Findings from the HOT-COVID Randomised Clinical Trial, just published in JAMA, were presented at #ISICEM24.
COVID-19 pneumonia often leads to hypoxaemic respiratory failure, necessitating high levels of supplemental oxygen and intensive care. Previous recommendations suggested maintaining peripheral oxygen saturation (Spo2) between 90% and 96%. However, uncertainty remains regarding optimal oxygenation strategies in critically ill COVID-19 patients. Previous studies on oxygenation targets primarily focused on invasively ventilated patients, while newer approaches like noninvasive ventilation and high-flow nasal oxygen are increasingly used but lack robust evidence.
A subgroup analysis from the Handling Oxygenation Target in the Intensive Care Unit (HOT-ICU) trial trial suggested that targeting a Pao2 of 60 mm Hg may lead to more days without life support, though mortality at 90 days remained unchanged. To address this, the Handling Oxygenation Targets in COVID-19 (HOT-COVID) trial aimed to determine whether targeting a Pao2 of 60 mm Hg compared to 90 mm Hg could increase the number of days alive without life support in 90 days among ICU patients with COVID-19 and severe hypoxaemia.
This was a multicentre randomised clinical trial involving 726 adults with COVID-19 who received at least 10 L/min of oxygen or mechanical ventilation in 11 ICUs across Europe. .The 90-day follow-up concluded on June 1, 2023.
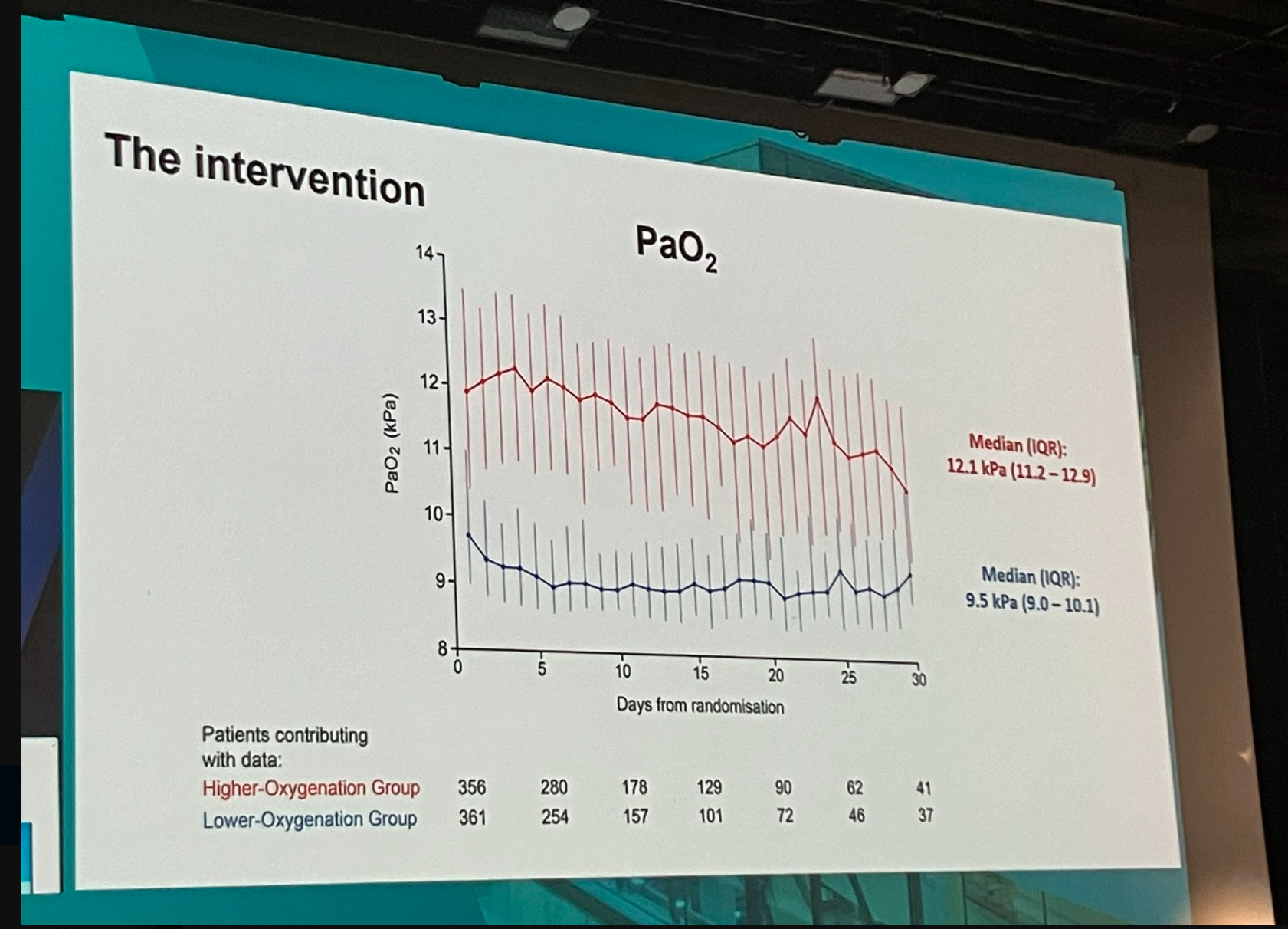
Patients in the study were randomly assigned in a 1:1 ratio to either a lower oxygenation group targeting a Pao2 of 60 mm Hg (n = 365) or a higher oxygenation group targeting a Pao2 of 90 mm Hg (n = 361) for a period of up to 90 days in the ICU.
