ICU Management & Practice, Volume 23 - Issue 3, 2023
The critically ill patient should be framed within sustainable medicine. It is crucial to mitigate the causes so that we do not have to adapt to the undesirable effects of the unsustainability of our clinical practice. We propose a simultaneous approach to sustainability in people, products, processes, and our planet.
Introduction and Justification
GREEN ICU (GREater ENvironmental sustainability in Intensive Care Units) is a multidisciplinary initiative that aims to develop evidence-based guidelines to reduce the environmental footprint of intensive care practice. Nowadays, we need a sustainable approach to our critical patient care that reduces the environmental impact of an ICU.
According to the Brundtlandt Report (1987), sustainable development is development that meets the requirements of the present generation without jeopardising the needs of future generations. Being aware of the scarcity of energy, resources and ecological footprint that measures the impact of our health activity is necessary to initiate any sustainability strategy.
Thirty-six years after Brundtlandt's definition, the danger is not only for future generations but also for current generations. Air pollution is the fifth most frequent cause of mortality worldwide: 4.2 million deaths/year (Schraufnagel et al. 2019). The main pollutants are sulphur dioxide, nitrogen oxide and volatile organic compounds.
A variety of strategies are included in sustainable medicine to lessen our effect on the environment: reducing our greenhouse gas emissions, water pollution, ecotoxicity, and social and economic impact. To prevent worse things from happening, just like with our patients, the main thing is to do no harm, including to our planet (Fang 2022).
The reality is that there is a problem of lack of sustainability in our health services, hospitals, and ICUs. Healthcare accounts for 5% of the world's GHGs. If healthcare were a nation, it would be the fifth largest GHG nation (Lenzen 2020).
It has been quantified that 30% of our clinical care is low value which would pollute without any health benefit (Barratt 2022). We, the professionals who care for each of our critical patients, are the guarantors of solving this. Therein lies another problem: our lack of regular updates on what we need to know to be part of the solution.
The impact on the environment is analysed through:
| A. | Medical care. Expenditure, energy use of facilities and type of care. |
| B. | Life cycle analysis (LCA) or cradle-to-grave analysis. Analyses the environmental impact of natural resource extraction, manufacturing, packaging, transport, use/reuse and recycling/disposal of product or process waste (McGain 2018). |
| C. | Material flow analysis (MFA). Quantifies material and waste flows entering and exiting the system defined in a given space (patient admitted to ICU) and time (day), with identification of environmental hot spots in ICU that require urgent efforts with opportunities for sustainable innovation. |
| D. | The carbon footprint, which represents the total volume of greenhouse gases (GHG: CO2, methane, nitrous oxide, others) produced by our activity, measured in CO2 emissions. As an indicator of this footprint, we use CO2 emissions or Carbon Dioxide Equivalent (CO2e). Its calculation helps an organisation to know its impact on the climate. |
| E. | Identifying the impact of the way we dispose of our waste. |
In the following section, we present studies with different approaches that aim to objectify the environmental impact of our professional activity with data on the previously listed points.
A. Medical Care
Healthcare and the associated expenditure vary greatly from country to country. In the U.S., it is more than 17% of GDP. A higher carbon footprint can be inferred from higher spending on healthcare. In the U.S., healthcare accounts for 10% GHG of the national total (Matthew 2020). In Australia and European countries, it is 7% (Malik 2018). The hospital and pharmaceutical sectors have the largest combined footprint (60%). This carbon footprint in the hospital sector was observed in a study in the U.K., which attributed 20% to buildings (electricity and gas) and 80% to clinical care (Tennison 2021).
Regarding hospitals as well as buildings, they consume 40% of the planet's materials, 30% of its energy and generate 20% of the solid waste stream. The ICUs of our hospitals, as structurally individual departments, can receive regular information on their energy expenditure with the aim of reducing energy and water use and initiating strategies with technicians and administrators.
Regarding healthcare, expenditure, and GHGs, they do not imply better outcomes and life expectancy (Bein 2023). It has also been studied how much of the GHG emitted would be avoidable. It was assessed that 10% of medical care is harmful, and 30% is low-value care (Barratt 2022). Reducing iatrogenesis and increasing adherence to "do not do" recommendations reduces burdens on the patient, expenditure, and the environment (Bein 2023).
Indeed, the deterioration of health caused by the unsustainability of the system perpetuates itself. Healthcare services themselves deal with a greater number of pathologies related to climate change, which leads to greater production of GHGs due to this new workload (Salas 2019; Sherman 2021).
