Several gender differences relate to optimal nutrition in intensive care. We describe these differences and their hypothetical implications for the patient.
Introduction
Nutrition therapy is an integral and important part of therapy in the intensive care unit (ICU). Malnutrition leads to more complications, more infections, longer hospital stays and even death (Lochs 2006, Norman 2008). Maintenance of lean body mass is crucial to improve outcome in critical care; hence, nutrition therapy aims at conservation or restoration of the body protein mass and provision of adequate amounts of energy. In adult intensive care, we generally treat all our patients in a similar fashion, in spite of large differences in age, posture, race or gender. In particular, body composition differs substantially between males and females, as does rate of metabolism. In the concept of optimal nutrition of critically ill patients the primary aim is to target individual needs of energy and protein, incorporating various parameters such as body weight, length and gender (for example, when using energy expenditure formulas). However, what is the basis for a gender-specific nutritional strategy, and what is the potential effect of this approach on outcome?
Optimal Nutrition
The first of several challenges is that of defining optimal nutrition. Adequate nutrition in intensive care is defined as providing energy as measured by indirect calorimetry, with the amount of protein reaching at least 1.2 g/kg pre-admission body weight per day. (Sauerwein and Serlie 2010; Sauerwein and Strack van Schijndel 2007). However evidence supporting these nutritional goals is mainly based on surrogate outcome parameters.
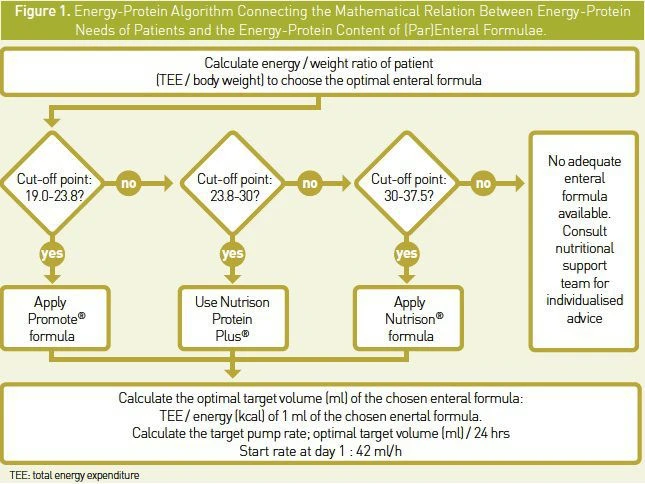
Another well-known challenge is to attain optimal nutrition. We developed a nutrition algorithm to improve nutrition therapy, which is fully incorporated into a patient data management system (Strack van Schijndel 2007). This energy-protein algorithm connects the mathematical relation between energy- protein needs of patients and the energy- protein content of (par)enteral formulae. The algorithm provides an appropriate nutrition formula for each ICU patient and also provides adequate pump speed to reach prespecified protein and energy targets (Figure 1).
A third challenge is to show the benefit that nutrition strategies have on outcome. Most studies failed to demonstrate any impact on outcome (Barr J et al. 2004; Doig GS et al. 2008; Martin CM et al. 2004). We have investigated the effect of our energy-protein targeted approach on clinical outcome in mechanically ventilated critically ill patients in a prospective observational study (Strack van Schijndel et al. 2009; Weijs et al. 2012).
Benefit on Outcome for Females Only?
In a prospective observational cohort study of 243 patients in a mixed medico-surgical ICU, we surprisingly found that optimal nutritional therapy, defined as more than 90% of total energy expenditure as measured by indirect calorimetry and provision of 1.2–1.5 g of protein/kg per day, was associated with reduced ICU, 28-day, and hospital mortality in female patients only. Female patients for whom both energy and protein goals were reached had better outcomes than those for which only energy goals were reached.
For males, no benefit from optimal nutrition could be demonstrated. We could not explain this finding, but we speculated that females have a lower protein mass, largely manifested as muscle mass, and therefore may have had a larger benefit from optimal protein delivery. In a later extended analysis consisting of 886 patients (including the 243 patients mentioned above), we confirmed that optimal nutrition therapy in mechanically ventilated critically ill, defined as both protein and energy targets reached, was associated with a decrease in 28-day mortality by 50%; however, we found this effect in both male and female patients. The gender difference was lost in this larger trial.
