HealthManagement, Volume 16 - Issue 3, 2016
INCREASE COMMITMENT BY TEAM INVOLVEMENT
In Europe, departments of radiology and nuclear medicine are typically independent centralised organisations with different cultures and values. Some imaging departments are being developed that integrate existing radiology and nuclear medicine departments. When planning integration, a key success factor is the relationship between the respective leaders and alignment on a strategy towards excellence.
When our hospital moved to a new location, five radiology and nuclear medicine departments were merged into an integrated imaging organisation employing more than 380 personnel. The original structure and teams (with their specific cultures, technical orientation, high degree of independence for professionals, modest research activity, and barely any care process integration) were restructured. This required a strategy update because of the new clinical orientation, organisation, facilities and equipment.
Our aim is to describe the process of fostering organisational change for a unified medical imaging department, through active staff involvement and shared ownership. The impact of the change process on organisational culture was evaluated by survey measurements before and after the initial strategy refinement and deployment workshop.
Materials and Methods
Initial Discussion
Two basic prerequisites were identified during the initial dialogue:
- A core team to guide the work on
process improvement, standardisation and integrated patient management;
- Creation of teamwork between
staff members, to establish a common understanding and shared ownership about
the goals of the new department.
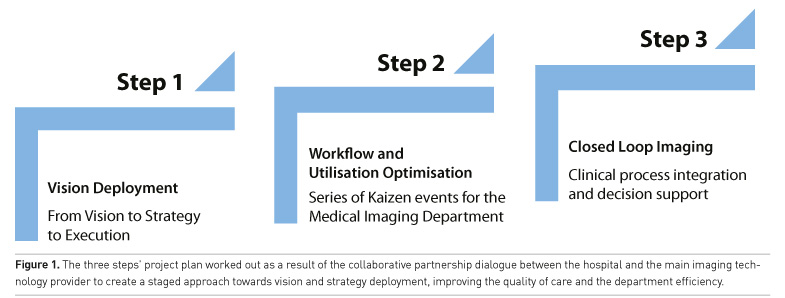
The programme plan for this collaborative partnership included a three-step approach (Figure 1):
- Step 1 (main topic for this paper) focuses on vision and strategy
definition and deployment, shaping the conditions for cultural change via a
team coaching approach.
- Step 2 involves a series of Kaizen events aiming to optimise
specific clinical workflow processes and to establish a continuous improvement
mindset (Colenso 2000). Kaizen events are rapid workflow improvement projects
through intensive teamwork based on the Lean and Six Sigma quality improvement
principles.
- Step 3 comprises a “closed loop imaging” project to facilitate the
implementation of a dashboard clinical decision support system based on
relevant clinical processes.
Team Coaching Approach
The process started with deep analysis of the existing strategy document prepared by the department director, followed by team activities to refine the vision and strategy articulation.
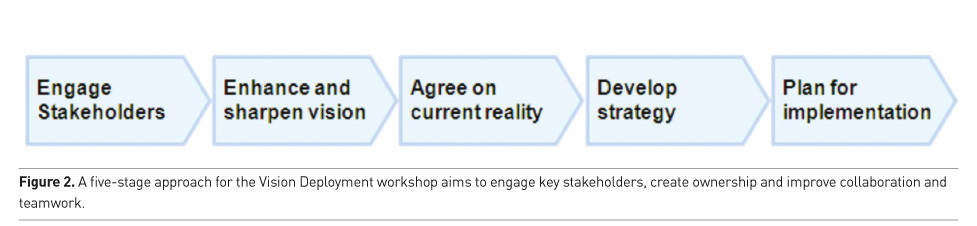
A series of team workshops was organised to create a common sense of direction. The team coaching encompassed a five stages approach (Figure 2), aiming to engage key stakeholders to work together as one team through the vision and strategy refinement and deployment processes (Erasmus Medical Center; Integrated Service Improvement Programme).
The core team involved in this coaching initiative had a balanced representation of members of the imaging department (28 participants, including 11 radiologists, 5 nurses, 3 radiographers, 3 administrative employees, 2 nuclear medicine physicians, 1 cardiologist, 1 paediatrician, 1 resident in-training, and 1 transporter). Participants were selected based on personal attitude and aptitude, job category, experience and gender balance. Suggestions were also obtained from other individual department coworkers from all job categories.