B. Life Cycle Analysis
In healthcare and in our ICUs, a wide variety and quantity of materials enter, are used, and disposed of, each with its own life cycle (LCA) and environmental impact. Between 2005 and 2020, the use of disposable materials has more than doubled, and the use of PPE during the COVID-19 pandemic has exacerbated this (Statista 2022).
ReCiPe is a method that assesses LCA developed in 2008 through cooperation between Radboud University Nijmegen, Leiden University and PRé Sustainability. It aims to transform our huge inventory of various life cycles into a limited number of indicators. ReCiPe 2016 is an improvement of ReCiPe 2008 (and its predecessors CML 2000 and Eco-indicator 99). This method is updated (by Radboud University) to incorporate new data and research.
The scoring of these indicators expresses the relative severity in an environmental impact category. In ReCiPe they divide the indicators into 18 mid-point indicators and three end-point indicators. Each item is also evaluated according to its temporality, management expectations or technological progress. The ReCiPe framework includes advantages such as the use of global impact mechanisms, consensus modelling and long-term thinking based on the precautionary principle.
C. Material Flow Analysis
ICUs are a major contributor to CO2 emissions (Hunfeld 2022). They conducted a material mass flow analysis (MFA) in a university ICU in Rotterdam in 2019. The MFA was measured by analysing inputs and outputs of the ICU throughout the year in kilograms, average number of products used x number of patients/day and mass in kg of materials used per patient/day. The study was followed by an environmental footprint analysis. The secondary objectives of this study were to obtain data on mass, carbon footprint, water use and to determine the environmental hotspots in an ICU. The study, during which 2,839 patients were admitted in 2019, with an average stay of 4.6 days, showed an MFA of 247,000 kg during their ICU stay. Of this MFA, 50,000 kg was incinerated as hospital hazardous waste. The environmental impact per patient resulted in 17 kg of mass, 12 kg CO2e, 300 L of water use and 4 m2 of agricultural land occupation per day.
Five critical points were identified in this study: non-sterile gloves, isolation gowns, bed protectors, surgical masks and syringes (including packaging).
With this material flow analysis, it is clear that carbon net zero does not equate to zero environmental impact. Every day, pharmaceuticals and consumables that cause ecological damage and GHG emissions are used and wasted (Grand View Research 2021). Therefore, it is important to stress that there are processes with advantages over others (recycling compared to manufacturing), but they all have a negative effect. Furthermore, the best way to reduce the damage to the planet is to reduce consumption.
D. Carbon Footprint
In our daily lives, we should reach carbon neutrality, which is achieved when the same amount of carbon dioxide (CO2) is emitted into the atmosphere as is removed from it in different ways, which is called a zero carbon footprint. The current carbon footprint is mainly derived from human use. The first cause is fossil fuel combustion, and the second cause is deforestation. In addition, we generate a carbon footprint when we use products and when we dispose of them. Also, we far exceed our GHG generation in relation to the earth's capacity to buffer it.
We release pollutants into the air, either directly from the source or secondary to the interaction between different compounds in the atmosphere (ozone of nitrogen oxides in the presence of sunlight). Our biological stores of carbon are the oceans and forests. The Amazon rainforest stores up to 200 billion tonnes of carbon. However, 20% of its area has been deforested in the last 60 years, and it is still increasing exponentially. The causes of this are agriculture (soy: the main component of propofol, palm), oil, droughts, and fires caused by climate change (D'Amato et al. 2017).
To help us understand ourselves and initiate decarbonisation and ecological transition, we can use ScopeCO2 (at sanidadporelclima.es; free online tool), which calculates our carbon emissions, also from hospitals. In this tool, GHGs are calculated from the activity data entered by the user for the year of calculation. It distinguishes between emissions generated in sources owned and controlled by the healthcare institution, associated with electricity consumption purchased from the energy producer, and others, for example, generated by staff travel or patient transfer services.
In this tool, emission factors of the type of kg of CO2 per kWh of electricity consumed are applied, following the international GHG Protocol methodology and with data from the Spanish Climate Change Office (Ministry for Ecological Transition and the Demographic Challenge) and the National Commission for Markets and Competition for electricity.
The carbon footprint of the health sector is equivalent to 4% of global net emissions (McGain et al. 2020). In Spain, the ecological footprint is 2.6 times higher than the sustainable footprint. But improvement is possible. The U.K. NHS has achieved a reduction in its carbon footprint of 580 kt CO2e by 2021 (NHS 2020).
To help reduce this impact, fifty countries - Spain among them - committed at COP26 to developing climate-resilient, low-carbon health systems (COP26 Health Programme). Of these, forty-five committed to transforming their health systems to make them more sustainable and reduce their emissions. Fourteen countries even set 2050 as the target date for GHG=Zero.