Gender Related Differences in Nutrition
There are several gender differences that relate to nutrition and these differences come with several hypothetical implications. The metabolic rate of men is generally higher than in women, due to larger body size and mainly higher active cell mass. This is taken into account in the most commonly used energy expenditure formulae. Body composition differs substantially between males and females.
A possible explanation for the difference in effect of nutritional therapy between men and women might be that the maintenance of protein mass in the body above the critical minimum is vital to survival. In other words, a lean body mass above the critical level is essential for the human body to function in a vital manner. Beyond this hypothesised protein threshold, loss of organ function and failing immune status will contribute to mortality. If this hypothesis is true, males have an advantage in nutritional reserve, because they are heavier and also have a more favourable proportionality between fat and protein, with larger relative protein stores.
Females may have a disadvantage, because they will reach this presumed minimum protein threshold in a shorter period of time during catabolism. On the other hand, it is suggested that fat stores might "protect" protein stores during periods of underfeeding, which might benefit females. Adequate nutrition aims to protect the body composition and is aimed at slowing down net protein catabolism. Due to the smaller reserves that females have, the effect of nutrition will be more obvious. However, with the exception of our first analysis (Strack van Schijndel et al. 2009), no reported studies account a gender-specific effect on outcome from nutritional interventions.
Another important consideration is that the energy deficit occurs mainly in the first days after admission, when targeted volume cannot be administered for practical reasons, such as gastric retention, slow increase of nutrition towards the targeted volume, haemodynamic instability, and diagnostic and therapeutic interventions. Allowed gastric residual volume is similar in males and females whilst the amount of enteral feeding in ml/hour is generally lower for women because of smaller caloric and protein needs. This might contribute to females reaching nutritional goals earlier.
Conclusion
There is still much debate about whether gender plays a role in outcome in critical care. Studies evaluating this relationship in critically ill patients have reached inconsistent results.We believe that gender differences relate to optimal nutrition in intensive care and these differences come with several hypothetical implications. For studies that found a gender-related difference in outcome, it would be interesting to specifically look at whether nutritional targets were reached more often and earlier in women, especially in the first days after admission.

References:
Barr J et al. (2004). Outcomes in critically ill patients before and after the implementation of an evidence- based nutritional management protocol. Chest,125:1446-1457.
Doig GS et al. (2008). Effects of evidence-based feeding guidelines on mortality of critically ill patients: a cluster randomized controlled trial. JAMA, 300:2731-2741.
Lochs H et al. (2006). Evidence supports nutritional support. Clin Nutr, 25:1779.
Martin CM et al. (2004). Multicentre, cluster-randomized clinical trial of algorithms for critical-care enteral and parenteral therapy (ACCEPT). CMAJ,170:197-204.
Norman K et al. (2008). Prognostic impact of disease related malnutrition. Clin Nutr 27:5-15.
Pichard C et al. (2004). Nutritional assessment: lean body mass depletion at hospital admission is associated with an increased length of stay. Am J Clin Nutr, 79:613.
Sauerwein HP and Serlie MJ (2010). Optimal nutrition and its potential effect on survival in critically ill patients. Neth J Med, 68:119-22.
Sauerwein HP and Strack van Schijndel RJM (2007). Perspective: How to evaluate studies on peri-operative nutrition? Considerations about the definition of optimal nutrition for patients and its key role in the comparison of the results of studies on nutritional intervention. Clin Nutr, 26:154-8. Strack van Schijndel et al. (2007). An algorithm for balanced protein/energy provision in critically ill mechanically ventilated patients. E Spen Eur E J Clin Nutr Metab, 2: 69-74.
Strack van Schijndel RJM et al. (2009). Optimal nutrition during the period of mechanical ventilation decreases mortality in critically ill, long-term acute female patients: a prospective observational cohort study. Crit Care, 13:R132.
Weijs PJ et al. (2012). Optimal protein and energy nutrition decreases mortality in mechanically ventilated, critically ill patients: a prospective observational cohort study. JPEN, 36: 60-8.