The primary outcome of the study was the number of days alive without life support interventions such as mechanical ventilation, circulatory support, or kidney replacement therapy at 90 days. Secondary outcomes included mortality rates, the proportion of patients experiencing serious adverse events, and the count of days survived outside the hospital at 90 days.
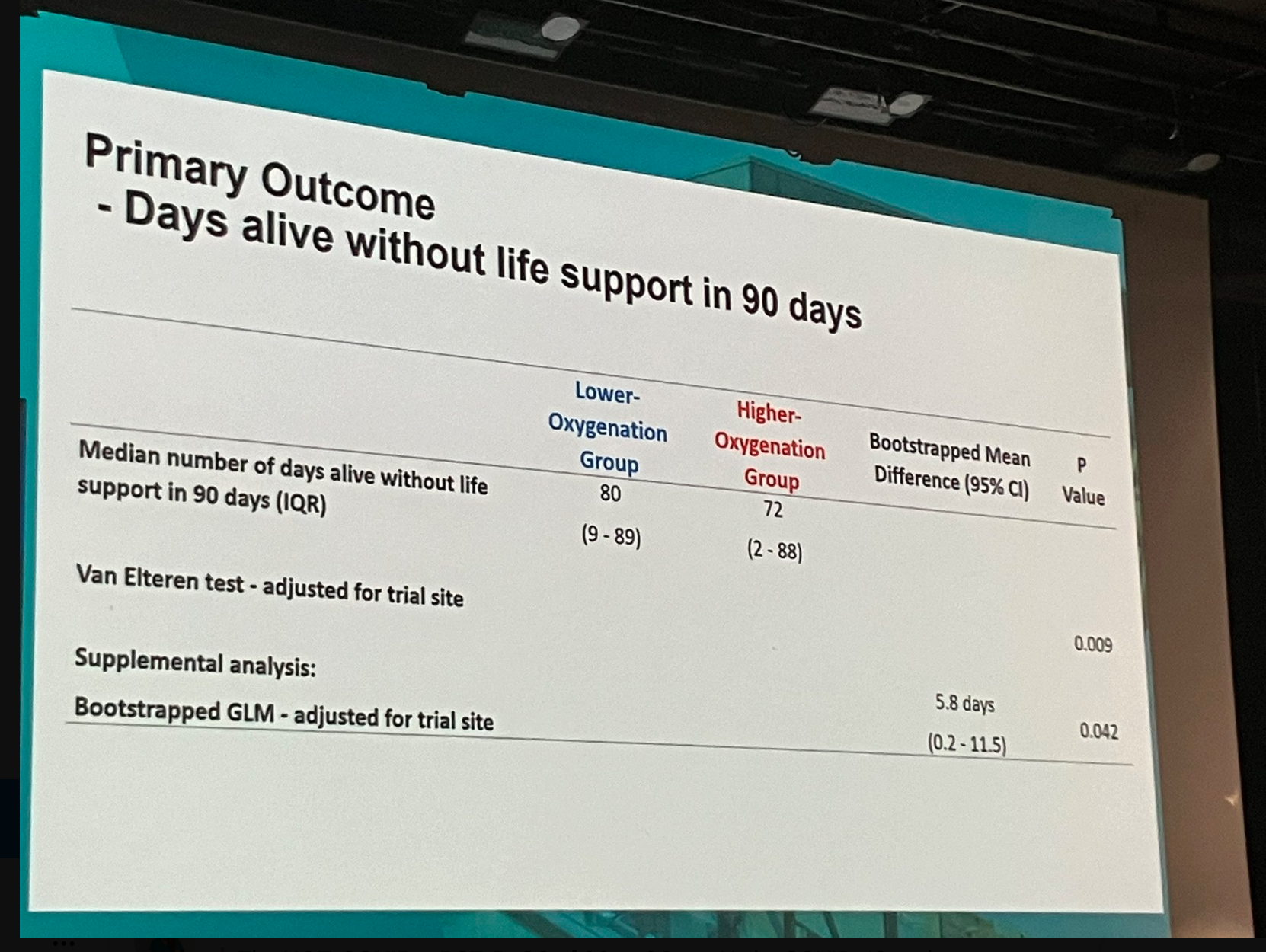
Out of the 726 patients initially randomised, primary outcome data were analysed for 697 individuals (351 in the lower oxygenation group and 346 in the higher oxygenation group). The median age was 66 years, with 495 patients (68%) being male. At the 90-day mark, the median duration of survival without life support was 80 days in the lower oxygenation group, compared to 72 days in the higher oxygenation group. Mortality at 90 days was 30.2% in the lower oxygenation group and 34.7% in the higher oxygenation group. No statistically significant differences were observed in the proportion of patients experiencing serious adverse events or in the number of days they survived outside of the hospital.
