HealthManagement, Volume 18 - Issue 3, 2018
With
the advent of smart hospitals, the digital future of clinical medicine calls
for a new ethical framework.
Fact:whether you like digital medicine or not—it is already here. Also true: facts do not hold normative power—the presence of breathtaking technological progress A is by no means a pro-ethical argument to use A. Artificial intelligence (AI) emerges, medicine transforms, and then clinics, as a core part of the health system, change step-by-step. But when it comes to digital health, Peter "Spiderman" Parker‘s Uncle Ben was right: "With great power comes great responsibility". Digital health ethics are discussed widely among academics and practitioners as well as in legal and economic realms. Legislators and nongovernmental organisations (NGOs) are paying attention to the debates. For example, the World Medical Association issued the Declaration of Taipei on ethical considerations regarding health databases and biobanks (2002/2016), and the German Ethics Council has discussed the ethics of big data and health (ethikrat.org/themen/forschung-und-technik/big-data). Hospital ethics committees are starting to reflect on digital transformation issues. The idea of patient experience at the very heart of the digital revolution in the clinical sector can be viewed under the economic paradigm fostering the ‘patient=client’ approach or the ethical paradigm nurturing the ‘patient=duty for welfare’ approach. Or both? When it comes to the smart hospital trend, deep integration of digital technologies into cure, care and management is—as a matter of fact—irreversible, and—as a matter of values—a very important and wide ocean of ethical issues to address. This importance extends to doctors, researchers, students, patients, nurses, digital experts, management, founders, industry professionals and many others in all areas of medicine, management, healthcare and hospitals, as well as other industries—and, last but not least, to the general public. Time to sketch some possible elements and fields of action toward smart hospital ethics.
In the long history of medicine, there has never been a period of such profound innovations as radical as digital transformation. Digital medicine is not an entirely gradual development, but changes medicine at its core. At the same time, the habits of most social contexts change, becoming more digital, and attitudes towards and handling of prevention, health, disease and cure change as well. Consequently, doctors, nursing stuff and management/administration staff adjust their relationship to patients (and themselves). Hospitals nowadays have to operate digitally, and target patient-oriented clinical services more consistently, including potentially positive results for patients as well as medical staff.
Why do we need smart hospital ethics?
The vigour of technical developments is steadily growing also in the hospital sector. A surgery robot is already almost retro. Understandably this increases society’s request for a certain degree of responsibility in this process. An example is the highly relevant debate over data protection. If hospitals are seen as seas of data in the future that medically and economically have a lot to offer, the legal question over data rights and the corresponding obligation of handling data appropriately quickly arises.
The introduction of the electronic patient record is, when thought through to the end, a rich source of new challenges, such as the possibility of amalgamating patient data and gaining new insights. Who owns these insights, who should obtain them and why, who might apply them and for what? As with all legal considerations, the basic problem is that these are normatively bound to a specific time and location and therefore not universally valid. Just as the investment sector hedges legal options, for example, to save taxes or reduce liability risks, so must imaginably different data protection cultures be weighted.
You might also like: Future medicine, today's healthcare
In a state under the rule of law we can justifiably hope that there is a major intersection between positive statutory and ethical standards. Nonetheless, first this intersection will never be complete and second, the rule of law and digital products are intangible. In addition, actual law and consequently real jurisdiction are lagging far behind technological development. This highlights the need for early and consistent reflection on the gap between facts and the ethically desirable. Technology assessments are needed to investigate developments in the digital realm of medicine and provide substantial insights and decision-making support in clinics and elsewhere.
The overall smart hospital system comprises many individual units, topics, players and processes of high complexity that lead to specific questions that in the analogue world were unable to evolve. Although many conceivable questions and prospective responses developed already in specific contexts relating to digital medicine, the overall view is of particular importance, because the smart hospital is a huge internal (doctors, nursing staff, management/administration, scientists, etc.) and external (patients, referrers, etc.) change process where an adequate basis of shared values can provide orientation.
Possible heuristic questions
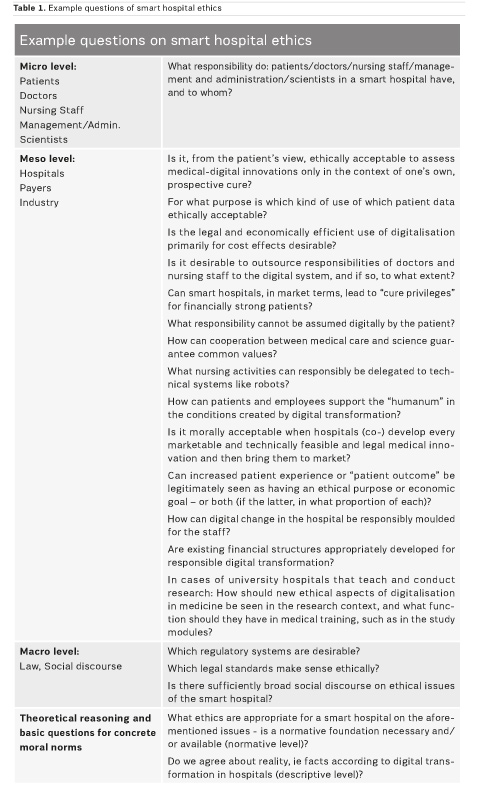
Table 1 includes example questions that are by no means exhaustive. They are designed to inspire us with new questions, stimulate hypotheses or invite criticism. An ethical view of hospitals is nothing new and is often the essential base of religiously-inspired establishments such as Christian hospitals. However, digitalisation generates a new material aspect that requires ethical considerations—if it is in fact true that for a reasonable moral conclusion normative (at least one) and descriptive premises need to be intertwined.