Model Towards Action Planning
A model by Mintzberg (Mindtools n.d.) was applied as a processoriented approach. This model shows all relevant influences in a process way, starting with a mission and vision statement, followed by an exploration through internal and external analyses connected via a strengths-weaknesses-opportunities- threats (SWOT ) evaluation (Wikipedia). Scenario and strategy discussions support the prioritisation process, finally leading to an action plan for organisation-wide deployment.
Internal analysis of organisation culture was performed with the Organizational Culture Assessment Instrument (OCAI ) (OCAI Online) (Figure 3). External analysis was achieved by studying vision and strategy documents published by other major European academic hospitals. SWOT and Gap analyses (Mindtools n.d.) were constructed and evaluated during the workshops to identify differences between the present state and desired state of the company culture.
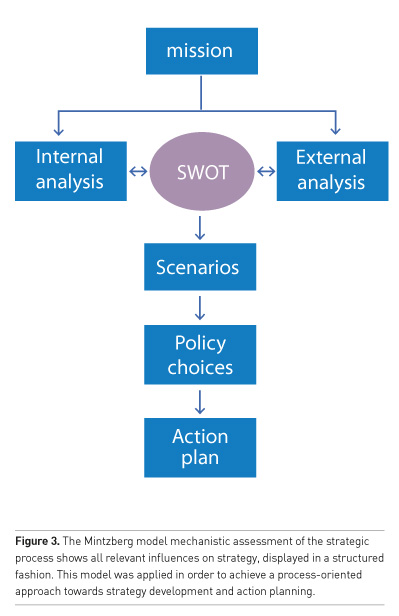
A workshop was conducted based on the existing vision and strategy document, the results of the initial survey on OCAI and a series of individual interviews with all 28 participants. Four agreed clinical pathways were utilised as pilots (paediatric, fast track, oncology and emergency). Workshop results, issues and opportunities were translated into an action plan.
Stakeholder Engagement
The OCAI survey provided an indication of the perceived present situation of the organisation’s culture in comparison to the perceived desired situation. The survey results were discussed in a deep dive session during the two workshop days. The OCAI survey suggested that “ad-hocracy” was the dominant influence in the present situation, characterised by a dynamic and creative working environment where leaders are seen as innovators and risk takers, promoting individual initiative and freedom (Dolan 2010). For the desired situation, the survey showed a dominant influence for a “family or clan culture”, suggesting a preference for a friendly and close community environment, leaders being seen as mentors.
Enhance and Sharpen Vision
All 28 participants were encouraged to picture a desired future state for the organisation (dream your future) as well as to describe the current situation (agree on reality), in order to identify gaps between the current and future state to understand where action is needed.
The team identified a series of opportunities, the most relevant being:
- State-of-the-art technology
provided huge medical, clinical and research opportunities.
- People would recommend the new hospital
to relatives and friends as a good place to work, behaving as real promoters
of their workplace.
- There was a very enthusiastic
team ready to work together to create opportunities.
- The new department improves
clinical innovation, attracts more and better residents, and expands synergies
between other clinical departments.
The team also mentioned a number of concerns, of which the most relevant were:
- The reasons to create a single
imaging department when employees keep working in small groups were unclear.
The team feeling of being one single department was weak.
- Effective collaboration within
the team and knowledge management was a concern. Central coordination, management
meetings, key performance indicators and communication were not clearly
defined.
- The style of competition was seen
as a threat.
- The faculty concern was about moving away from their professional clinical work because of administrative tasks and management issues.
