ICU Management & Practice, Volume 24 - Issue 1, 2024
Critical care pharmacists use their specialist knowledge to optimise medication for their patients. This article looks at the various roles of the critical care pharmacist within the multidisciplinary team.
Introduction
The pharmacist's role in critical care is well-developed in the United Kingdom (UK), USA, Australia, New Zealand, Canada and some parts of Europe. In this article, we describe the multiple roles of the critical care pharmacist (CCP), how they collaborate with various members of the critical care team and the role of their supporting pharmacy colleagues.
The CCP plays a key role in optimising pharmacotherapy and clinical outcomes in the intensive care unit (ICU), applying their expert knowledge of drug therapy to the individual patient’s needs, and working in conjunction with the multidisciplinary team. CCPs have developed knowledge, skills and experience to become specialists in this field. To enable them along this journey, many pharmacists and pharmacy technicians (PT) attend courses such as our own The Fundamentals of Critical Care Clinical Pharmacy Course(Shulman et al. 2024)and achieve curriculum objectives such as those published by the Faculty of the Royal Pharmaceutical Society (new version pending April 2024). A pharmacist's expertise in medicines and pharmacology makes a significant contribution to the goal of safe and effective care of the most vulnerable and unwell patients in the hospital.
CCPs undertake a daily clinical review of each patient’s drug therapy, taking into account their acute condition and chronic disorders. Working in conjunction with their PT colleagues, they document a record of the patient’s medication history and consider which of these medications are suitable for continued use in the ICU, a process known as medicine reconciliation. Their clinical review will consider laboratory results, clinical observation charts, response and symptoms, and synthesise this information in the context of the appropriateness of the prescribed medications. This review is called medicines optimisation.
Working with the Multidisciplinary Team
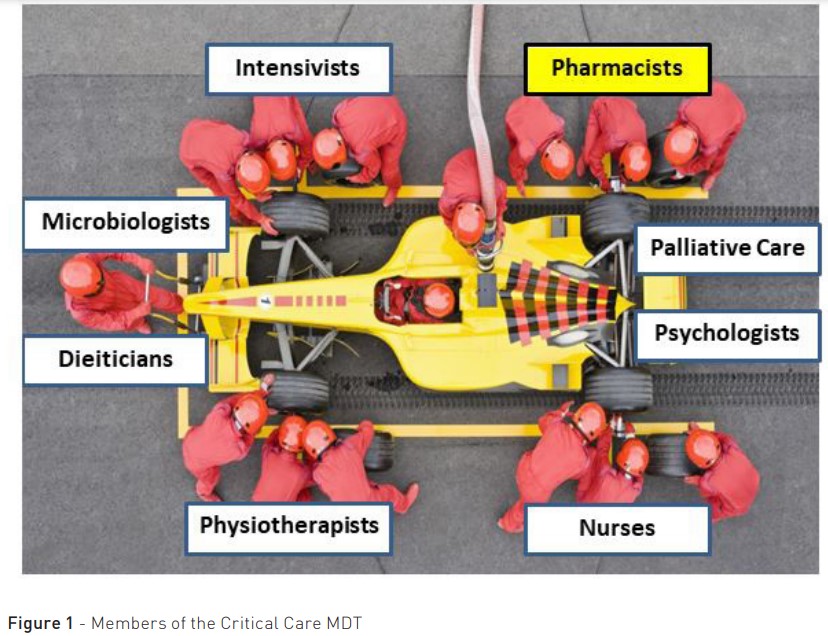
CCPs work closely with a range of healthcare professionals in the multidisciplinary team (MDT), bringing their unique focus for the benefit of the patient, analogous to a Formula 1 team (as depicted in Figure 1). CCPs contribution working within the MDT has been associated with improved patient mortality (Kim et al. 2010), reduced ICU length of stay (Lee et al. 2019) and a reduced number of preventable and non-preventable adverse drug events (Leape et al. 1999).
Working alongside intensivists, pharmacists use their expert knowledge of drug handling to personalise complex drug therapies for individual patients to optimise the use of medications. For example, they can advise on appropriate doses of drugs or alternative drug options for patients in extremes of body weight, age or organ function (e.g. renal replacement therapy), and they can also interpret therapeutic drug monitoring to ensure there is minimal toxicity and maximal therapeutic benefit.
