Reducing management complexity in patient care.
Research shows how to optimise and streamline care in the hospital setting by separating patients into routine and complex groups.
After years of medical progress, we are now facing the age of precision medicine in which new technologies allow for effective care tailored to the individual patient. Yet, why are the current business models in healthcare subject to inertia and still rely on intuitive medicine? Consider the general hospital for example, which has ever since been providing all kinds of services for all kinds of patients. Its clinical departments, which are predominantly organised along medical specialties, deliver routine as well as non-routine care. Routine and non-routine care, however, encompass substantial differences in the diagnosis and treatment trajectories and therefore require completely different organisational structure and processes. They cannot be blended adequately and their coexistence poses a complex managerial challenge. Standardised routine services are provided in a resource-intense environment and are thus deploying resources, which are essential for the varying requirements of non-routine services (Christensen et al. 2009).
While redesigning the hospital landscape is a hot topic in the public debate, concrete and appropriate redesign suggestions seem to be lacking. Within the scientific community, however, concrete approaches are already discussed and one idea entails separating routine from non-routine care in general hospitals. Our recent paper “Separate & concentrate: accounting for patient complexity in general hospitals” (Management Science, forthcoming) supports that claim. Using data of more than 250,000 patients in 60 German hospitals, we analysed how quality of care is affected by operational factors. For 39 disease segments, we considered how disease-specific hospital volume (ie the number of patients), disease-specific hospital focus (ie the number of patients as a proportion of all patients), and disease-specific degree of concentration (ie the proportion of patients admitted to the disease-specific default department) are related to the mortality rates within seven days following hospital admission. Our empirical results show that the effects differ depending on the patient’s degree of complexity. We classify patient complexity based upon their emergency status and their co-morbidity level or categorise the extremes as either routine patients or complex patients. Routine patients are, by definition, never admitted as an emergency and do not suffer from more than two comorbidities. Complex patients, on the contrary, are admitted as an emergency and have a high co-morbidity burden, ie at least three comorbidities.
While the disease-specific hospital volume seems to be irrelevant for routine patients, it turns out to be detrimental for complex patients; higher volumes relate to higher mortality rates. These results appear quite surprising given the vast number of health economic and medical studies indicating quality gains due to increased volume. How can these reverse results be explained? In contrast to other studies, our study also incorporates the hospital’s focus, which is also referred to as the hospital’s level of specialisation. Specialisation is not only a highly important determinant for quality but also a factor that is quite often strongly connected to the hospital’s volume –a highly specialised hospital does frequently also provide care for a high number of patients.
Whereas volume does not affect routine patients, our results show that the aforementioned level of hospital focus is crucial. If a routine patient is treated in hospital with specialisation in the patient’s disease segment on the one hand and not too many admissions of patients with different diseases on the other hand, the routine patient experiences a substantial quality gain. Incorporating the findings on the hospital’s volume, we can conclude that if routine patients are separated and receive care in a specialised organisation, it would be not only beneficial for routine patients themselves, but also indirectly for complex patients considering that the overall disease-volume will be reduced through the separation.
Moreover, our results show that complex patients benefit from a high degree of concentration within the hospital. To determine the disease-segment’s degree of concentration, we consider how patients are routed to and distributed over clinical departments. For example, if 80 percent of the patients within one disease segment are admitted to the same clinical department, it indicates a high level of concentration. If patients of one disease-segment are, by contrast, admitted to four clinical departments in equal shares, the level of concentration is rather low. Our results imply that if hospitals have a disease-specific routing strategy and patients are predominantly admitted to the same clinical department rather than distributed over multiple departments, complex patients experience substantial quality gains.
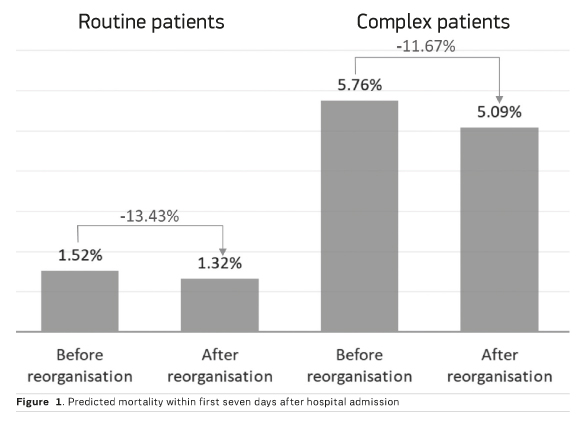
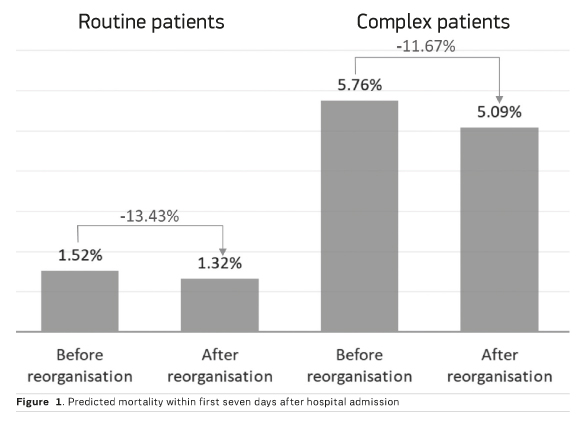
Taken together, the empirical results support the claim that reducing the managerial complexity of general hospitals can be achieved via two steps: separate and concentrate. Within the first step, we suggest separating routine care from non-routine care, with routine care consecutively being provided in separate clinics or organisationally distinct facilities. Using our empirical results, we can simulate that such a separation could lead to a 13.43 percent reduction in mortality rates for routine patients. If we then proceed with the second step and increase the level of concentration within the clinical departments, we could reduce the mortality rates of complex patients substantially. If hospitals have admission policies and routing strategies in place that allow them to achieve disease-specific concentration levels of 60 percent, mortality rates of complex patients could drop by 11.67 percent. This is illustrated in Figure 1, which shows the expected results of such a reorganisation attempt. Obviously, such a redesign goes along with a variety of implementation challenges that are not captured in our simplified counterfactual simulation. Yet our analysis should demonstrate the potential clinical effect size if general hospitals change their business model towards the separate and concentrate design. Now it’s up to the scientific community and health policy makers to refine the approach.
In a nutshell, we can therefore state that if general hospitals engage in the “continue-as-it-is” vein, we do not end up with the optimal quality of care for any patient. Routine patients have to be separated consistently and their care has to be organised in dedicated organisational units. The remaining complex patients should be allocated consistently to clinical departments that are equipped with the required interdisciplinary resources.
Key Points
- New technologies are allowing for precision medicine to tailor care yet present-day general hospital business models rely on intuitive medicine
- The co-existence of routine and non-routine care encompasses substantial differences presenting critical managerial challenges.
- Quality of care for routine and complex patients is impacted by operational factors
- A reduction in managerial complexity of general hospitals is achievable through two steps: separate and concentrate
Christensen CM, Grossmann JH, Hwang J (2009) The innovator's prescription: a disruptive solution for health care. New York: McGraw Hill.