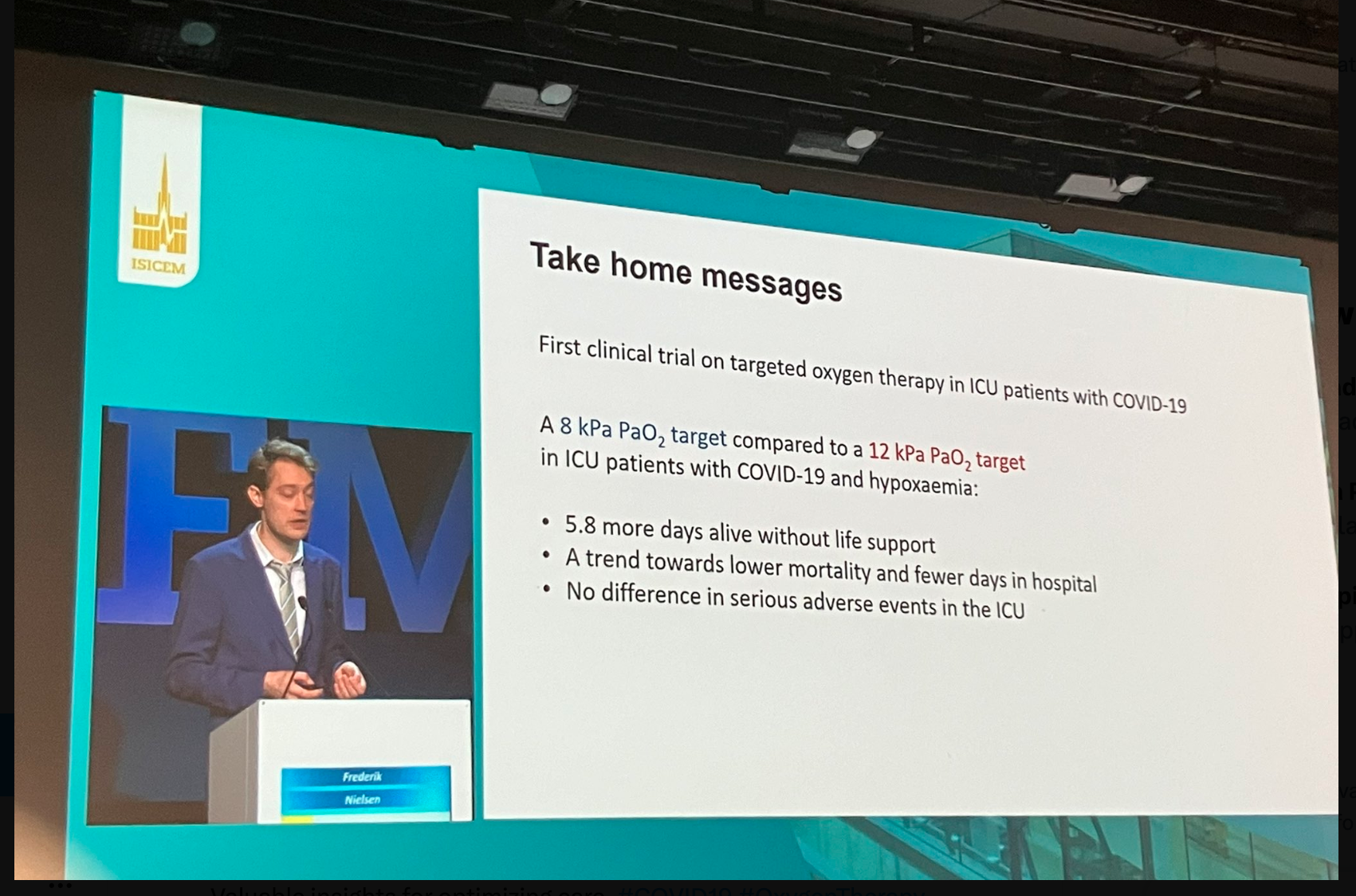
Overall, these findings show that in adult ICU patients with COVID-19 and severe hypoxaemia, a Pao2 of 60 mm Hg led to a greater number of days survived without requiring life support over a 90-day period than targeting a Pao2 of 90 mm Hg.
Source: JAMA, ISICEM 2024
Image and Slide Credit: ISICEM