There are a multitude of specific application questions about new digital medicine, along with completely new questions. It is, for example, conceivable to transfer the well-known trolley experiment (an old but very helpful thought experiment developed by Philippa Foot in 1967 - trolleydilemma.com), which asks important ethical questions on decision theory and ethics, into the clinical area. How can and should AI decide, when a choice has to be made between two alternatives, when careful balance is required and the situation is complicated because the relevant values have equal weight? Assume there is only one special autonomous surgery robot and two patients who, based on human judgment, need the same surgery: an old and a young man. Without surgery the chances of survival are extremely low. An operation is needed immediately. An algorithm statistically evaluates the situation, and its choice might differ from the human’s. Why? Is that legitimate?
A real-world example is the genome testing company Nebula Genomics set up by Harvard professor George Church to address the B2C2B market for genetic data via blockchain, with no middlemen needed for private persons to market their DNA data. Human genome sequencing costs decreased dramatically from $ 100,000,000 in 2001 to under $1,000 today (Grishin et al. 2018). In principle, smart hospitals could develop and offer similar services or cooperate with innovative game changers. What ethical questions arise when hospitals start to become game changers in the digital realm?
To face these and other conceivable scenarios it is necessary to ask theoretical ‘raison d’être’ questions, given that individual ethics for every problem do not exist.
Hospitals’ responsibility for critical reflection and development
Over the past 30 years, many different hospital ethics committees were initiated in many developed countries, not least to consider questions and answers on technological development in the medical sector. Tasks include regular and also internal consulting, concrete assessment of specific medical and nursing situations as well as training. Their institutional embedding ranges from real control and decision functions to purely advisory tasks.
Mostly, the critical success factor is institutional independence and whether ethics committee members remain silent. It makes sense, particularly in a new field like digital transformation in a hospital, to establish a new initiative alongside the existing ethics bodies, to focus completely on the new questions and offer solutions in the smart hospital context.
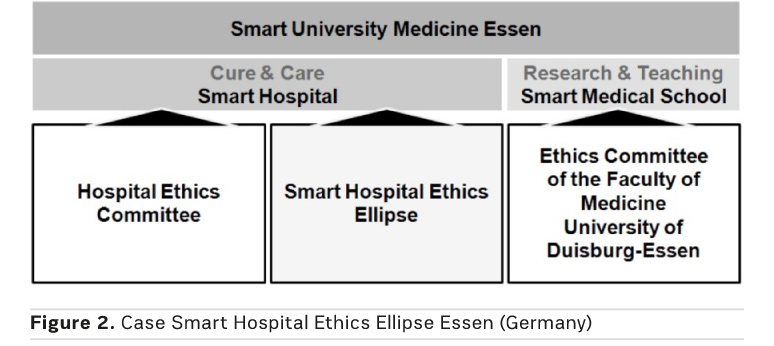
Engaging with the new ethics
An example of appropriate engagement with a new ethical body accompanying digital reorientation is the Universitätsmedizin Essen (Essen University Hospital). As a smart hospital, the Universitätsmedizin Essen does not follow the usual procedure of primarily using the digitalisation strategy to enhance efficiency and economy, but as a principal opportunity to improve patient care and unburden staff from tedious and time-consuming administrative tasks, and to innovatively increase quality in order to better take care of patients with value-driven empathy, a human core competence that cannot be expected from algorithms. It is the focus on humanity that transforms a digitally oriented hospital into a smart hospital. If teaching and research join forces in a smart medical school with the same ambition, this can be regarded as smart university medicine. The Universitätsmedizin Essen is on its way to becoming the ‘Smart University Medicine Essen’.
Successful change from a hospital of the present to a smart hospital of the future is not only a technological question, but encompasses internal and external cultural change. This includes the mindset and behaviour of all hospital personnel. The challenge is to set aside one’s own needs and focus on patients without any reservation; in particular, being aware of the changes to one’s profession—even reputation. Already the doctor is no longer the exclusive knowledge bearer and decision-maker on whether people live or die. Doctors have the chance to use the benefits of digitalisation to intensify their real strength: trustful and empathic care of their patients. Thus, patients experience warm, individual and digital medicine. Doctors, nurses, managers and administrators will have more time and digital resources for their professional expertise to agilely, healthily and successfully act in terms of patient care, teaching and research and more. The technical staff of the smart hospital will have more time to provide good advice and to answer individual questions.