Critically ill patients are more likely to experience adverse drug effects or interactions due to the large number of medications they are prescribed. Therefore, the pharmacist has an important role in identifying potential adverse effects or highlighting significant drug-drug or drug-condition interactions which may result in adverse outcomes. Encouraging the deprescribing of any unnecessary medications can also help to reduce adverse effects.
Pharmacists work closely with nursing colleagues on critical care and provide support in various ways, including checking the compatibility of multiple intravenous infusions or advising on unusual routes of administration of medications. Discussions explore and can resolve issues around medication tolerability, pain, bowel movements, administration of intravenous medications, sourcing medication, and safe and secure storage of medication.
Dieticians collaborate with pharmacists to formulate feeding plans and decide on the timing of drug administration based on the interactions between enteral feeds and drugs (e.g., levothyroxine should be administered two hours after a feed is stopped). They may also produce parenteral nutrition plans based on the patient’s requirements. Pharmacists organise the manufacturing or procurement of these bags.
Pharmacists collaborate with physiotherapists to advise on appropriate pharmacological therapy for secretion management. They will also aim to titrate the sedative effects and maximise analgesia to allow for effective rehabilitation.
CCPs and clinical psychologists can work closely to explore both non-pharmacological and pharmacological options for the management of delirium, agitation, anxiety and sleep. They may also work with mental health teams to manage patients with a complex psychiatric history.
Pharmacists participate in the MDT ward round, which brings together contributions to patient care from the various participants to provide shared decision-making, tailoring therapy to the individual patient’s needs. Ward rounds are mostly undertaken at the bedside, but the advent of virtual meeting platforms has provided the potential for wider MDT input. In the PROTECTED-UK study (Shulman et al. 2015), more than half (59.4%) of pharmacist-led contributions were made during the ward round, demonstrating the importance of pharmacists being present. This study highlighted that many pharmacists' contributions do not arise from a request for input from the MDT but are initiated from the pharmacist’s proactive patient review. The study also found that 88% of these pharmacists' contributions were agreed upon and implemented by the MDT.
Additional activities carried out by the specialist CCP include involvement in audit, research, guidelines development, staff education and financial reporting. Larger ICUs will have an ICU pharmacy team consisting of a consultant-level lead pharmacist, senior specialist CCPs and rotational clinical pharmacists, pharmacy technicians and potentially, pharmacy assistant(s) (FICM 2024). In the UK, The Intensive Care Society and the Faculty of Intensive Care Medicine produced the Guidelines for the Provision of Intensive Care Services (GPICS). GPICS states there must be a designated intensive care pharmacist for every critical care unit. There must be one specialist pharmacist for every 10 ICU beds, one for every 20 high-dependency beds for a weekday service, and proportionately more for a 7-day service, which is the target (GPICS 2022). In practice, a larger team is required to cover leave and sickness.
PTs work cohesively with the pharmacist to provide a supporting role. They document the drug history of each patient, forming the first step of the medicine's reconciliation process. This can be complicated given the patient's history, the barriers to communication with the sedated or intubated patient and the need to consult a variety of sources of information. The PTs are also responsible for organising the regular supply of medications in the ICU, responding to urgent requests for critical medications, responding operationally to drug shortages, conducting medication use audits, and liaising closely with the charge nurse. In some hospitals, the role of the PT has extended into areas such as compiling drug expenditure finance reports and staff training.
A pharmacy assistant is an emergent role whose tasks could include fridge temperature documentation, medication expiry checks, medication returns, medicine delivery to the bedside, unpacking medicines deliveries, and organising medication storage in the unit. These roles provide an effective skill mix, freeing up nursing and pharmacist time to focus on their clinical priorities.
Medication Safety and Clinical Governance
ICU patients are prescribed nearly twice as many medications as those in other non-ICU settings. This increases the risk of adverse events, medication errors and drug interactions. (Cullen et al. 1997).Adverse drug events are found to be significantly reduced when ICUs have a pharmacist integrated as part of the MDT (Lee et al. 2019).The pharmacist helps to reduce medication errors and patient harm through clinical chart reviews and medicines reconciliation on an individual patient basis but, in addition, can assist in creating a safer environment via a range of clinical governance measures. An example of this is contributing to regular incident meetings where reported events are investigated by the pharmacist, intensivist and nurse, looking at root cause analyses and ways to prevent reoccurrence. A broader MDT review of medication incidents leads to an enhanced understanding of the contributory factors, leading to more effective solutions. Pharmacists can action system learning and feedback to staff through a variety of means, which also provides a safer environment for patients through continuous improvement (Shulman 2022). CCPs encourage collaboration between the pharmacy department and critical care units, for example, to procure ready-to-administer vials or pre-filled syringes of medications to enhance safety and reduce nursing preparation times.
