HealthManagement, Volume 17 - Issue 5, 2017
Food waste at hospitals can be recognised and addressed
An Irish healthcare sustainability programme aims to increase the catering efficiency of hospitals with steps to reduce waste.
Non-profit organisation, Health Care Without Harm Europe (HCWH Europe), brings the voice of healthcare professionals to the European policy debate about key issues including sustainability. In order to support work on sustainable food in healthcare, they have organised international workshops and produced a report on sustainable food in European healthcare as a result of a survey with European hospitals. Eileen O'Leary from the Cork Institute of Technology has contributed to HCWH Europe's work in this area and spoke to HealthManagement.org about the challenges and best practices in sustainable food in healthcare.
How does healthcare define food waste?
Under the Irish Green Healthcare programme, which we run on behalf of and is co-funded by the National Health Sustainability Office (NHSO ) within the Health Service Executive (HSE ) and by the Environmental Protection Agency (EPA ), we have performed a large number of food waste surveys in both acute and nonacute healthcare facilities.
The HSE is Ireland’s national public health service. Green Healthcare’s focus is on ef ficiencies and savings in relation to water and waste in Irish healthcare facilities.
To perform these food waste surveys we have taken the definition of ‘waste’ in general under EU law, i.e. something is a waste if it is discarded/to be discarded, a nd a pplied t his to food arising in a catering scenario. Thus, when we are performing food waste surveys, any food that is ‘discarded or to be discarded’ we have taken as food waste. Thus, it will encompass all biowaste/food arising from food preparation, cooking, serving, clearing plates after patients/ staff have finished eating, wash-up after service, as well as anything discarded from storage. In order to help identify options for improvement, we further break down food waste into different categories as follows:
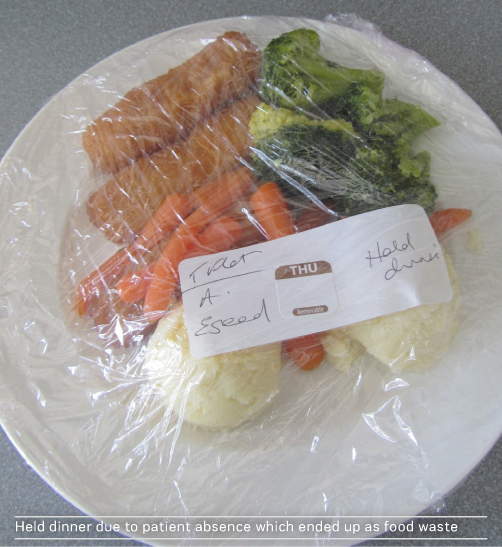
- Unserved food waste. This is edible food that is left over
in bulk service containers, bain maries, kitchen pots, etc. after service, that
is subsequently discarded (any food that is retained and stored for future use
is not counted). For centrally-plated systems, it may also include untouched
plates of food that were never served. It may also include items that are out
of date discarded directly from storage (we have found the latter to be
relatively very small as a source of food waste; there are usually good stock
rotation systems in place).
- Plate waste. This is edible food remaining on plates, bowls,
etc. after patients/staff have finished eating.
- Preparation waste. This is food waste that arises in preparing
and cooking of food. This may or may not be edible. It is often unavoidable. It
includes things like vegetable peelings, salad off-cuts, meat/fish skin/bones,
bread heels, tea-bags, coffee grounds, and so on.
Putting a focus on the first two of the above areas (unserved food and plate waste) in terms of the quantities arising, food types, and sources within the facility can help identify actions to reduce food waste amounts.
What needs to change in terms of seeing food as integral to a patient’s treatment?
It needs to be led from top management within a healthcare organisation. Systems like protected meal times, if in place, need to be respected by medical staff and properly enforced.
International best practice examples, showcasing healthcare organisations that place food and nutrition central to patient care, could help.
In the longer term, it needs to be ensured that it is addressed within the education system for all medical personnel.



In terms of financial wastage, what sort of figures are we talking about when it comes to hospital food waste?
