ICU Management & Practice, Volume 18 - Issue 4, 2018
Why use sedation?
How much and what sedation?
Less is better in sedation. Side effects of sedation include prolonged mechanical ventilation, increased risk of infection, longer hospital and ICU length of stay and risk of mortality.
The ideal ICU sedation drug has a good ability to provide analgesia, is rapid onset and easy to titrate. Drugs for sedation should allow the possibility to communicate haemodynamic instability and not be associated with delirium.
The concept of titrating the drug to its effect is good. Intensivists should define the target of sedation so that the more drug used the closer to the target is achieved. Sedation is very time-sensitive. Sedating the patient with shock and high agitation so that they can be intubated is essential and they need a high dose for some hours.
The 2018 guidelines for management of pain, agitation/sedation, delirium and immobility and sleep disruption recommend propofol or dexmedetomidine over benzodiazepines for sedation in critically ill, mechanically ventilated adults who are not undergoing cardiac surgery [conditional recommendation, low quality of evidence] (Devlin et al. 2018). A 2013 meta-analysis of benzodiazepine vs non-benzodiazepine-based sedation for mechanically ventilated critically ill patients found that benzodiazepine-based regimens were associated with more ICU days and longer duration of mechanical ventilation, and probably more delirium (Fraser et al. 2013). Lonardo et al. (2014) compared midazolam and lorazepam in adult ICU patients in a retrospective, multicentre study for single ICU admissions with a single ventilation event (>48h) who were treated with continuously infused sedation. There were 2,250 propofol-midazolam and 1,054 propofol-lorazepam matched patients. Patients treated with propofol had a reduced risk of mortality, increased likelihood of earlier ICU discharge and earlier discontinuation of mechanical ventilation.
How to use sedation?
Daily sedation stops
Paired sedation and weaning protocols
Tailor the drug to the patient status
The Sedation Practice in Intensive Care Evaluation (SPICE) study compared deeply sedated with lightly sedated (RASS score [-2 to +1]) patients. Patients who had light sedation within the first 4 hours had reduced time to extubation and improved probability of survival (Shehabi et al. 2012). Other studies demonstrated the same results with shorter time to extubation and better survival in patients with light sedation during the first hours (Shehabi et al. 2013; 2018); the probability of 180-day survival increased with how efficiently sedation was decreased (Shehabi et al. 2018). Importantly, the results did not depend on the drug used but did depend on how they used the drugs.
Two randomised controlled trials that compared dexmedetomidine to midazolam (MIDEX) or propofol (PRODEX) for sedation in more than 1,000 patients during prolonged mechanical ventilation mandated SBT and RASS-targeted sedation (Jakob et al. 2012). The results showed very little change in duration of mechanical ventilation when comparing dexmedetomidine with midazolam; between dexmedetomidine and propofol there was no difference. Patients were more able to communicate and had similar duration of mechanical ventilation and outcomes when dexmedetomidine was used, compared to midazolam or propofol, in patients who did not require deep sedation (Jakob et al. 2012).
Delirium assessment
Does the choice of drug make no difference in all clinical contexts?
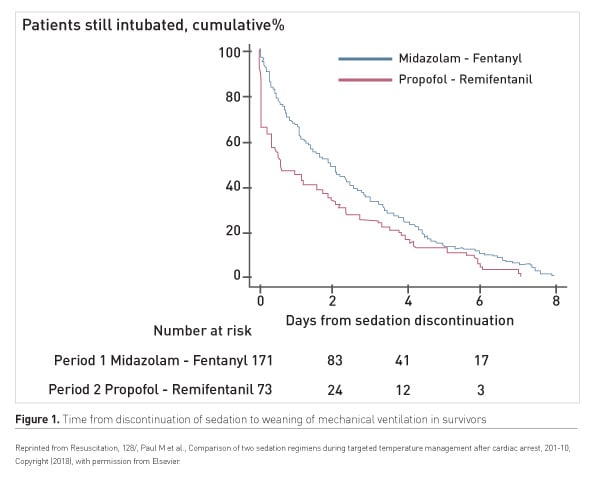
In a study of sedation in patients admitted after out-of-hospital cardiac arrest two periods were compared: propofol-remifentanil, period P2, vs midazolam-fentanyl, period P1 (Paul et al. 2018). Time to awakening and the proportion of comatose patients decreased with the propofol-remifentanil regimen. The propofol-remifentanil regimen was also associated with reduction in mechanical ventilation duration and reduction in incidence of delayed awakening (Figure 1).
How long to sedate?