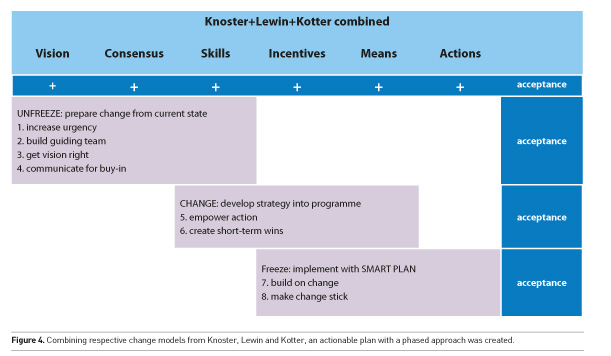
Interviews were clustered and mapped on the prerequisites for successful change of the Knoster model (Knoster 1991). Knoster distinguishes 6 organisational prerequisites for a successful approach to change (Figure 4). The model shows the relationship between successful change and a variety of conditional elements such as Vision and strategy, Consensus on the strategy, Skills to execute it, Incentives to make it worthwhile (what’s in it for me), the Means to help execute it, and finally a clear Action plan to deploy the strategy. All conditions are critical to a successful change process; all prerequisites must be in place; and all identified actions have to be accomplished along the journey.
Agree on Current Reality
The organisers inspired participants to draw the image of an ideal service organisation around four selected care pathways: paediatric, fast track (stroke, heart failure or bowel attack), oncology and emergency. Facilitators explicitly asked the participants to assume the role of a patient, which helped to identify many patient-focused improvement opportunities. The current situation was evaluated with cause-effect analysis (Ishikawa diagram), SWOT analysis and Gap analysis. Communication is crucial within a large imaging department, and therefore it was recognised as essential to have an effective communication tool for procedure planning and execution.
Developing Strategies and Action Plans
Final sessions were dedicated to developing action plans. Several quick win opportunities were identified to support internal processes to identify areas for process improvements. A Kaizen approach (Colenson 200) was considered effective to perform detailed analysis and achieve process improvement for specific modality workflow and/or specific patient/ clinical pathways. Combining respective change models by Knoster (Colenson 2000; Mindtools n.d.) enabled creation of an actionable plan with a phased approach (Figure 4).
Our combined model shows the relationship between successful change and a variety of the conditional elements identified by Knoster (Vision, Consensus, Skills, Incentives, Means and Actions). Lewin (Mindtools n.d.) divides a change process into three consecutive time phases; each phase requiring focus on specific prerequisites of the Knoster model. Kotter (Mindtools n.d.) proposed an 8-step actionable approach to leading change (create urgency, form a powerful coalition, create a vision for change, communicate the vision, remove obstacles, create short-term wins, build on the change, and anchor the changes in corporate culture). All these steps were mapped on the three phases distinguished by Lewin.
Lewin and the 8-step approach introduced by Kotter have structured the action plan according to the three phases distinguished in our adapted model. Knoster shows which elements need to be in place as prerequisites for a successful change process, indicating that more is needed for successful change than just vision and strategy. The ultimate goal was to find ways to fill the gaps identified by the Knoster analysis.
Results
According to the developed steps and following the combined Knoster+Lewin+Kotter modified model, the following 8 recommendations were constructed (Figure 4).
Step 1: Develop a sense of urgency around the need for change and inspire people to move, making objectives real and relevant. The suggested actions were:
- Identify potential threats and
develop scenarios showing what could happen in the future.
- Examine opportunities that should
or could be exploited, collect facts and develop arguments for strategic workshops.
- Start honest discussions and give
dynamic and convincing reasons to get people talking and thinking within the management
team and young talented individuals.
- Request support from “customers”,
apart from stakeholders and industry people, to strengthen the department argument.
Step 2: Get the right people in place with the right emotional commitment, and with the right mix of skills and levels. The following actions were suggested:
- Identify the true leaders in the
organisation and incorporate talented, powerful, change promoter young
individuals to construct an extended management team.
- Ask for an emotional commitment
from these key people.
- Check for weak team areas,
ensuring a good mix of people from different areas and with different levels
within the department.
Step 3: Get the team to establish a simple vision and strategy and focus on the emotional and creative aspects necessary to drive service and efficiency. Here, the suggested actions were:
- Determine the values that are
central to the change.
- Develop a short summary,
capturing what is "seen" as the future organisation, sharpening the
existent department strategic document.
- Create a strategy to execute that
vision, developing scenarios during a vision workshop.