Wider roles include setting up and maintaining electronic prescribing systems, writing the drug library for medication smart pumps, medication barcoding, and automated dispensing cabinets, which may help improve medicines management and governance around controlled drugs.
Reducing Medication Expenditure
Studies have shown a positive cost-benefit from CCP’s contributions. Bosma et al. (2019) estimated a cost–benefit of €119–136 per accepted pharmacist contribution, and one review reported a median cost–benefit of £6.42 per £1 invested in pharmacy services (Crosby et al. 2020). Alongside clinical interventions, other cost-saving activities which pharmacists can undertake include:
- Reviewing drug expenditure reports
- Advising on cheaper but effective switches between drugs within the same class
- Encouraging intravenous to oral switches where clinically appropriate
- Preventing the wastage of medications and managing the stock of medications
- Promoting the deprescribing of medications where not clinically indicated (e.g. anti-infectives, stress ulcer prophylaxis)
Not only do these activities help reduce costs, but they also help the MDT take a more sustainable approach to healthcare. Medications are a large contributor to climate and ecological emergencies, and many of the pharmacy team's actions are consistent with reducing the carbon footprint and environmental risk. This focus will increasingly become more pronounced.
Independent Prescribing Pharmacists
Traditionally, doctors prescribe medication, but at least in the UK, this role has been extended more widely and in critical care, it is standard for the CCP to be an accredited independent prescriber within their area of clinical competence. Up to 72% of critical care units in the UK have a practicing independent prescribing pharmacist on the team (Borthwick et al. 2023). Independent prescribers can prescribe (or deprescribe) medications as part of their clinical review, helping reduce the workload of the MDT and improve efficiency. Prescribing examples include dose adjustments, formulation changes, new medications to initiate as discussed in the ward round, correction of incorrectly prescribed medications, parenteral nutrition, and patients' home medications. Such prescribing decisions can be made immediately without having to contact a medical prescriber, and hence, treatment can be updated without delay.
Antimicrobial Stewardship
Antimicrobial usage in ICUs is high; approximately 70% of critically ill patients receive anti-infectives during their admission (Vincent et al. 2009). Pharmacists play an important role in carrying out antimicrobial stewardship activities. Working closely with physicians, pharmacists can provide advice on appropriate antibiotic choices based on resistance patterns within their area and optimal personalised dosing in relation to organ function and patient characteristics. They can also prompt the medical teams to undertake regular reviews of antimicrobial therapy to prevent unnecessarily prolonged therapy and inadvertently discontinued anti-infectives, which may drive up resistance.
Discharge roles
Patient discharge from the ICU to a non-ICU ward is one of the most challenging and high-risk transitions of care due to the number of medications and the complexity and acuity of the medical conditions that characterise this patient group. (Heselmans et al. 2015).
Bourne et al.'s (2022) systematic review highlighted that frequent medication changes, with many chronic medicines discontinued and acute medication commenced, present a patient safety concern, particularly at the point of transition.
CCPs can advise on the step-down medication plan of patients at the point of transition. This includes highlighting medications that require a medical review, critical care medications that require deprescribing (e.g., antipsychotics for delirium, strong potassium infusions), and continuation of pre-admission medications for chronic conditions. This avoids post-ICU polypharmacy, potential harm and unintentional continuation of medications.
Pharmacists are often best placed to facilitate the safe discharge of complex ICU patients from the ICU to home, as other members of the MDT may not be familiar with the issues around discharge.
Research and Evaluation
Pharmacists have a role in investigating, leading, conducting, and supporting research and evaluation. They frequently collaborate with intensivist teams (for example, Chan et al. 2022) or join pharmacy research teams (for example, Shulman et al. 2015) to investigate gaps in knowledge.
CCPs contribute to writing local and national guidelines and protocols to promote a standardised, equitable approach to pharmacotherapy, considering individual patient characteristics. Both are produced by critically appraising the published data and promoting an evidence-based approach to patient care.
Pharmacists produce medicine management policies, which set out the best practices for safe prescribing, dispensing, pharmacist clinical review, storage and administration of medicines.