The platform that brings together health actors committed to tackling the climate emergency is Health#ForTheClimate. Its aim is to help reduce the sector's carbon footprint and achieve carbon neutrality by 2050. This initiative is part of Community#ForTheClimate, a multidisciplinary platform with the aim of implementing the Paris Agreement and which has the support of ECODES, the company MSD and the collaboration of the social responsibility healthcare network.
E. Waste Disposal
Identifying the impact of the way we dispose of our waste. The scale of the problem is enormous. The NHS generated 624,000 tonnes of waste between April/19 and March/2020. Although ICU waste has not been systematically quantified, approximately 50% could be recyclable (McGain 2009). At the NHS level (Silva et al. 2021), 47% of waste was incinerated, 16% was recycled, 7% went to landfill, and the remainder underwent alternative treatments. Since the COVID-19 pandemic, medical waste has increased by up to 350% in some countries, mainly from plastic personal protective equipment (PPE).
Incineration does not completely destroy the waste and leads to further contamination of air, water and soil (Fang 2022). Studies have shown higher rates of cancer and perinatal defects in communities around waste incinerators (Thompson 2008).
Wastewater treatment plants are not designed to remove pharmaceuticals. Products are discharged into water (they have even been detected in drinking water) or used as agricultural fertiliser. According to the Swedish Chemical Agency, the environmental impact on water of these discharges depends on three factors of the products or pharmaceuticals: persistence (ability to resist degradation), bioaccumulation (in the fatty tissue of aquatic animals) and toxicity (potential harm). The impact of these factors on everyday drugs such as propofol (Mankes 2012; Favetta 2002), opioids, antibiotics (Gothwal 2015), lido and bupivacaine, sugammadex and paracetamol has been studied with disappointing findings. In that study, hazardous materials such as cadmium, chromium, dioxins, polycyclic aromatic hydrocarbons, BTEX compounds, sulphur dioxide, nitrogen oxide, etc., which are thrown away, have been found to cause, through ingestion, inhalation or topical absorption: respiratory, cardiovascular, gastrointestinal, renal and nervous system diseases. Plastic, despite its recycling, remains plastic, only decreasing its size or deteriorating its quality. Only paper has less impact, but its recycling is also associated with air and water pollution.
Special attention should be paid to the fact that 90% of oral medicines (mainly antibiotics and antidepressants prescribed on an outpatient basis) are excreted in wastewater as active substances (original dosage form or metabolites) via the faeces and urine of patients. As for the disposal of antibiotics, since wastewater is rich in nutrients and bacteria, this type of waste can lead to the development of antibiotic-resistant strains. This causes more than 33,000 deaths and the loss of more than 874,000 disability-adjusted life years/year in Europe (Cassini 2019). This will worsen with antibiotic resistance genes already detected in environmental samples.
In addition, detergents of hospital laundries also contribute to environmental damage (Fang 2022). These products have surfactants (which damage fish gills and increase vulnerability to toxins), phosphate (already banned), EDTA (which increases the bioavailability of heavy materials) or bleaching agents (hydrogen peroxide is biocidal).
The last step for any product may be landfilling, even after recycling it or treated in waste plants or incinerated. Landfills have been associated with public health risks. Methane, CO2, nitrogenous products, heavy metals, and bioaerosols (fungi, enterobacteria, endotoxins) can, through their contamination of soil, water and air, cause rhinitis, asthmatic flare-ups, and infections (Health Protection Agency 2011).
What is crucial is prevention, prioritising the least (Royal College of Anaesthetics 2022) and best first use. The impact of disposing of used items is impossible to be harmless nowadays. This is the reason for the COP26 Health Programme. In addition, in Latin America, the Health Care Without Harm Programme works to transform the global health sector to be ecologically sustainable and promote environmental health and justice, highlighting in 2022 the initiative “Hospitals that heal the planet”.
In Madrid, the Santa Cristina Hospital achieved full quality and environmental certification for all its processes in March 2022 with the development of a Management System based on the ISO 14001:2015 standard, minimising its impact on the environment and collaborating in the sustainability of its surroundings based on energy efficiency, water consumption and proper waste segregation. Its objectives include implementing legal recommendations and requirements, pollution prevention, sustainable use of resources, energy efficiency programmes, environmental commitment with its suppliers and promoting training for continuous environmental improvement.
The Hospital Universitario del Henares was inaugurated in 2008, with a polyvalent ICU which, following the COVID-19 pandemic, has sixteen structural beds. Its construction provided it with natural light, and it was defined as a paperless hospital. During the COVID-19 pandemic, we were overwhelmed by the large amount of waste from patient care. In the aftermath, we felt it was the ideal time to optimise our clinical practice for more sustainable critical patient care. Nevertheless, at the moment, all ICUs have in common several intrinsic aspects in their activity that make it difficult to achieve a GREEN ICU:
- Increased number of diagnostic and therapeutic procedures, especially in high-tech ICUs, which may even generate more GHGs without necessarily improving mortality, prognosis or patient comfort.
