HealthManagement, Volume 17 - Issue 1, 2017
Introduction
Meetbaar Beter (En: Measurably Better) is a doctor-driven and patient-focused initiative with strong scientific roots that aims to improve the transparency and quality of cardiovascular care in the Netherlands.
Meetbaar Beter has become an international best practice in the implementation of value-based healthcare (VBHC). The project started as an initiative of two hospitals, and by now 19 heart centres participate, covering over 85 percent of complex heart care in the Netherlands. In 2016, outcomes that matter most to patients have been published for over 150,000 patients, including the treatment of high prevalence medical conditions like coronary artery disease, aortic valve disease, atrial fibrillation and mitral valve disease.
Limited sets of outcome measures per medical condition, selected by doctors (cardiologists and cardiothoracic surgeons) and validated by international experts, form the basis for the open learning and development culture of Meetbaar Beter. Doctors gain insight in outcomes and use this information to cooperate and continuously improve the quality of care for heart patients (Van Veghel et al. 2016). In this article we share the approach that has led to the success of Meetbaar Beter.
The Goal of Meetbaar Beter
Meetbaar Beter’s aim is to facilitate quality improvement for patients with heart diseases in the Netherlands. Its focus is on health outcomes that matter most to patients. The hypothesis, based on Porter’s VBHC (Porter 2010), is that improvement of outcomes will lead to a reduction of costs. Measuring costs will be included in Meetbaar Beter, in a later phase.
Transparency of outcomes is an intermediate but important goal as it helps build high levels of trust between heart centres and stakeholders such as patient organisations, health insurance companies and government organisations. Transparency is considered a sine qua non in being able to identify best practices. Study results support the importance of transparency and its strong relation with quality (Larsson et al. 2012).
Leading Principles
Meetbaar Beter has a few leading principles. Firstly, it is doctor-driven. Doctors and their teams regularly create changes in healthcare. In Meetbaar Beter, the board of directors, advisory board and outcome team typically consist of doctors making lead decisions. Strong connections have also been built with Dutch societies of cardiologists and cardiothoracic surgeons.
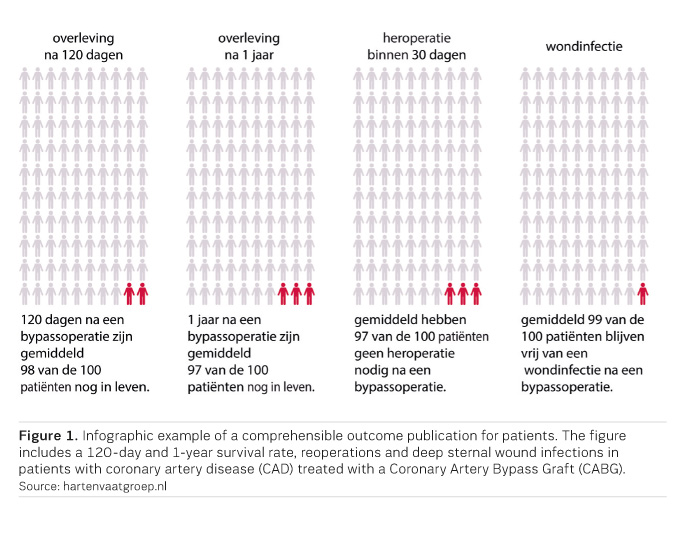
Secondly, Meetbaar Beter is patient-centred. The organisation and improvement work is structured around medical conditions. Outcomes are measured for medical conditions both independent and dependent of the chosen treatment. The selection of outcome measures is validated by large patient groups and outcomes are published in a comprehensible manner for patients. For instance, infographics have been developed (Figure 1).
 Thirdly, transparency is a leading principle. In
Meetbaar Beter, strict data quality and data completeness criteria are used.
When the data quality of a hospital fulfils the minimum quality criteria, data
is published independent of the results. This has proven to be a strong
stimulation for heart centres in improving the quality of data. Already in the
very early stage of Meetbaar Beter, the publication of data led to hypotheses for
quality improvement. Lessons have been learned quickly by heart centres in
organising outcomes-based quality improvements.
Thirdly, transparency is a leading principle. In
Meetbaar Beter, strict data quality and data completeness criteria are used.
When the data quality of a hospital fulfils the minimum quality criteria, data
is published independent of the results. This has proven to be a strong
stimulation for heart centres in improving the quality of data. Already in the
very early stage of Meetbaar Beter, the publication of data led to hypotheses for
quality improvement. Lessons have been learned quickly by heart centres in
organising outcomes-based quality improvements.
Finally, Meetbaar Beter focuses on outcome measures. Outcome measures are considered leading with respect to process and structure measures. Outcomes are influenced by the initial conditions of patients and the quality of care delivery. For an insight in quality of care, in several analyses, outcomes are corrected for the initial conditions of patients. A limited number of process and structure measures can be included to facilitate learning. For example, to evaluate the success rate of techniques.
Solid Methodology
The VBHC theory has been implemented within the Meetbaar Beter practice. This is one of Meetbaar Beter’s cornerstones of success and it is seen as a guidance for other initiatives.