- Ensure that the new coalition can
briefly describe the vision.
Step 4: Involve as many people as possible, communicate the essentials, simply, and appeal and respond to the people's needs. The following actions were suggested:
- Speak frequently about the change
vision and further develop the communication plan.
- Openly and honestly address
peoples' concerns and anxieties, including “soapbox” sessions.
- Apply the vision to all aspects
of operations, from training to performance reviews, by establishing success
factors and performance indicators linked to objectives.
- Lead by example with actions such as “walk the talk” (manage by walking around, be present on the work floor and give a good example to motivate people).
Step 5: Remove obstacles, enable constructive feedback and lots of support from leaders - reward and recognize progress and achievements. The suggested actions included:
- Identify leaders whose main roles
are to deliver the change, investigate midterm opportunities and assign quick
win project to core team members.
- Check the organisational
structure, job descriptions, performance and compensation systems to ensure
they are in line with management vision.
- Recognise and reward people for
making change happen, communicate about best practices.
- Identify people who are resisting
the change, and help them see what is needed.
- Take action to quickly remove
barriers, human or otherwise.
Step 6: Nothing motivates more than success. There is a need to set aims that may be easy to achieve and within a short timeframe. Some suggested actions were:
- Implement easy surefire projects,
such as Kaizen events for specific issues that address impacts and objections early,
for example patient routing and examination planning.
- Avoid early targets that are
expensive and whose investment cannot be justified in each project.
- Reward people who help you meet
targets by celebrating their successes.
Step 7: Many change projects fail because victory is declared too early. Real change runs deep. Quick wins are only the beginning of what needs to be done to achieve long-term change. The team identified and proposed the following actions:
- After every win, analyse what went right and what needs to be improved. Define SMART goals (Specific,
- Measurable, Attainable, Relevant
and Time-bound) to make improvement measurable.
- Set goals to continue building on
the momentum that the team achieved.
- Make sure that people are well
trained in the idea of continuous improvement.
- Enable people to experience the
benefits of the changes.
Step 8: To make any change stick should become part of the core of the organisation. The corporate culture often determines what gets done, so the values behind the vision must be shown in day-to-day work. The following final actions were suggested:
- Establish a track record of
success! Celebrate success! Involve everyone and publicly recognise key
members! Talk about progress every chance you get!
- Create plans to replace key
leaders of change as they move on to ensure that their legacy is not lost or
forgotten.
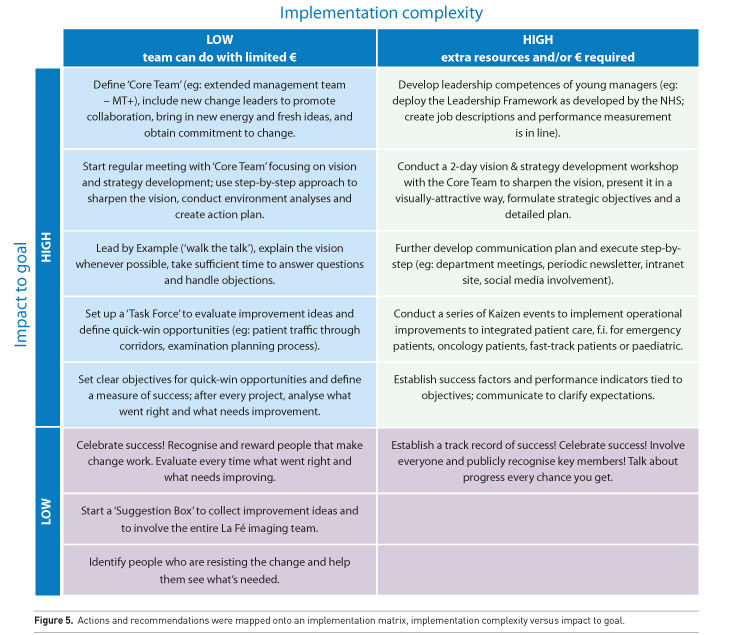
- These recommendations were
translated into tangible actions, which were mapped onto an implementation 2x2
matrix, implementation complexity versus impact to goal (Figure 5).