- Increased average life expectancy and comorbidity of our patients.
- Continuous activity of staff, resource use, and energy demands.
Knowing each other is essential to find solutions. We have already come a long way. The Drawdown Report (drawdown.org) is an international initiative launched by climate change scientists. It considers the hundred most practical options that, if implemented, may halt climate change in just one generation. There have been proposals for solutions focused on critical patient care for more than a decade (Chapman 2011) and even studies on it (Baid 2020). However, we need to have at hand a sustainability kit for our ICUs along the lines of those already developed by the Australian and New Zealand Intensive Care Society (ANZICS 2022). They are a guide for intensivists who want practical measures to reduce the carbon footprint of our ICUs. We present our approach where medical and environmental ethics walk hand in hand (MacNeill 2021).
Goals
The characteristics of our objectives are that they must be agreed upon, assumed by all, focused on the long term, with a real impact, and with a local and global scope with the aim of moving from a linear to a circular system and integrated into our work and personal identity.
- Primary objective: to train professionals who work in critical patient care and develop strategies to reduce the environmental impact of a sixteen-bed polyvalent ICU.
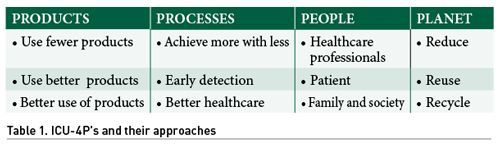
- Secondary objectives: focused on the 4Ps to cure and care for our planet, people must act on themselves, on the products and processes of critical patient care.
- Products
- Processes
- People
- Planet
Management: Research, Training, and Clinical Practice for a Sustainable ICU
The approach to the analysis of our situation must be holistic and integral, with the participation of the whole team and the evaluation of processes and results. This great complexity is an enormous opportunity to work together on different variables without having to use differentiated strategies that may conflict.
For an ICU to be sustainable, it needs measures to prevent its carbon footprint, resource use and waste management. It also needs to apply broader and broader concepts. Moving from the best available evidence-based medicine, having added patient-based medicine and now it is also time for planet-based medicine. A planet-based medicine that needs the 10 Rs: reject, rethink, reduce, reuse, repair, refurbish, remanufacture, reuse, recycle and recover.
A sustainable ICU is a concept of a non-linear but cyclical development. It is based on a dynamic equilibrium that allows self-regulation and feedback. According to the principle of subsidiarity, problems should be solved as close as possible to their source. This is where we are on the front line in our ICUs.
We need to know, through subsequent research and training, what to measure and how to solve each step of our clinical practice in a GREEN ICU. Following the secondary objectives set out above, we are going to order our suggestions for sustainability without implying this as an order of priorities.
Products
Use fewer products
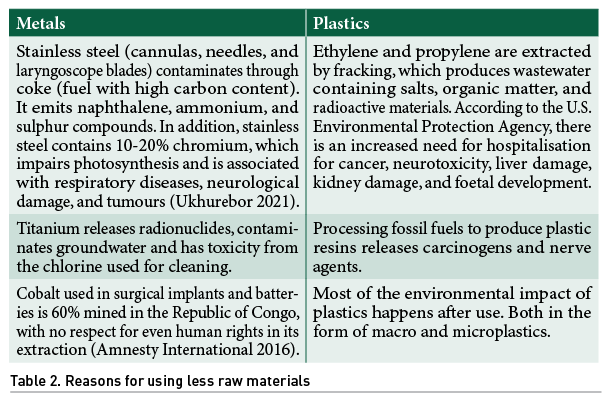
- Less use of raw materials in their manufacture (Table 2) (Fang 2022).
- Reduced use of single-use equipment. Gloves are the largest single-use product. Latex gloves contribute to deforestation because they require rubber. On the other hand, nitrile gloves are made from a petroleum-derived copolymer of acrylonitrile and butadiene. Highlight the GOSHs Gloves Off Campaign of the Great Ormond Street Hospital for children (NHS) with its mission to encourage health professionals to reduce the unnecessary use of non-sterile gloves.
- Fewer products, less local carbon emission from the energy in their manufacture.
- Reduced need for transport, reduced GHG emissions. NHS-related road transport is responsible for 3.5% of all journeys in England. It accounts for 7,285 tonnes of nitric oxide/year and 330 tonnes of particulate matter, mostly less than MW 2.5 (NHS 2020). Air pollution leads to 40,000 deaths per year in the U.K. so NHS-related transport could be responsible for 1,400 of those deaths (Royal College of Physicians 2016).