Conclusion
Key Points
- Prescribe sedation in response to pain, anxiety, agitation, sleeplessness
- Non-benzodiazepine-based sedation vs benzodiazepine is associated with less mortality, less ICU days and earlier discontinuation of mechanical ventilation
- Track compliance with protocols for stopping sedation
- The less sedation the better the likelihood of survival and the shorter the time to extubation
References:
Devlin JW, Skrobik Y, Gélinas C et al. (2018) Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Crit Care Med, 46(9):e825-73.
Fraser GL, Devlin JW, Worby CP et al. (2013) Benzodiazepine versus nonbenzodiazepine-based sedation for mechanically ventilated, critically ill adults: a systematic review and meta-analysis of randomized trials. Crit Care Med, 41(9 Suppl 1):S30-8.
Girard TD, Kress JP, Fuchs BD et al. (2008) Efficacy and safety of a paired sedation and ventilator weaning protocol for mechanically ventilated patients in intensive care (Awakening and Breathing Controlled trial): a randomised controlled trial. Lancet, 371(9607):126-34.
Jakob SM, Ruokonen E, Grounds RM et al.; Dexmedetomidine for Long-Term Sedation Investigators (2012) Dexmedetomidine vs midazolam or propofol for sedation during prolonged mechanical ventilation: two randomized controlled trials. JAMA, 307(11):1151-60.
Kawazoe Y, Miyamoto K, Morimoto T et al.; Dexmedetomidine for Sepsis in Intensive Care Unit Randomized Evaluation (DESIRE) Trial Investigators (2017) Effect of dexmedetomidine on mortality and ventilator-free days in patients requiring mechanical ventilation with sepsis: a randomized clinical trial. JAMA, 317(13):1321-8.
Kress JP, Pohlman AS, O'Connor MF et al. (2000) Daily interruption of sedative infusions in critically ill patients undergoing mechanical ventilation. N Engl J Med, 342(20): 1471-7.
Lonardo NW, Mone MC, Nirula R et al. (2014) Propofol is associated with favorable outcomes compared with benzodiazepines in ventilated intensive care unit patients. Am J Respir Crit Care Med, 189(11):1383-94.
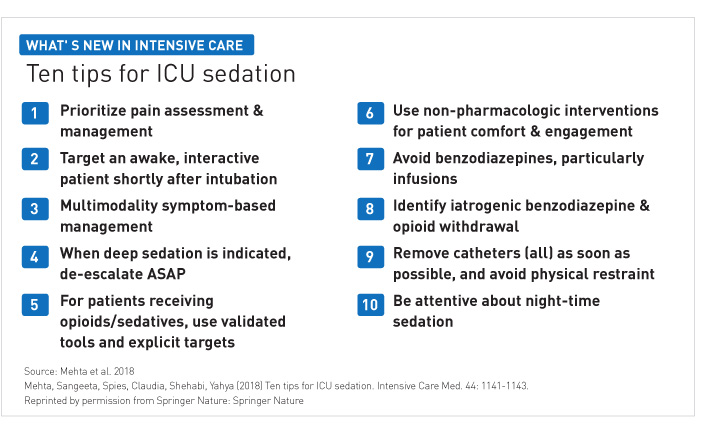
Mehta S, Spies C, Shehabi Y (2018) Ten tips for ICU sedation. Intensive Care Med, 44(7):1141-3.
Patel SB, Poston JT, Pohlman A et al. (2014) Rapidly reversible, sedation-related delirium versus persistent delirium in the intensive care unit. Am J Respir Crit Care Med, 189(6):658-65.
Paul M, Bougouin W, Dumas F et al. (2018) Comparison of two sedation regimens during targeted temperature management after cardiac arrest. Resuscitation, 128:204-210. Erratum in: Resuscitation, 2018 Oct;131:135.
Shehabi Y, Bellomo R, Kadiman S et al.; Sedation Practice in Intensive Care Evaluation (SPICE) Study Investigators and the Australian and New Zealand Intensive Care Society Clinical Trials Group (2018) Sedation intensity in the first 48 hours of mechanical ventilation and 180-day mortality: a multinational prospective longitudinal cohort study. Crit Care Med, 46(6):850-9.
Shehabi Y, Bellomo R, Reade MC et al.; Sedation Practice in Intensive Care Evaluation (SPICE) Study Investigators; ANZICS Clinical Trials Group (2012) Early intensive care sedation predicts long-term mortality in ventilated critically ill patients. Am J Respir Crit Care Med, 186(8):724-31.
Shehabi Y, Chan L, Kadiman S et al.; Sedation Practice in Intensive Care Evaluation (SPICE) Study Group investigators (2013) Sedation depth and long-term mortality in mechanically ventilated critically ill adults: a prospective longitudinal multicentre cohort study. Intensive Care Med, 39(5):910-8.