Success Measurements
Different measurements were obtained to measure the result of the change management process in the organisational culture. One year after the workshop, the OCAI survey was repeated among the team members of the Vision Deployment workshop. The analysis performed before and after the change process showed that the perceived adhocracy was taken over by hierarchy as the perceived dominant organisation culture. This indicates that the imaging organisation became a much more structured work environment.
An external 5-point scaled survey (1 to 5, 5 being extremely good) was sent to all medical staff and medical residents of the hospital, outside the imaging department, to evaluate different aspects related to the organisation. There were 168 complete answers before (2012) and after (2013) the change management initiative. Analysis showed an overall improvement in our organisation regarding assessment of the new clinically-oriented department (3.56±0.97 versus 3.61±0.94, mean±SD , before and after the change process respectively); ability of imaging specialists to solve clinical problems (3.97±0.90 versus 4.00±0.90); availability and quality of imaging results and reports (3.69±0.90 versus 3.81±0.95); departmental collaboration in educational and research programmes (3.59±0.89 versus 3.66±0.88); and participation of imaging specialists in clinical guidelines and appropriateness criteria proposals (3.53±0.98 versus 3.57±0.96). The only slightly negative trend was observed in the accessibility of imaging specialists for clinical consultancy (3.87±0.98 versus 3.87±1.04).
The organisation kept working on the implementation of the three step global approach (Figure 1), and started to focus on further process improvements. Kaizen events were implemented to optimise specific clinical workflow processes and to initiate a continuous improvement work attitude (Colenson 2000).
Discussion
The process of fostering major organisational changes in a large European university hospital is a challenging task. Many departments are evaluating merging with related ones (such as radiology and nuclear medicine within the same hospital or linked large areas) to improve operational efficiency, eliminate waste and optimise the value of their services (Kruskal et al. 2012). Critical success factors are a clear direction (ie consolidated strategy), process analysis and intensive involvement of the clinical staff in the deployment of this strategy (Kruskal et al. 2012; Thomson et al. 2016).
The five-day Vision Deployment workshop was instrumental to engage a representative core team of key opinion leaders from all levels of the organisation. Individual interviews gave the team ample opportunities to share their ideas and concerns, while the right level of trust and buy in was created for the workshop. Although team size (28 participants) and constitution (most participants were unfamiliar with concepts of strategy development) made it challenging to achieve the objective of strategy refinement, many good ideas were generated as a starting point for process improvements in our imaging department. These practical elements have all been captured in a midterm action plan that will be implemented via several rapid process improvement activities (Kaizen events).
The combination of proven change models (Knoster, Lewin and Kotter) allowed the development of a phased plan with clear recommendations, actions and ownership. The core team was able to initiate several key actions, important aspects for the future success of the new department. We showed it was possible to bridge the gap between management and staff and align their visions, by carefully integrating all stakeholder opinions and visions. We created active involvement of staff in the strategy refinement and deployment process, and obtained their increased commitment in return. All the workshop activities logically led to an increase in contact and communication between staff that previously had little contact, yielding much improved understanding and appreciation for each other. Finally an action plan was developed that will guide further midterm improvements.
The outcome of our organisational change process was an effective alignment between management and staff views, and this yielded renewed commitment to an ambitious but realistic plan to implement the necessary changes. The new department really had to go through this change facilitation program to create sufficient awareness and commitment to start working on important integrated care initiatives, as well as patient experience and process improvement initiatives.
Acknowledgements
The corresponding author’s department and hospital has a Master Research Agreement with Philips Research. Part of this work was done within this grant. Ené Regos was working for Philips Healthcare Transformation Services in Spain, currently working for Philips HealthTech LATA M as Customer Service Sales and Business Manager for Hispanic countries. André van Est works for Care IQ Group BV, an SME located at The Netherlands.
Key Points
- Encourage organisational change
process by developing an integrated imaging department is needed in the
academic professional organisation.
- Industry change management
practices (Mintzberg management of change with Knoster, Lewin and Kotter models)
can be adapted.
- An effective alignment between
management view (desired state perspective) and staff view (present state
perception) can be successfully implemented