- Lower MDR rate, reduced need for isolations and rationalisation of the use of drugs, gowns, and gloves.
Use better products
- Purchase more energy-efficient technology and products.
- Ensure suppliers manufacture products and drugs (e.g., propofol) ethically and sustainably.
- Evaluate with manufacturers to remove redundant parts from devices already packaged as a set for use.
- Longer-lasting batteries, less polluting in their manufacture and disposal.
- Local products with a smaller ecological footprint in their transport due to the distance and means of transport.
- Use of bronchodilator inhalers, etc. with a lower carbon footprint.
- Use of drugs in more concentrated formulations.
- Purchase reusable versus single-use equipment. There are NIV face interface LCAs, breathing circuits, dressing boxes, bed linen.
- Plastic-free packaging.
Better use of products
- Adapt stocks to consumption of both medication and materials to avoid expiry.
- Better treatment of equipment that is used and can be repaired in situ by a biomedical engineer in a short period of time.
- Avoid using medicines, monitoring, and vascular accesses with little value in the healing process of that disease.
- Protocol cleaning of filters to improve air quality.
- Use perfusions that come from other places of care other than the ICU.
- Manufacture products with alternative substances to plastic.
Processes
Achieving more with less
- Digitalisation and use of intelligent technologies.
- Streamlining our processes: individualised protocols for each hospital and patient.
- Informed consent for admission and other techniques, data protection document without needing to sign them on paper. Transmission from the patient's unit or family information room with an electronic document holder via Wi-Fi to a SELENE form (our computer programme).
- Request for blood products with the double check on the form or consult the SELENE blood bank to avoid the use of paper.
- Individualisation of the need for consumables and diagnostic tests, both analytical and radiological tests.
- Individualised monitoring needs. Night mode of screens to save energy.
- Choose wisely' initiative: consider useful measures daily, rethink therapeutic objectives and in accordance with the patient's wishes (Auriemma 2019). Recommendations NOT TO DO in both adults and paediatrics (SEMICYUC 2019-Hernandez 2023).
Early detection
- Early detection of patients at risk, fewer ICU admissions due to optimisation of management on the ward or earlier admissions in ICU resulting in shorter stays due to less pre-ICU deterioration, and fewer readmissions due to post-ICU surveillance. The above, thanks to HEWS-type programmes (Abella 2023), would lead to lower resource consumption and waste generation.
- Early detection of MMR would lead to avoiding outbreaks with the consequent lower consumption of resources and generation of waste derived from the necessary isolations.
- Early detection of professional burnout with an adequate professional ratio to help continuous process improvement.
Better health care
- Training in our generated environmental effects and strategies to minimise them.
- Doing our healthcare right the first time: diagnosis, choice of antibiotics, surgery, avoiding malnutrition, etc. (Fang 2022). This would avoid complications, increased length of stay, waste, and costs.
- Digitalisation with access to data from other healthcare centres.
- Optimising monitoring and transmission of all possible data to the P.C. in the unit or via Wi-Fi of isolated patients in the ICU. These would avoid the use of gowns, gloves, etc., by avoiding the need to enter.
- Accurately predict the drugs amounts and which drugs we are going to use in our actions.
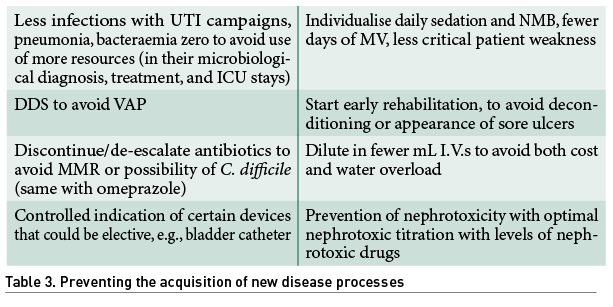
- Preventing the acquisition of new disease processes other than those that have led to their admission (Table 3).
- Improve information transmission (I.T.) to avoid duplication, errors or readmissions at the time of I.T. on transfer to the ward.
- Better menus adapted to disease and type of patient to avoid food wastage.
- Fewer changes in home treatment patterns and quicker reconciliation.
Persons
Health professionals
- Approach by healthcare professionals (Bein 2021) legal regulations and policies with a three-pronged strategy: ecological, social, and financial.
