HealthManagement, Volume 15, Issue 2/2013
Author
Christopher Kim
Associate Professor, Internal MedicineAssistant Professor, Pediatrics and Communicable Diseases, Associate Chief of Staff, Office of Clinical Affairs
Associate Medical Director, Faculty Group Practice, University of Michigan Health System
[email protected]
Hospital-based patient care has become more complex over time, with higher acuity of cases, and greater need for care coordination among all healthcare providers. And, for most patients, being hospitalised can be a harrowing new experience that they hope will go well. However, a fundamental and integral part of patient care—that is, to engage and partner with the patient and their family members in all aspects of their care—has sometimes become lost among all the other duties placed on healthcare providers.
Healthcare providers spend a considerable amount of their time complying with documentation requirements, ensuring quality and safety checklist have been completed, and discussing the patient case with other care providers. While these activities are important in making the healthcare organisation “run”, it is just as important (if not more), to ensure that healthcare organisations strive to provide a patient-centred experience through the entire hospitalisation.
The Unit Based Leadership Model
There are different approaches a healthcare organisation may take to meet the goal of providing patient-centred care in the hospital. One strategy that hospital based leaders might consider is to implement a local unit based leadership model to champion the patient-centred approach. In an article describing our organisation’s approach to organising and managing a unit based leadership model, we describe the selection process of the unit based leaders, the goals established for the units, and the support that they can expect to receive to accomplish those goals (Kim et al., 2012). The central point of this model is founded on the idea that broad institutional strategic decisions are developed at the senior leadership level, but the execution of these strategic goals are accomplished at the level of direct patient care.By establishing a unit based medical director to partner with a nurse leader on the unit, they can monitor the patient care activities where they are doing well, and selectively identify areas where they need to improve. Together, they can work with the unit based primary and support staff (e.g. nursing,pharmacy, therapists, case managers and social workers, nutritionists, clerical and custodial staff) and the physician teams to improve the culture of the interdisciplinary workplace, focus on quality, safety and efficiency initiatives, and enhance the patient’s hospital care experience. There are established metrics for each of these categories, and it is important that the hospital leadership provides these data to the unit based leaders, along with their targets.
Rating Patient Experience
For U.S. based hospitals, the patient care experience rating for each hospital is publicly available through the Centers for Medicare and Medicaid Services’ Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey(http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/HospitalHCAHPS.
html). These surveys administered to adult patients recently discharged from the hospital,report measures on topics such as nurse communication, doctor communication, responsiveness of hospital staff, pain management, communication about medicines, discharge information, cleanliness and quietness of hospital environment, and overall rating of hospital and willingness to recommend hospital. Beyond helping patients compare how hospitals perform relative to these measures,
some of these measures are also used to calculate incentive payments to hospitals.
For hospital based leaders to be able to improve on these patient-centred experience measures, they need to first have a good understanding of the local care environment, which is where the unit based leadership model can be beneficial. As the front line leaders, and with first-hand experience of providing patient care on those units, the medical director and nurse manager are well positioned to identify specific target areas and work with staff to facilitate patient-centred care. To accomplish this goal, the unit based leaders should be supported in their work in the following areas.
First, while most people can recognise good service and experience when they receive it, it is not always intuitive to understand what it takes to deliver good service. The selected leaders on the unit should be identified based on their commitment to improving the mission of the organisation, and to assist them in this goal, they should be trained in what it
takes to deliver patient-centred care. A training programme on customer service enhancement may be helpful, but healthcare service excellence needs to also incorporate the patient and their families into the patient care model. Additional training on patientcentred care, through conferences, seminars, and talking with patient and family advisory councils are just some ways in which the unit based leaders can keep updated and receive feedback on the latest practising enhancements to patient-centred care.
Second, the clinical leaders at the unit level need to model the behaviour of practicing interdisciplinary rounds at the patient’s bedside. This concept may be foreign to some services, but is a model of care that has been utilised and improved over time by other services. For example, in the field of paediatrics, there has been recognition of the need to work closely with family members in all decision making in the hospital as integral partners in the child’s care. In our organisation, it was the paediatric unit leaders that have incorporated the idea of conducting inter-disciplinary bedside rounds. The members of the healthcare team usually include the physician team (students, residents, and attendings), nursing staff, the case manager, social worker, and pharmacist, who meet with the patient and family at the bedside to discuss the plans for the day, as well as address any questions that the patient/family or any of the team members may have to clarify these outstanding issues at the bedside. This requires careful coordination, and so clear expectations about the timing of these rounds, as well as informing the appropriate staff that their patient is next in line for these rounds is critical, and the unit leaders help to work on continuously improving this practice. The adult care hospital can also adopt this practice to conduct patient centred discussions at the bedside, and the unit based leaders can help to coordinate this workflow as well as develop the script for the care providers to discuss with their patients.
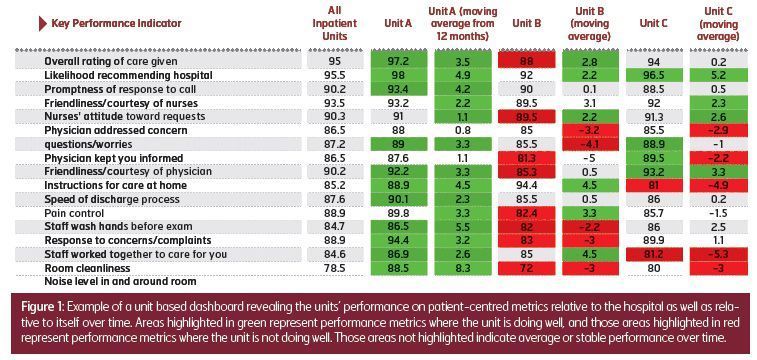
Last, the unit leaders need data in the form of a dashboard that can let them know how they are doing relative to these patient centred measures over time, as well as how they compare to the other clinical units in the hospital. The measures of HCAHPS data are delayed, and thus many hospitals utilise surrogate survey data from either the same survey vendors that conduct the HCAHPS, or internally developed questions. These data should be summarised for the unit leaders, that can clearly show the areas that they are doing well in (green) to those areas where they are stable (white) to those areas that they need to improve (red) at one glance—see figure 1. Additional information through patient comments collected should also be made available to share with the unit’s staff on both praise and improvement opportunity comments.





