related to construction, installation, and training. Thereafter, yearly operating expenditures may be up to $2 million.
2) Regulatory Requirements
A Tele-ICU system must be HIPAA compliant. Popular consumer-level video conferencing tools do not generally meet the requirements. While nearly every EMR vendor now offers a secure audio/video communication package, these simple, widely-available tools do not meet Tele-ICU regulatory requirements for active patient-monitoring (APM) systems. The US Food and Drug Administration(FDA) has guidance regarding differentiating APM from medical device data systems (MDDS). Devices (including software devices) used for APM must be FDA class II certified (Code of Federal Regulations 21; Medical Devices Data System FDA). Currently, FDA class II certified APM for Tele-ICU include only Philips VISICU, InTouch Health Remote, and iMD Soft Meta Vision ICU (Herasevich and Subramanian 2019).
3) Medical Licensing
Licensing is cited as one of the most significant barriers to telemedicine in the U.S. Currently, each U.S. state grants its medical licenses independently, and – outside of the context of temporary, emergency changes made during the COVID-19 pandemic – each state mandates that an individual who provides medical treatment to a patient located in their state holds a medical license issued from their state. Therefore, establishing multi-state Tele-ICU services requires that every provider in the practice secures medical licenses in all of the states included in their Tele-ICU practice. While an interstate medical licensure compact exists to help expedite multi-state licensure for qualified physicians (https://www.imlcc.org), the licensure process is generally considered to be cumbersome.
Rapid Deployment
Telemedicine transformed healthcare delivery in response to two distinct features of the US COVID-19 pandemic: (1) the demand for stay-at-home outpatient care, and (2) the surge of inpatient hospital admission (Wosik et al. 2020). Beginning in March 2020, there emerged an urgent need for telehealth solutions to manage the problem of large cohorts of outpatients who were unable to travel for routine appointments, in order to evaluate new symptoms and to manage long-term care needs.
At Mayo Clinic, more than 6500 providers performed outpatient video telemedicine consults from the onset of the pandemic through July 15, 2020, a 2000% increase from the 300 providers who had performed telemedicine consults pre-pandemic (Demaerschalk et al. 2021). This rapid increase serves as proof that the existing telemedicine systems are scalable, and that there are no major technological barriers to expansion. Separately, in response to regional surges in inpatient hospital admissions of critically-ill patients with COVID-19, the Mayo Clinic Enhanced ICU (which provides tele-ICU care) was able to establish new telemedicine ICU consultative services in hospitals in New York, Wisconsin, and Florida within days, facilitated in part due to licensing waivers.
Going Forward
Looking ahead to a post-pandemic future, it seems safe to predict that virtual care will remain a part of the US healthcare landscape. The experience during the COVID-19 pandemic has established telemedicine as a reliable and useful mode of healthcare delivery. It is now clear that telemedicine solutions can serve to increase access to care, both for inpatients and for outpatients. It is also clear, based on the experience with COVID-19 itself, that remote patient monitoring can facilitate safe treatment at home for conditions that previously required hospitalisation.
Given these benefits, it is likely that state and federal regulations and policies pertinent to telemedicine will undergo changes, with the intention of reducing barriers to establishing telemedicine practices. Already, bipartisan legislation has been introduced to the US Congress (“The Protecting Access to Post-COVID-19 Telehealth Act of 2021”) which proposes to eliminate most geographic and originating site restrictions on the use of telehealth in Medicare, extend Centers for Medicare and Medicaid Service reimbursements for telemedicine beyond the COVID-19 public health emergency, and make permanent the disaster waiver authority to expand telehealth in Medicare during future emergencies and disasters.
At this point it is evident that telemedicine in general, and Tele-ICU in particular, have great opportunities to incorporate a new generation of tools that will allow for marked improvements in remote care. What will be the functional utility of such state of the art systems and how will they exhibit the true value of telemedicine? First, they will integrate real-time clinical analytics for the purpose of clinical surveillance. Embedding smart algorithms that utilise machine learning into telemedicine systems will allow for predictive and prescriptive analytics among large populations of patients. Such analytics have the potential to foster more accurate and timely care in the management of patients, and to enhance safety when monitoring large numbers of patients. Second, the Tele-ICU Command Centre will transform from a site of co-located physicians and nurses to a multifunctional cockpit operation involving various functions, services and teams in one physical location (Figure 1). Third, real-time ambient intelligence will be at the centre of digital technologies. Fourth, future systems will integrate hospitals around best care protocols.