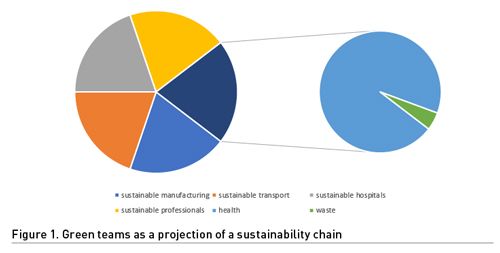
- Creation of "Green teams" with bottom-up initiatives (Bein 2023). Lead for coordinated work, being a collaborative and interprofessional work.
- Reducing therapeutic futility (Bein 2023). Intensive care interventions that prolong life without achieving effective patient-centred care are futile. Futile treatment brings harm to patients and caregivers, to the payer/taxpayer and to our environment. Ethical, ecological, and best clinical practice principles are often synonymous. Futility undermines human dignity and ecological ethics.
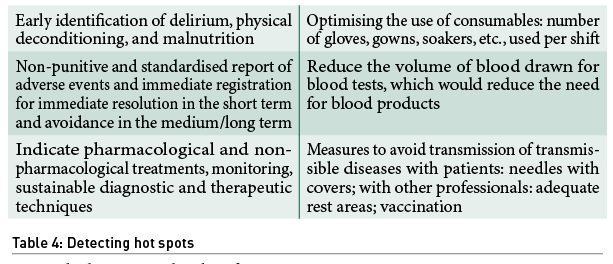
- Detection of areas for improvement in our daily life as hot spots (Table 4).
- On-call pass: optimising times for assistance and optimising transmission of information. (Salinas 2022)
- Zero waste in the staff room (reusable cups and bottles).
- Minimise staff travels.
- Calculate personal carbon footprint. Training and evaluation with CME/CPD activities for BJA Education subscribers.
Patients, families, and society
- The decision to admit or not a patient to ICU leaves its footprint on the planet either by promoting health (in the case of an appropriate and timely admission) or by deciding not to admit a patient in the case of futility, in the context of "non-maleficence" by avoiding further carbon footprint, waste, expense etc.
- Promote public health to reduce the need for healthcare or use of pharmaceuticals (Bein 2023). Educate on healthy lifestyles. Actively involve patients and families in the prevention of chronic and acute diseases (pandemics).
- Optimise preoperative and postoperative care (Lobo 2020), promote adherence to the Stockholm 'Wise List' of treatments, and not prescribe non-recommended treatments (Eriksen 2017).
- Family and patient education in self-care (diabetes, CVC, stomas, tracheostomies).
- Knowing what or how far a patient wants to be cared for (Popovich 2023), with shared decision-making. Matching patient and family expectations. Consult or offer the possibility of issuing advance directives.
- Accessibility, by using public transport to visit relatives in the hospital or for medical consultations.
Planet
The planet needs ecological management of the energy, waste, and consumables we use in our daily practice. The 10 R's stand for reject, rethink, reduce, reuse, repair, refurbish, remanufacture, reuse, recycle and recover. Globally, medical waste accounts for 4% of all plastic waste. During the COVID-19 pandemic, it accounted for 23% of total NHS waste. For a practical approach, we will break it down into the mantra (Bein 2023) of first, reduce waste; second, reuse if possible; and third, recycle.
Reduce
- Transition from carbonised energy systems to renewables to achieve an energy refurbishment of our buildings.
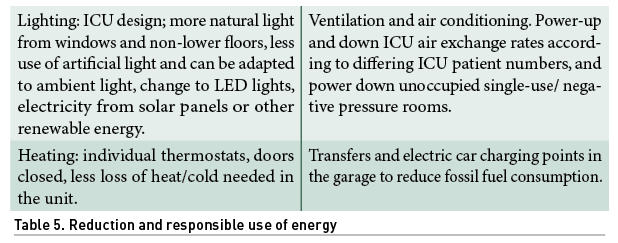
- Energy efficiency, reduction, and responsible use of energy (Table 5) (Hufing 2014).
Reduction of:
- Machines. MV-NIV devices and other machines with the best energy rating. Innovative technologies that cover a real need. Not being hostage to programmed obsolescence. Biomedical engineer available to make repairs.
- Fungibles: less waste generation by reducing the use of gloves and gowns.
- The type of packaging of our products.
- Paper and recycle, information to relatives on large posters at the entrance and Q.R. reading with instructions for visits, etc.
- Protocols and instructions for equipment, accessible by reading Q.R. codes or training pills in the hospital's continuous training app.
Reuse
- Circular management from fibrobronchoscopes, dressing boxes, NIV interfaces to packaging.
- Maximise the reuse of laundry linen for the same or other purposes.
