Malnutrition is frequently observed in upper gastrointestinal cancer surgical patients; it is an independent predictor of postoperative morbidity and mortality and leads to both increased length of hospital stay and hospital costs. Consequently, every effort should be made to apply nutritional support, including both standard enteral nutrition (EN) and immunonutrition, as a complementary therapeutic limb in current oncological treatment protocols.
Epidemiology and Consequences of Malnutrition
Gastric and oesophageal cancers are among the leading causes of cancer-related death worldwide due to late presentation and poor prognosis. In curable disease, a therapeutic strategy encompassing surgery, chemotherapy and/or chemoradiation is thus mandatory (Mariette et al. 2012). Malnutrition is frequently observed in 60–85% of surgical patients with an upper gastrointestinal cancer (Stratton et al. 2003) and is an independent predictor of postoperative morbidity and mortality, leading to increased length of hospital stay and hospital costs (Stratton et al. 2006). Many factors can affect nutritional status, particularly disease stage and the choice of treatment used (surgery, chemotherapy and/or radiotherapy) (Van Cutsem 2005). Nutritional support should therefore be used as a strong therapeutic weapon, which may be complementary to standard active oncological therapy.
Nutritional Interventions in Digestive Cancer Surgery
Nutritional support in oncology patients aims to prevent early death, decrease postoperative complications and improve quality of life. It should begin early and be a routine part of the treatment of cancer patients. Depending on patients’ individual needs, these goals may be achieved by giving patients nutritional recommendations and dietary advice, as well as by providing artificial nutrition using oral supplements, EN via a feeding tube, or parenteral nutrition (PN).
Dietary advice may be sufficient when the patient is capable of consuming at least 75% of his or her nutritional requirements to maintain good health and there is no radiotherapy, chemotherapy or surgery scheduled. However, when these requirements are not met and dietary advice is insufficient, a higher level of nutritional support must be initiated. Oral supplementation should be used in cases of malnutrition or when the patient is unable to consume at least 50–75% of his or her requirements by means of conventional feeding for a period longer than five consecutive days.
In moderate or severe malnutrition, or when patients are unable to consume at least 50% of their requirements through conventional feeding for more than five consecutive days (Lipman 1998; Braunschweig et al. 2001), enteral feeding is required. The implementation of EN is recommended when the patient’s gastrointestinal tract is functional as it appears to have better efficacy, lower cost and cause less iatrogenic complications than PN (Mariette et al. 2005). In cases where swallowing is affected, for example in oesophageal cancer, or if serious mucositis is expected, EN should be administered through a nasogastric or nasoenteric tube for a duration of two to three weeks. Alternatively, gastrostomy (in oesophageal cancer) and jejunostomy (in oesogastric cancer) feeding may be administered for a duration of more than two to three weeks (Mariette et al. 2005, Conference de consensus 1995). Figures 1 and 2 propose an algorithm for deciding upon the route of EN administration in oesophageal and gastric cancers, respectively. In a recent review of our experience with percutaneaous radiological gastrostomy (PRG) before surgery for oesophageal cancer, we found a PRG complication rate of 3.4%, without any incidence of metastatic inoculation and without any injury of the gastric vascular arcade, thus not compromising subsequent gastric pull-up. Due to early enteral feeding, outcomes of malnourished patients were similar to those of non-malnourished patients (Tessier et al. 2012).
As other scientific societies have done, the French Society of Digestive Surgery established guidelines, graded from A to C (a grading system is summarised in Table 1), on perioperative nutritional support in GI cancer surgery (Mariette et al. 2005), including the following suggestions:
• During the perioperative period, EN is not required in well-nourished patients, those with weight loss of <10% or in patients who can sustain an oral diet providing at least 60% of their needs within the week following surgery (Grade A).
• Preoperative nutrition is recommended in severely malnourished patients with weight loss ≥20% who will undergo major surgery (Grade A). The same approach seems to be beneficial for patients with moderate malnutrition (weight loss of 10–19%) (Grade B).
• Postoperative nutrition is recommended:
i. In all patients who benefited from preoperative nutrition (Grade A);
ii. In all malnourished patients who did not benefit from preoperative nutrition (Grade A);
iii. In patients who cannot resume an oral diet in the postoperative course due to surgical complications (Grade A), or in patients consuming <60% of the required diet within the week following surgery (Grade A); and
iv. In other patients for whom no unequivocal recommendation could be drawn (Grade B).
Immunonutrition
Major surgery leads to a decline in immune status, and an increase in postoperative mortality and rates of infectious morbidity. Enhancing immune function could help decrease such complications. In recent years, standard EN has been enhanced with nutrients whose specific purpose is to upregulate the host immune response, control the inflammatory response and improve nitrogen balance and protein synthesis following surgery. The immunonutrients used are glutamine, arginine, poly-unsaturated fatty acids (omega- 3), nucleotides, taurine, vitamins A, E, and C, beta-carotene and trace elements.
The use of immunonutrition in the surgical setting has been well studied with over 28 randomised controlled trials showing that immunonutrition is more efficient than standard isocaloric and isoenergetic nutrition in significantly decreasing postoperative infectious morbidity, length of hospital stay and healthcare costs (Gianotti et al. 2002, Beale et al. 1999).