It is often the cost of a brown bin waste service that people tend to focus on. However, the associated cost of food waste in terms of lost food purchases always dwarves the size of the bin service costs. The Green Healthcare programme performed a detailed food and food waste cost assessment at an acute hospital in Dublin. This covered the three weeks of the hospital’s menu cycle. It quantified the total amount of food purchased for the three weeks, and performed a stock take at the beginning and end of the three weeks. This provided the total amount of food used in terms of Euros and kgs.
This survey showed an average cost of food per kg of €2.29/kg. Based on an associated food waste survey, it was found the average cost of edible food waste (unserved food and plate waste) per kg was €2.05/kg. The difference is down to cheaper foodstuffs taking up a larger percentage of the waste, i.e. meat and fish are more likely to be better portioned. Similarly, surveys in the hospitals have shown that, on average, 70% of food in food waste bins is edible food which was meant to be eaten (unserved food and plate waste). The remainder 30% was food with no value (preparation waste).
Thus, each full 240-litre brown bin represents about €170 in lost food purchases, while it usually is only about €10 per bin in waste handling charges. An alternative way to look at these numbers is that 1000 kg or 1 tonne of food waste arising in the brown bins for a hospital represents over €1,400 in lost purchases. This allows a hospital with the total annual tonnes of food waste available to it from its waste contractor to put a cost of food purchases lost as food waste each year.
There are several hospitals in Europe that are implementing best practices and innovations in food management and succeeding in reducing food waste. In your view/s which are some of the most successful and why?
The Green Healthcare programme has a number of case studies on Irish hospitals that have taken steps to reduce their food waste. One of the best performers surveyed was Mayo General Hospital. Another hospital that has made improvements is St Michael's Hospital, Dún Laoghaire. I think success is in many cases down to the staff involved.
From your experience of focusing on best practice in food management, is it possible for a hospital to start taking simple steps to see immediate reductions in food wastage?
Most definitely. The best first step to take is to start observing food waste amounts arising at the different points around the hospital (wards, main kitchen) and at different meals. Often due to the layout of the hospital, the food waste generated at the wards is never seen by the main kitchen. Even if a hospital starts only observing and not weighing food waste, it may help inform what could be done. Often, the limiting factor in implementing changes can be staff time. A catering department c an use the waste data and its associated purchasing costs to make the financial case to management to seek the provision of some additional staff time to help implement changes, where needed (e.g. through better coordination of ordering from the wards).
Irish healthcare facilities, and commercial facilities in general in Ireland, are fortunate in one respect in that it has been mandatory by law since 2009 to segregate food waste for collection, in order for it to be sent for composting or anaerobic digestion. Thus, the amounts of food being wasted are much more visible, compared to food waste being handled via a mixed waste collection or a macerator to sewer. In addition, data on total tonnages of food waste can be obtained since such waste is weighed by the waste contractors.
I’d like to add that, as well as tracking total food waste amounts, it can be useful for a hospital to benchmark itself against its peers, as well as against itself year on year. The Green Healthcare programme has produced an average benchmark for all wastes for acute and smaller community hospitals, and for food waste too, which is based on a kg per patient bed day basis. For acute hospitals we have found an average of 0.73 kg of food waste per bed day, while best practice was 0.45 kg of food waste per bed day.
As part of the food waste surveys carried out, the Green Healthcare programme has also measured the total weight of food prepared. Thus, it has been able to determine that on average 51% of the food prepared is eaten by patients, with 27% being unserved food waste and 22% ending up as plate waste.
Key Points
- 1 tonne of food waste arising in the brown bins for a
hospital represents over €1,400 in lost purchases
- Under EU law, something is a waste if it is discarded/ to be
discarded
- To identify options for improvement, food waste is broken
down into Unserved Food Waste, Plate Waste and Preparation Waste
- Regarding food as part of patient treatment needs to be led
from top management
- Protected meal times need to be respected by medical staff
and properly enforced
- Lost food purchases always dwarves the size of the brown bin
waste service costs
- To improve, start observing food waste amounts arising at
the different points around the hospital and benchmark against its peers and
itself
Reducing Waste
As recommended by Eileen O’ Leary, a Best Practice Guide on food waste reduction in healthcare as well as guidance on how to undertake a food waste survey in a healthcare facility is available at: greenhealthcare.ie/wp-content/uploads/2014/05/Best-Practice-Food-Waste-revised.pdf