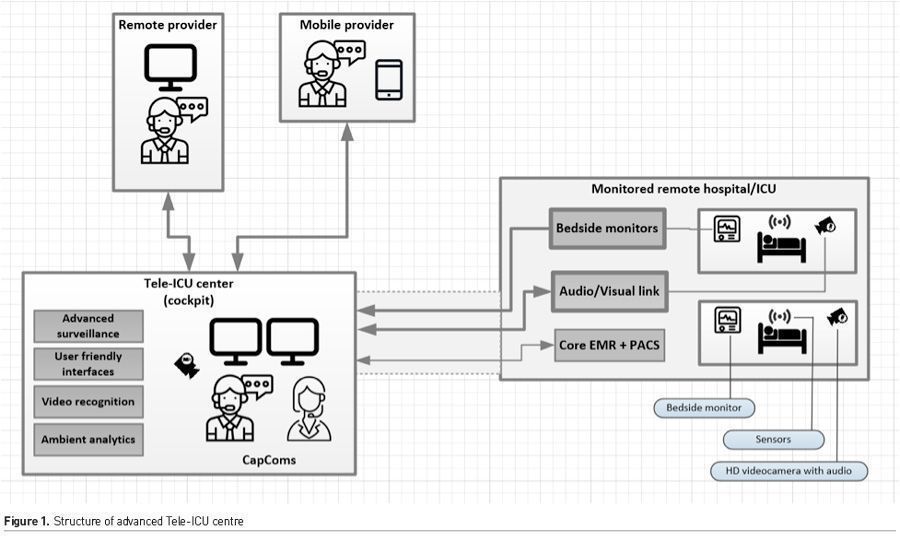
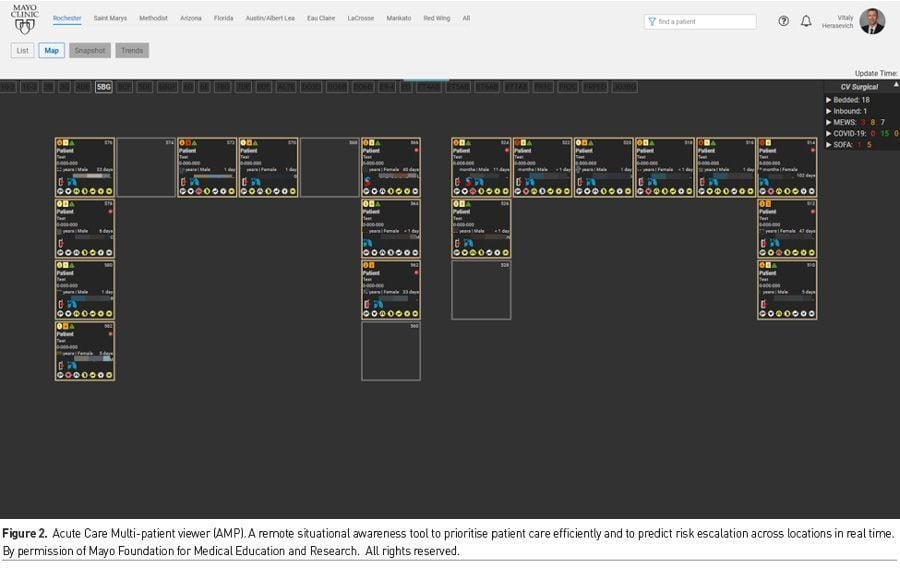
An example of technology designed for the next generation of Tele-ICU is Acute care MultiPatient viewer (AMP). This is an advanced Clinical Control Tower system, which includes central alert screening capabilities. AMP can use machine learning models to generate alerts, which are managed by a designated capsule communicator or “CapCom,” analogous to NASA’s ground-based astronaut who maintains contact with crew members in their spacecraft. AMP also has advanced visualisation for situational awareness and standard communication channels (Figure 2). Video recognition, sound processing and sensor analytics embedded in the workflow will further enhance the system (Davoudi et al. 2019).