This change also affects patients, whose positive experience is at the heart of the smart hospital. Strengthening patients’ personal competence, focusing on the cooperative interaction between doctors and patients from both directions, healing medically instead of industrially is what it is all about. On the patient side, it aims to reduce the conflict between the desire for safety and need for self-determination. This offers the opportunity for the general public to benefit more from high-end medicine. A new digital maturity is becoming conceivable and livable for patients in the smart hospital: more self-responsibility, more transparency, more cybersecurity, and most of all more quality care within the context of patient outcome.
A smart hospital does not produce health. It generates honest, empathic, first-class and highly professional basic conditions for recovery, and as a partner of patients it individually designs their prevention plan and aftercare. This relationship between scalability and individualisation can only be achieved via digital transformation: an economically successful hospital with individualised top medicine can hardly be viewed otherwise. Dignity is not a marketable product, but without digitally transformed scarcity management and innovative medicine it is in constant institutional conflict with markets and competition.
Conclusions
The path to a smart hospital with more hospitality, a sense of wellbeing, trust and warmth for patients and staff with patient-centric attitudes can only be successful if the broad topic areas of the fundamentally connected ethical aspects are closely integrated into this massive change process. Thus, what can (feasibility), want (emotions), and shall (ethics) we welcome?
Hospitals of the future will successfully endure when the opportunities of digitalisation are closely oriented to patient needs and not economic success, which will anyway result from a successful reorganisation process.
Without ethical reflections, the above-mentioned stances of the Universitätsmedizin Essen regarding their own digital transformation are hardly justifiable. An economic bottleneck, legally secured, would not render digitalisation unworkable. But maybe in the sense of what has been outlined above: because in that context success can only mean success for patients and staff that on a purely economic-legal basis is harder to achieve and impossible to legitimise. Even though in this case the Universitätsmedizin Essen is not a profit-oriented but a state-owned organisation. Considering that the U.S. healthcare company Kaiser Permanente has annual sales in 2016 almost equal to the state of Luxembourg (Siegel 2016) and the German private hospital group Helios manages more than 30,000 beds, it indicates what direction the journey is headed in. It is remarkable, to define digitalisation also as, but not only or even primarily, a returns driver.
Critical ethical reflections on different dimensions of the smart hospital are important. Ethics must not come too late but should guide technological, legal and economical perspectives; the speed of technological development is, to some extent, breathtaking.
The smart hospital Ethics Ellipse has been initiated from the Management Board of the Universitätsmedizin Essen to develop scientific, clinical and industrial proposals and recommendations and to support the Universitätsmedizin Essen in further implementation of the smart hospital. Against the background of plausible expectation for a diversity of questions, sharing multiple perspectives seems appropriate (Figure 2). Cooperation will guarantee solid development of medicine, economy and ethics that, first and foremost, has one goal: to optimally address the needs of patients.
References:
Capurro R (2017) Digitization as an ethical challenge. AI & Soc 32: 277–83.
Grishin D, Obbad K, Estep P et al. (2018) Blockchain-enabled genomic data sharing and analysis platform, v4.52. Nebula Genomics. Available from nebulagenomics.io/assets/documents/NEBULA_whitepaper_v4.52.pdf
Heinemann S (2018) Future medicine, today's healthcare – is the “smart hospital” a chance for change? HealthManagement.org The Journal 18(1): 68–70.
Heinemann S, Miggelbrink R (2011) Medizinethik für Ärzte und Manager. In: Thielscher, C. (Hrsg.), Wiesbaden: Medizinökonomie, pp. 107–44.
Hösle V (2004) Morals and politics. Notre Dame, IN: University of Notre Dame Press.
Siegel R (2016) What if healthcare could start with technology? — Bernard Tyson, CEO Kaiser Permanente. Stanford Business School, The Industrialist’s Dilemma, 21 Feb. Available from medium.com/the-industrialist-s-dilemma/what-if-healthcare-could-start-with-technology-bernard-tyson-ceo-kaiser-permanente-5052658a6212
Sulmasy LS, López M et al. (2017). Ethical Implications of the electronic health record: in the service of the patient. J Gen Intern Med 32(8): 935–9.
Werner JA (2018) Smart Hospital: Im Mittelpunkt steht der Mensch. Macwelt, 30 Mar. Available from macwelt.de/a/smart-hospital-im-mittelpunkt-steht-der-mensch,3448853
World Medical Association (2002/2016) WMA Declaration of Taipei on ethical considerations regarding health databases and biobanks, Adopted by the 53rd WMA General Assembly, Washington, DC, USA, October 2002 and revised by the 67th WMA General Assembly, Taipei, Taiwan, October 2016. Available from wma.net/policies-post/wma-declaration-of-taipei-on-ethical-considerations-regarding-health-databases-and-biobanks