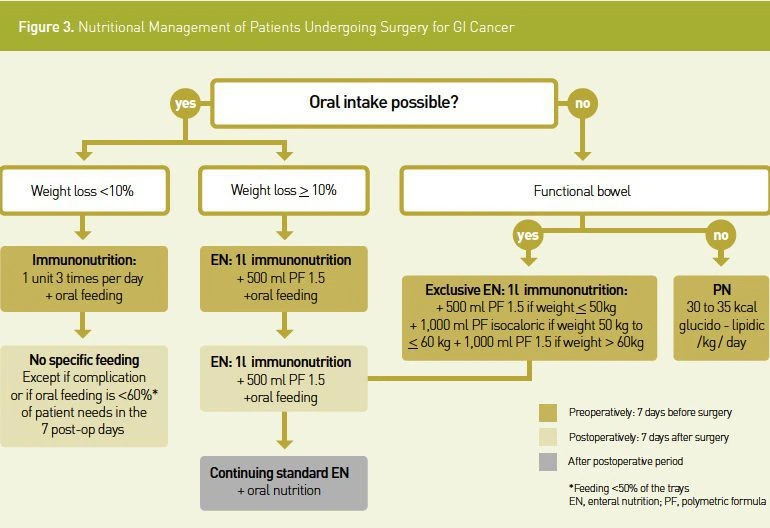
However, there is a great degree of heterogeneity in terms of nutritional status and the type of control used, and in some studies samples were quite small. Despite this, the effect of immunonutrition has generally been found to be beneficial, especially in malnourished patients. Numerous meta-analyses have assessed the evidence relating to the use of immunonutrition in the surgical setting (Cerantola et al. 2011; Marimuthu et al. 2012). The overall conclusion is that in surgical patients, a lower rate of infectious complications and shorter hospital stay were associated with perioperative immunonutrition, relative to standard EN. Figure 3 illustrates a decision tree for the nutritional management of patients undergoing GI cancer surgery.
Enteral immunonutrition lasting five to seven days is recommended in the preoperative setting in all patients who will benefit from oncological GI surgery (Grade A). In the postoperative period, immunonutrition should be continued in all patients who were malnourished in the preoperative period:
• For five to seven days, provided that there are no postoperative complications; or
• Until patients can consume an oral diet meeting at least 60% of their requirements (Grade A).
Putting the Perspective into Practice
It is known that:
(i) Immunonutrition is efficient in the perioperative period in oesophago-gastric cancers;
(ii) Both oesophageal and gastric cancer patients are frequently malnourished; and
(iii) Most patients with oesophago-gastric cancer will receive neoadjuvant chemo(radio)therapy that may compromise both nutritional and immune status.
Hence, routine immunonutrition may help to support immune and nutritional status during the neoadjuvant and perioperative treatment periods. To test this hypothesis, an ongoing European randomised controlled trial sponsorised by NestléHealthScience, with myself Prof. Mariette as Principal Investigator, is assessing the role of long-term administration of immunonutrition during the neoadjuvant and the surgical phases to improve quality of life, to reduce postoperative morbidity and to reduce neoadjuvant treatment toxicities (NCT01423799).
Conclusion
Knowledge of the nutritional status of patients with oesophago-gastric cancer is essential, not only in identifying malnourished and non-malnourished patients, but also in allowing treatment adaptations along each step of the multimodal oncological treatment path. Whether or not the treatment procedure is surgical, all patients could benefit from nutritional support during oncologic treatments. Preoperative immunonutrition lasting five to seven days is proposed for both malnourished and nonmalnourished patients with oesophago-gastric cancer, along with artificial nutrition for at least seven days after surgery for malnourished patients. Dietary counselling should be provided to all patients receiving chemotherapy and/or radiotherapy. Surgeons play a key role in including and applying nutritional support as a strong therapeutic weapon in the oncological therapeutic strategy for GI cancer patients.




References:
Beale RJ et al. (1999). Immunonutrition in the critically ill: a systematic review of clinical outcome. Crit Care Med. 27:2799-805.
Braunschweig CL et al. (2001). Enteral compared with parenteral nutrition: a meta-analysis. Am J Clin Nutr. 74:534-42.
Cerantola Y et al. (2011) Immunonutrition in gastrointestinal surgery. Br J Surg. 98:37-48.
Conference de consensus (1995). Nutrition périopératoire en chirurgie réglée de l’adulte. Nutr Clin Metabol. 9(suppl 1):1-50
Gianotti L et al. (2002). A randomized controlled trial of preoperative oral supplementation with a specialized diet in patients with gastrointestinal cancer. Gastroenterology.122:1763-70.
Lipman TO (1998). Grains or veins: is enteral nutrition really better than parenteral nutrition? A look at the evidence. JPEN J Parenter Enteral Nutr. 22:167-82.
Mariette C et al. (2012). Surgery in Esophageal and Gastric Cancer Patients: What is the Role for Nutrition Support in your Daily Practice? Ann Surg Oncol. 19:2128-34.
Mariette C et al. (2011). Oesophagogastric junction adenocarcinoma: which therapeutic approach?
Lancet Oncol. 12:296-305.
Mariette C et al. (2005). Société Française de Chirurgie Digestive. Perioperative care in digestive surgery. J Chir (Paris). 142:14-28.
Marimuthu K et al. (2012). A meta-analysis of the effect of combinations of immune modulating nutrients on outcome in patients undergoing major open gastrointestinal surgery. Ann Surg. 255:1060-8.
Stratton RJ and Elia M (2006). Deprivation linked to malnutrition risk and mortality in hospital. Br J Nutr. 96:870-6.
Stratton R, et al. (2003). Prevalence of diseaserelated malnutrition. In: Stratton RJ, Green CJ, Elia M, eds. Disease-related malnutrition: An evidence-based approach to treatment. CABI Publishing, Wallingford, Oxon. 35-92.
Tessier W et al. (2012). Percutaneous radiological gastrostomy in oesophageal cancer patients: a feasible and safe access for nutritional support during multimodal therapy. Surg Endosc. Sep 7. [Epub ahead of print]
Van Cutsem E and Arends J (2005). The causes and consequences of cancer-associated malnutrition. Eur J Oncol Nurs. 9 Suppl 2:S51-63.