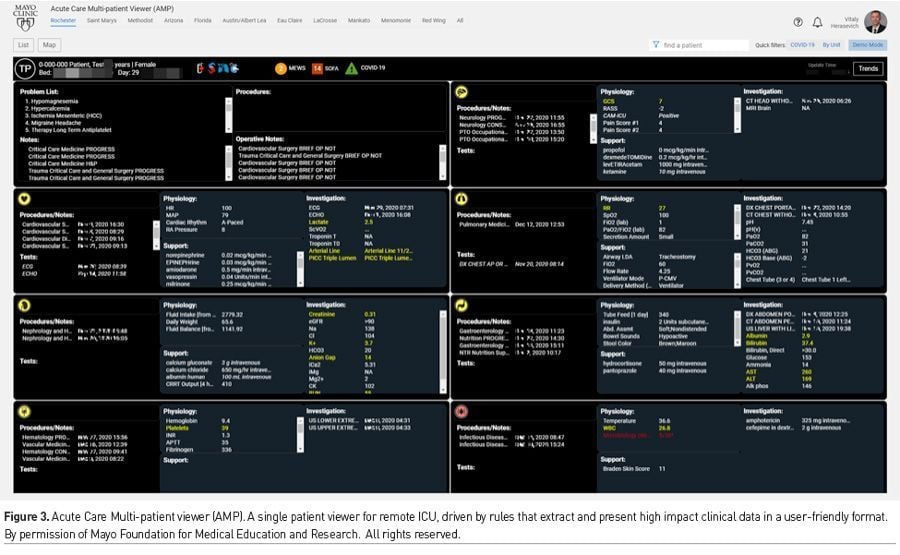
Remote clinicians dealing with large numbers of patients at once require smart tools that enable clinical decision-making without scrolling through the full EMR. High impact data should be extracted by rules and presented in user-friendly formats to minimise cognitive load and errors (Figure 3) (Ahmed et al. 2011). Actionable, predictive, real-time clinical analytics enable proactive and efficient patient care.
After all, telemedicine provides opportunities to harness technology to develop better ways to provide care, rather than simply new ways to do the job. Tele-ICU care will mature from a tool to support regional staffing shortages to a viable clinical service that could apply to a wide range of clinical needs.
Conflict of Interest
None.
References:
Code of Federal Regulations 21 Part 880. Docket No. FDA-2008-N-0106.2008. Available from: accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?CFRPart5880.
Davoudi A et al. (2019) Intelligent ICU for Autonomous Patient Monitoring Using Pervasive Sensing and Deep Learning. Scientific reports, 9(1):8020-8020.
Demaerschalk BM, Blegen RN, Ommen SR (2021) Scalability of Telemedicine Services in a Large Integrated Multispecialty Health Care System During COVID-19. Telemed J E Health, 27(1):96-98.
Doarn CR et al. (2018) Development and Validation of Telemedicine for Disaster Response: The North Atlantic Treaty Organization Multinational System. Telemed J E Health, 24(9):657-668.
Grundy BL et al. (1977) Telemedicine in critical care: an experiment in health care delivery. Jacep, 6(10):439-44.
Herasevich V, Subramanian S (2019) Tele-ICU Technologies. Crit Care Clin, 35(3):427-438.
Medical Devices; Medical Device Data Systems. FDA rule 76 FR 8637 , FDA- 2008-N-0106. Available from federalregister.gov/documents/2011/02/15/2011-3321/medical-devices-medical-device-data-systems.
Nicogossian AE, Doarn CR (2011) Armenia 1988 earthquake and telemedicine: lessons learned and forgotten. Telemed J E Health, 17(9):741-5.
Rosenfeld BA et al. (2000) Intensive care unit telemedicine: alternate paradigm for providing continuous intensivist care. Crit Care Med, 28(12):3925-31.
Scott BK et al. (2020) Advanced Digital Health Technologies for COVID-19 and Future Emergencies. Telemed J E Health, 26(10):1226-1233.
Temesgen ZM et al. (2020) Health Care After the COVID-19 Pandemic and the Influence of Telemedicine. Mayo Clinic proceedings, 95(9S):S66-S68.
Wosik J et al. (2020) Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc, 27(6):957-962.