Audits and quality improvement projects are developed and implemented by pharmacists, often in collaboration with the nursing, medical or the wider team. This can include conducting monthly audits to monitor the safe and secure storage of medications with the nurses. Regular auditing can measure and improve adherence to standards and lead to continuous improvement and changes in practice.
Education and Training
Pharmacists can provide education and training for nurses and doctors. This could include a ‘journal club’ literature review as a prelude to practice change, providing prescribing tips for commonly used drugs within critical care, sharing learning outcomes from medication incidents, guidance on the clinical governance process for managing controlled drugs and clinical advice around dosing in organ failure. A team's awareness of this information will improve medication safety, promote safe prescribing and reduce medication errors from occurring.
Pharmacists also relay information to the MDT about new relevant national guidelines, drug safety alerts, medication shortages and strategies on how these will be managed.
The COVID-19 pandemic highlighted a demand for more critical care trained pharmacists to support the increased number of ICU admissions. To address this training burden, we established an international training course, ‘The Fundamentals of Critical Care Clinical Pharmacy Course’(Shulman and Gadher 2024).
Conclusion
CCPs use their specialist knowledge to perform daily clinical reviews to optimise medication for their patients. Working in close collaboration with the critical care teams, they have become integral members of the MDT, contributing to positive clinical outcomes and safety for patients in the ICU. Their roles also include education and training, research, service improvement, managing drug expenditure and promoting medication safety.
Conflict of Interest
None.
References:
Borthwick M et al. (2023) Critical care pharmacy workforce: a 2020 re-evaluation of the UK deployment and characteristics. Human Resources for Health. 21:28.
Bosma LBE et al. (2018) The effect of a medication reconciliation program in two intensive care units in the Netherlands: a prospective intervention study with a before and after design. Ann. Intensive Care. 8:19.
Bourne RS et al. (2022) Medication-related interventions to improve medication safety and patient outcomes on transition from adult intensive care settings: a systematic review and meta-analysis. BMJ Qual Saf. (8):609-22.
Chan XHS et al. (2022) Comparison of Antibiotic Use between the First Two Waves of COVID-19 in an Intensive Care Unit at a London Tertiary Centre: reducing broad-spectrum antimicrobial use did not adversely affect mortality, Journal Hosp Infection. 124:37-46.
Crosby A et al. (2023) Economic evaluations of adult critical care pharmacy services: a scoping review. Int J Pharm Pract. 31(6):574-84.
Cullen DJ et al. (1997) Preventable adverse drug events in hospitalized patients: a comparative study of intensive care and general care units. Crit Care Med. 25 (8):1289–97.
FICM (2024) Critical Care Workforce Development Toolkit V1.0 - January 2024. Available at Critical_Care_Career_Pathway_Toolkit.pdf (ficm.ac.uk)
Heselmans A et al. (2015) Medication review by a clinical pharmacist at the transfer point from ICU to ward: a randomized controlled trial. J Clin Pharm Ther. 40:578-83.
ICS and FICM (2022) Guidelines for the Provision of Intensive Care Services - Edition 2.1. Available at Intensive Care Society | GPICS V2.1
Kim MM et al. (2010) The effect of multidisciplinary care teams on intensive care unit mortality Arch Intern Med. 170(4):369-76.
Leape LL et al. (1999) Pharmacist Participation on Physician Rounds and Adverse Drug Events in the Intensive Care Unit. JAMA. 282(3):267–70.
Lee H et al. (2019) Impact on Patient Outcomes of Pharmacist Participation in Multidisciplinary Critical Care Teams: A Systematic Review and Meta-Analysis. Critical Care Medicine. 47(9):1243-50.
Shulman R et al. (2015) Pharmacist's review and outcomes: Treatment-enhancing contributions tallied, evaluated, and documented (PROTECTED-UK). J Crit Care. 30(4): 808-13.
Shulman R, Gadher N (2024) The Fundamentals of Critical Care Clinical Pharmacy Course 2024. Available at https://sites.google.com/view/fundamentalsofcriticalcare24/home
Shulman R (2022) Processes to reduce medication errors in the ICU. ICU Management & Practice. 22(1):30-3.
Vincent JL et al. (2009) International study of the prevalence and outcomes of infection in intensive care units. JAMA. 302(21):2323-9.









