HealthManagement, Volume 17 - Issue 4, 2017
How much do clinicians—and patients—really know about the likely outcomes of the decisions they make, and how can we help them know more?
Should I start taking statins? Should I go for a breast cancer or prostate cancer screening test?
Or even just should I take another ibuprofen for my backache—that headline about them potentially causing an increased risk of a heart attack pops into my mind…

Our lives are full of decisions that relate to health, whether as healthcare professionals or simply as individuals, and when we make those decisions— even small ones—we are weighing up the potential risks and benefits in our heads. But how many of us actually know what those risks and benefits really are? A recent meta-analysis of the understandings of both patients (Hoffman and Del Mar 2015) and clinicians (Hoffman and Del Mar 2017) showed a consistent problem: even specialist clinicians tend not to be aware of the actual figures for treatments they work with regularly. Hence patients and clinicians are often making decisions without really understanding what is likely to happen as a result.
What are the chances?
This situation is clearly not ideal. Clinicians I speak to resoundingly say that they don’t feel that they have access to the information they need, and they don’t feel confident that they can explain it to patients either—and the evidence backs that up. A recent paper reported how less than half of patients enrolled on a large, multi-centre clinical trial understood the potential risks and benefits to them, even after receiving extensive information about it (Diemert et al. 2017). The authors, in classic understatement, described this
as ‘suboptimal’.
At the new, philanthropically-funded Winton Centre for Risk & Evidence Communication at the University of Cambridge, UK, we to aim to tackle these problems: to help bring together the best evidence available and to help communicate it to both clinicians and patients.
Predict
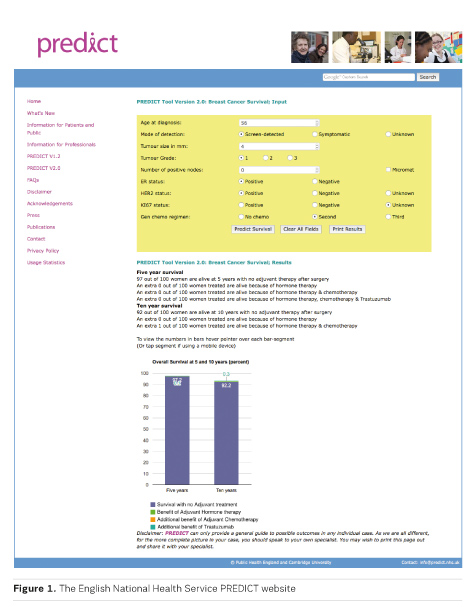
One project we are working on is the English National Health Service Predict website (predict.nhs.uk) (Figure 1). This uses a risk prediction algorithm to calculate the likely outcomes for women who have had surgery for breast cancer depending on which adjuvant treatment path they follow. It’s a site that has been publicly available for many years and currently has around 20,000 users each month from all around the world. Many oncologists use it regularly in their decision- making. From a patient’s perspective, however, the site is difficult to use and easy to misunderstand— it’s not remotely designed for them and yet is publicly available.
Our job, then, is to make Predict not just suitable, but useful, for patients: ideally used in consultation with their clinician, but it should also be useful to patients who might use it themselves at home to discuss with their families.
From the perspective of a clinician, Predict is very helpful in that you can quickly input details of an individual patient’s condition, along with your proposed treatment, and it will output a bar chart showing that patient’s predicted outcome (in terms of survival) at 5 or 10 years. The perspective of a patient, however, is vastly different.
Firstly, there is the question of what the site does. For a clinician, this sort of calculation is an everyday occurrence. In one of our focus groups, however, a woman (who had not had breast cancer) described how she could imagine sitting down at this site called ‘Predict’ and being faced with something that was going to tell her her future: how entering her details and then being expected to click a button to discover her likely fate would have her shaking and probably in tears. Clearly the design, the language used and the information surrounding the tool about what it will (and won’t) do is vital. It’s not simply a matter of avoiding or explaining technical terms, or even of making the numbers that come out of it clearer through graphics.
What does prediction mean?
Reading online forums, it’s clear that many patients do enter their details into the current version of Predict, alongside other similar risk prediction sites designed for clinicians, and are then upset and confused by the different outcomes they get from each. Some talk of having ‘favourite’ risk prediction tools, which give them more favourable outcome predictions—without realising that there’s a reason for the difference. The sites giving apparently ‘better’ outcome proportions are simply giving disease-only mortality figures rather than all-cause mortality. If you are an older woman, your base chance of mortality—regardless of disease—can be significant. No wonder it ‘sounds better’ on sites that don’t mention that. But these sorts of perspectives—which you can read in forums but also arise out of our focus group work to understand the needs of patients—raise a whole host of interesting issues around our work. Most of us, as patients, want reassurance in the face of scarily uncertain futures, and facing our inevitable mortality is not something we choose to do. On top of that, dealing with probabilities does not come naturally to most of us. For an individual, an outcome is usually all or nothing—either my cancer will recur or it won’t: there’s no ‘70%’ about it. In focus groups and on forums we hear the sentiment: “knowing the statistics won’t affect the outcome for me”—except that it does when knowing the statistics helps you choose a treatment option that gives you a better chance of the outcome that you would value the most. Helping patients to recognise this—to give them a sense of empowerment rather than fear in this unfamiliar world of probabilities is a key task that we need to tackle, and help doctors deal with too.