Recycle
- "SIGRE point" SIGRE (non-profit entity in charge of guaranteeing the correct environmental management of the containers and remains of medicines that are generated in homes). Launched in 2001, the result of collaboration between the pharmaceutical industry, pharmacies, and pharmaceutical distribution companies, to be an effective and efficient model for medicines in solid or liquid formulations following safe disposal protocols, especially for antibiotics.
- Differentiated disposal in containers for glass, paper/cardboard, plastic, organic, batteries, and toners.
- Safe disposal of toxic materials, biohazardous materials, sharps, etc.
- Safe disposal of stool, diuresis (especially 24 hours after administration of contrasts), and patient bleeding, by means of appropriate filtering and treatment prior to disposal.
- Use of biodegradable materials
- Safe incineration
Conclusion
People have created the problem, and people must commit themselves to solving it. It is an ambitious plan that requires a mobilised society because of the scale of this crisis to be able to solve it successfully. Healthcare professionals, in addition to caring for our patients, can care for our planet in our day-to-day work by developing zero-carbon ICUs immersed in sustainable, more efficient, and cost-effective healthcare systems. There should be no ethical dilemma between the beneficence of health promotion and the non-maleficence of avoiding the deterioration of our planet.
We must plan and execute better processes to bring about real change in the quality of life for present and future generations in balance with the planet. To maintain that balance, we must move towards this shared goal. It is not an option to not accomplish it.
Conflict of Interest
None.
References:
Abella A et al. (2013) ICU without walls project. Effect of the early detection of patients at risk. Medicina Intensiva.
ANZICS (2022) Resources. Available at https://www.anzics.com.au/safety-quality-resources/
ANZICS. A beginners guide to Sustainability in the ICU. Sustainability toolkit evolved from the ANZICS 2020 NZ ASM and Australian Quality and Safety committee sustainability e-conference. ISBN: 978-1-876980-56-6.
ANZICS. Choosing wisely. Available at www.choosingwisely.org.au
Amnesty International (2016). This is what we die for: human rights abuses in the Democratic Republic of Congo power to the global trade in cobalt. London. Amnesty international.
Auriemma CM et al. (2019) Less is more in critical care is supported by evidence-based medicine. Intensive Care Med. 45:1806-1809
Baid H et al. (2020) Environmental sustainability of intensive care service provision: a systematic review. Prospero 2020 CRD42020205717.
Barratt AL et al. (2022) High value health care is low carbon health care. Med J Aust. 216:67-68
Bein T and McGain F (2023). Climate responsibilities in intensive care medicine—let’s go green! Intensive Care Med. 49:62-64.
Bein T et al. (2021) What’s new in intensive care: environmental sustainability. Intensive Care Med. 47:903-905
Carbon footprint registration, compensation and carbon dioxide absorption projects. Ministerio de transición ecológica. Available at https://www.miteco.gob.es/es/cambio-climatico/temas/mitigacion-politicas-y-medidas/registro-huella.aspx
Carbon footprint of the Ministry for the Ecological Transition and the Demographic Challenge. Available at https://www.miteco.gob.es/es/cambio-climatico/temas/mitigacion-politicas-y-medidas/informesHuella-MITECO.aspx
Cassini A et al. (2019) Attributable deaths and disability-adjusted life-years caused by infection antibiotic resistant bacteria in the E.U. in 2015. Lancet Infect Dis. 19:56-66.
Chapman and Chapman (2011) Greening critical care. Critical Care. 15:302
D´Amato et al. (2017) Climate change, allergy and asthma, and the role of tropical forests. World Allergy Organ J. 10.11.
Eriksen J et al. (2017) High adherence to the ‘Wise List’ treatment recommendations in Stockholm: a 15-year retrospective review of a multifaceted approach promoting rational use of medicines. BMJ Open. 7:e014345.
Fang L et al. (2022) Sustainability in anaesthesia and critical care: beyond carbon. BJA Education. 22(12): 456e465.
Favetta P et al. (2002) Propofol metabolites in man following propofol induction and maintenance. Br J Anaesth. 88:653-8.
Gothwal R et al. (2015) Antibiotic Pollution In The Environment: A Review. Clean-Soil Air Water. 43:479-89.
Grand View Research (2021). Medical plastics market size, share & trends analysis report by application (medical device packaging, medical components, orthopedic implant packaging), and segment forecast, 2021-2018. Available at https://www.grandviewresearch.com/industry-analysis/medical-plastics-market
Health Protection Agency (2011) Impact on health of emissions from landfill sites. London.
Hernández Borges A et al. (2023) Recomendaciones de «no hacer» en cuidados intensivos pediátricos en España: selección por método Delphi. Anales de Pediatría. 98(1):28-40
Hufing K et al. (2014) Environmental sustainability in the intensive care unit—challenges and solutions. Crit Care Nurs Q. 37:235-250
Hunfeld N et al. (2022) Circular material flow in the intensive care unit—environmental effects and identification. Intensive Care Medicine. 49:65-74.
