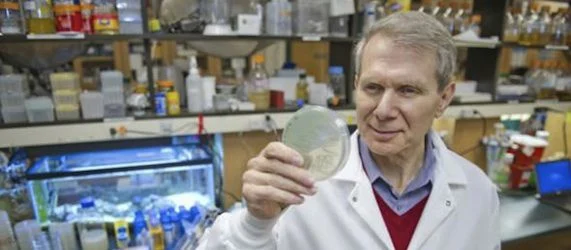
According to a pioneering study recently published in the journal ‘Nature’, the work of University Distinguished Professor of Biology Kim Lewis has led to a promising new approach in the treatment for and elimination of the methicillin resistant staphylococcus aureus, or MRSA.
This powerful antibiotic-resistant bacterium, dubbed the "superbug", is responsible for contaminating of over 1 million Americans each year. Patients subsequently develop entrenched chronic infections such as bone infection (osteomyelitis), heart infection (endocarditis), or infections of implanted medical devices that are, in most cases, incurable, even with appropriate antibiotic treatment.
MRS-type bacteria have gradually developed to actively resist certain antibiotics, generating major interest among medical and scientific communities. As Director of Northeastern's Antimicrobial Discovery Center, Lewis approached his research based on his suspicion that a different adaptive function of bacteria might be the real cause that has rendered these infections so destructive.
Together with his research team Lewis spent more than a decade studying a specialized class of cells produced by all pathogens called persisters, which, according to Lewis, had no other function than to survive. They posited that by killing these expert survivors, they could potentially cure chronic infections such as MRSA, traditionally resistant to multiple antibiotics. Brian Conlon, postdoctoral researcher in Lewis' lab and first author on the paper, stated that if persisters could be eradicated, the chance of resistance developing the first place could be decreased as well.
Lewis found that persisters succeed in their survival by entering a dormant state, rendering them impermeable to traditional antibiotics, which work by targeting active cellular functions. As a treatment has been completed, the cells reawaken and allow for the infection to re-establish itself.
For his scholarship in the field Lewis was elected to the American Academy of Microbiology in 2011.
Findings of the study, to which assistant professor Steve Leonard of the Department of Pharmacy Practice also contributed, show that drug called ADEP successfully wakes up the dormant cells and then activates a self-destructing mechanism. During the laboratory experiments, this approach entirely eradicated MRSA cells, even in a mouse model of chronic MRSA infection.
Conlon noted that by coupling ADEP with a traditional antibiotic, the team was able to completely obliterate the entire bacterial population.
As is the case with all other antibiotics, actively growing bacterial cells are expected to grow resistant to ADEP. Lewis is confident however, that cells become rather wilted during this process. Drugs such as rifampicin or linezolid have proven successful in the fight against ADEP resistant cells and provide a potent cocktail that kills persisters and is able to eradicate ADEP-resistant mutant bacteria.
Dr. Richard Novick of New York University's Langone Medical Center and a leader in the field praised the research as an extraordinary consequence of Kim Lewis’ groundbreaking work on bacterial persisters, and said it represented a most creative approach in this era of fading antibiotic utility.
Lewis' team are of the opinion that while ADEP is aimed at MRSA, similar components will be of use for treating other infections and disease models that can only be conquered via the elimination of the rogue cell population such as cancerous tumours.
Several are already being pursued.
Source: Science Daily
13 November 2013
Latest Articles
MRSA, antibiotic resistance, medical research
According to a pioneering study recently published in the journal ‘Nature’, the work of University Distinguished Professor of Biology Kim Lewis has led...