You might also like: Radiation Dose: Communicating With Patients
What matters to you?
Patients should also have more power than simply understanding which treatment gives them the best chance of surviving longest. Clinicians, by default, are obliged to maximise their patients’ lifespan, but we all have different priorities—and often with life, quality can be more important than quantity. One thing that has come up often when talking to both doctors and patients is the need to be able to discuss things like side effects and the risks of decreased quality of life associated with different treatment options. Helping collate and provide the figures around the risks and benefits of treatment options in terms of mortality is hard enough—adding in the side effects, which are not so well recorded, is even harder. Listening to patients, though, it’s clearly important to them and so it’s something that we aim to do.
Providing clinicians and patients with risk and benefit information, tailored to the individual patient as much as possible, and in a clear and friendly format, will hopefully allow a much greater level of shared decision making. When we ask in our patient focus groups whether people would like to take an active role in
deciding between treatment options, the overwhelming response is yes: of course they want guidance from a trusted clinician, but they want to feel in charge of the final decision: patients express sentiments such as “it’s my body” and “I have to live with the consequences.” This is reinforced by data on patient satisfaction when they have used decision aids to help them discuss the options with their doctor. These types of tool, then, should have a growing role in healthcare in the future.
Information for every decision
The NHS Predict site is designed specifically for decisions around adjuvant treatment in breast cancer, but we are planning to use it as a proof of principle for a whole range of other applications as well. Our next adaptation of it is planned to be for transplant patients, who have to make agonising decisions. With donor organs in such short supply, and increasing techniques to make use of ‘imperfect’ organs, transplant patients are now more than ever being put in the position of choosing between accepting a donor organ which may carry higher risk to them, or remaining on the waiting list in the hope of a ‘better’ organ. In this scenario, it is vital that they know the risks of each— mortality whilst on a waiting list is painfully high for some patients, something which is a difficult fact to face, and so is at the heart of a very sensitive conversation between patient and surgeon. We very much hope that a carefully designed and personalised site can help that conversation take place.
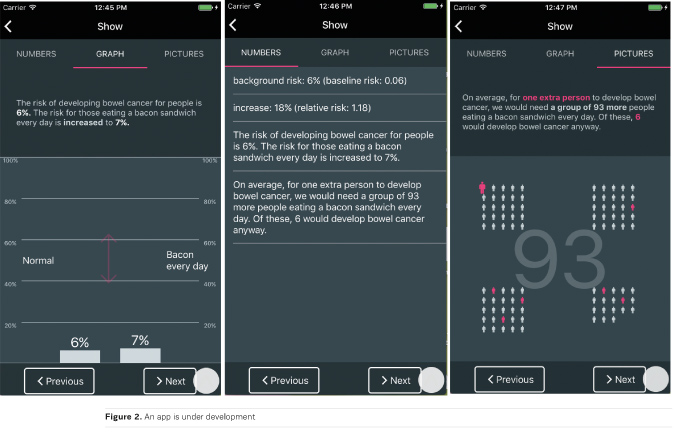
Not every health decision, though, is so sharply life and death. From popping a painkiller to taking a screening test, we all face minor decisions every day— and yet most of us make them without knowing the facts. Here too we aim to help. Many years of research have been put into developing simple tables and infographics to display the potential benefits and harms of any health decision ‘at a glance’. Now, these are becoming accepted as an important addition to patient information in leaflets and on websites, and we are developing a free app that can display such information handily on mobile devices, allowing clinicians and patients to have it at their fingertips (Figure 2). There is a hint that patients who are more informed might tend to choose less medical treatment (Arterburn et a l. 2012)—as well as b eing h appier in t he outcome (Stacey et al. 2017)—and if that turns out to be true, it is a great incentive in a world where there is increasing pressure for medicalisation and stress on health services. If an informed patient is a happier patient, a less medicalised patient, and the patient of a doctor under less stress then truly the future of healthcare is a future in which information — not medication — is king.
The Winton Centre for Risk & Evidence Communication was founded at the University of Cambridge at the end of 2016. Its motto is ‘to inform but not persuade’ and it aims to help present and communicate quantitative evidence to decision-makers in a whole range of fields, from healthcare to the legal profession.
References:
Arterburn D, Wellman R, Westbrook E et al. (2012) Introducing decision aids at Group Health was linked to sharply lower hip and knee surgery rates and costs. Health Aff (Millwood), 31(9): 2094-104.
Diemert DJ, Lobato L, Styczynski A et al. (2017) A comparison of the quality of informed consent for clinical trials of an experimental hookworm vaccine conducted in developed and developing countries. PLoS Negl Trop Dis, 11(1): e0005327.
Hoffmann TC, Del Mar C (2015) Patients’ expectations of the benefits and harms of treatments, screening,
and tests. JAMA Intern Med, 175(2): 274–86.
Hoffmann TC, Del Mar C (2017) Clinicians’ expectations of the benefits and harms of treatments, screening, and tests. JAMA Internal Medicine, 177(3): 407–19.
Stacey D, Légaré F, Lewis K et al.(2017) Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev, (4): CD001431