Lenzen M et al. (2020) The environmental footprint of health care: a global assessment. Lancet Planet Health. 4:e271-e279.
Lobo B et al. (2020) Post-Intensive Care Syndrome - Patients and Families Need to Know They are Not Alone. ICU Management & Practice. 20(4):271-274.
Malik A et al. (2018) The carbon footprint of Australian health care. Lancet Planet Health. 2:e27-e35
Mankes RF (2012) Propofol wastage in anaesthesia. Anaesth Analg. 114:1091-2.
Matthew J et al. (2020) Health care pollution and public health damage in the United States: an update. Health Af (Millwood). 39(12):2071-2079.
McGain et al. (2020) Environmental sustainability in anaesthesia and critical care. Br J Anaesth. 125:680-92.
McGain F et al. (2018) The carbon footprint of treating patients with septic shock in the intensive care unit. Crit Care Resusc. 20:304-312.
McGain E et al. (2009) An audit of potentially recyclable waste from anaesthetic practice. Anaesth Intensive Care. 37:820–823
MacNeill AJ et al. (2021) Planetary health care: a framework for sustainable systems. Lancet Planet Health. 5:e66-e6.
National Health Service (2020) Delivering a “Net Zero” National Health Service. London. NHS England ang NHS Improvement.
Popovich J et al. (2023) Time-Limited Trials of Intensive Care Unit Care. JAMA Intern Med.
ReCiPe (2016) v1.1 A harmonized life cycle impact assessment method at midpoint and end-point level Report I: Characterization RIVM Report 2016-0104a. National Institute for Public Health and the environment. The Netherlands.
Royal College of Anaesthetics (2022) Environmentally sustainable anaesthetic practice e-learning. Available at https://www.rcoa.ac.uk/events-professional-development/education-professional-development/e-learning-anaesthesia
Royal College of Physicians (2016) Every breath we take: the life-long impact of air pollution. London: report of a working party.
Salas RN et al. (2019) Prioritizing health in a changing climate. N Engl J Med. 381:773-774.
Salinas I et al. (2022) Information Transfer as a Strategy to Improve Safety in ICU. ICU Management & Practice. 22(1):18-24.
SEMICYUC Guidelines and Recommendations (2019). Available at http://privada.semicyuc.org/temas/formacion/guias-de-practica-clinica/guias-y-recomendaciones-de-la-semicyuc
Sherman JD et al. (2021) Net zero healthcare: a call for clinician action. BMJ. 374:n1323.
Schraufnagel et al. (2019). Air pollution and no-communicable diseases: a review by the Forum of International Respiratory Societies. Environmental Committee, part 1: the damaging effects of air pollution. Chest. 155:409-16.
Silva ALP et al. (2021) Increased plastic pollution due to COVID-19 pandemic: Challenges and recommendations. Chemical Engineering Journal. 405:126683.
Statista (2016) Global raw material demand fr medical disposables by product group from 2005 to 2025. Available at https://www.statista.com/statistics/689249/demand-of-raw-materials-for-medical-disposables-product-type-worldwide/
Tennison I et al. (2021) Health care’s response to climate change: a carbon footprint assessment of the NHS in England. Lancet Planet Health. 5:e84-e92
Thompson J et al. (2008) The health effects of waste incinerators: 4th report of the British Society for ecological medicine. Second Edition. London.
Ukhurebor KE et al. (2021) Effect of hexavalent chromium on the environment and removal technique: a review. J Environ Manage. 280:111809.
Other links of interest:
http://www.green.harvard.edu/greencarpet
https://blogs.brighton.ac.uk/sustainablecriticalcare/
https://hoopcarpool.com/informe-drawdown/
https://link.springer.com/content/pdf/10.1007/s00134-022-06940-6.pdf?pdf=button
https://pre-sustainability.com/articles/recipe/
https://semicyuc.org/wp-content/uploads/2018/08/50x70cm_no_hacer_todos_grupos-03_0.pdf
https://sustainablehealthcare.org.uk/
https://twitter.com/hope_enpie/status/1628687344835391489?t=Y0NszQvHl5bAWoDV6guELA&s=08
https://www.bjaed.org/cme/home
https://www.crd.york.ac.uk/prospero/export_record_pdf.php
https://www.gosh.nhs.uk/news/gloves-are-off/
https://www.sccm.org/Clinical-Resources/ICULiberation-Home/ABCDEF-Bundles https://www.sigre.es/conocenos/#que-es-sigre