Key Factors Include:
- Outcomes Teams
Outcomes teams are formed to select, define, and perform maintenance on the most relevant outcome measures and initial conditions. Outcomes teams are multidisciplinary and are organised around one medical condition. They include both cardiologists and cardiothoracic surgeons from participating heart centres.
- Care Delivery Value Chain
The Care Delivery Value Chain (CDVC) is one of the main elements of Porter’s VBHC theory (Porter and Teisberg 2006). The CDVC is described by the outcome team and is used to define the medical condition, inclusion/exclusion criteria and any potentially relevant outcome measures.
- Selection Criteria and Outcomes Hierarchy
After defining the medical condition and CDVC, a list is created of all the available outcome measures using scientific and grey literature, the best practices, guidelines and so on. Subsequently, a small, feasible subset of the most relevant outcome measures is made by categorising them according to the Tiers of Porter's Outcomes Hierarchy (Porter 2010). Outcomes within each Tier are then selected and ranked based on the following criteria:
- Patient
Relevance - What is the impact
of this outcome on the patient’s quality of life? Large patient groups are
involved to assess this criterion.
- Medical Relevance - To
what extent is it possible for healthcare professionals to positively influence
the outcomes?
- Patient Volume -
How many patients is the outcome relevant to? How often does a negative outcome
occur?
- Validation
Validation is organised at several levels. Validation is a continuous process that ensures the independence and quality of Meetbaar Beter.
- Internal Validation: Medical and statistical experts engage in total quality management and medical decision-making.
- External Validation: An
international academic advisory council (IAAC) is organised which consists of
independent internationally renowned experts. The IAAC consists of three
dimensions:
- Methodology council - five experts in VBHC, change management and quality improvement.
- Medical council - over 25 renowned medical experts.
- Data management & statistics council - two internationally renowned experts.
- External Validation:A
sounding board is organised to ensure the involvement of health insurance
companies, patient organisations and government organisations. Discussions in
this sounding board have shown to be helpful in creating an alignment in
strategic goals and ensuring a correct interpretation of published data.
- Data Quality System
All participating heart centres are responsible for the completeness and quality of their own data. The Meetbaar Beter organisation is responsible for data quality control and for reporting feedback to heart centres. Meetbaar Beter has developed a data quality control system that includes quality control formats, audits performed by medical experts and compliance statements that must be signed by medical leadership at the heart centres
- Maintenance Cycle
After the annual publication of outcomes, the selected outcome measures and initial conditions are evaluated at several levels. Subject to evaluation are the standard sets of outcome measures, the definitions, data analysis methods and so on. Meetings are organised, questionnaires are sent to medical experts and data managers from participating heart centres and all comments are discussed by the outcome teams.
Any adjustments made in the maintenance cycle are regularly checked against all elements of the Meetbaar Beter methodology, such as the selection criteria described above.
Publication of Outcomes
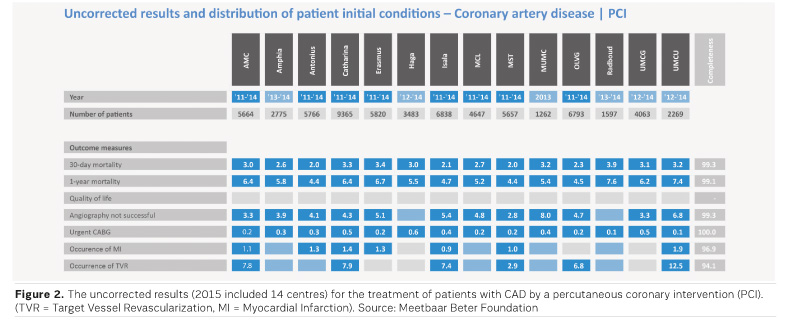
Meetbaar Beter publishes the outcomes per individual hospital and all heart centres combined in the annual Meetbaar Beter Books (Meetbaar Beter 2017). The primary goal is to provide insight into the outcomes and to facilitate generation of valid hypotheses on potential improvement. To define such hypotheses, data on outcomes must always be combined with medical expertise. Outcomes are published at three levels. The first level of publication is uncorrected results (Figure 2). The percentage of events is presented without taking differences in population characteristics into account. Although the comparison of heart centres based on these uncorrected results is not possible, it still gives insight into the true outcomes and offers possibilities for improvement.
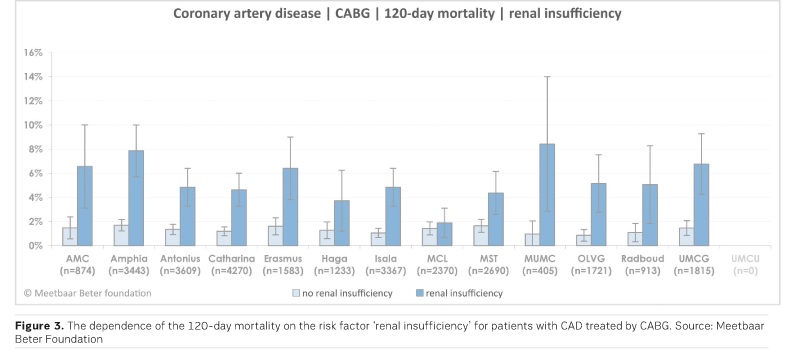
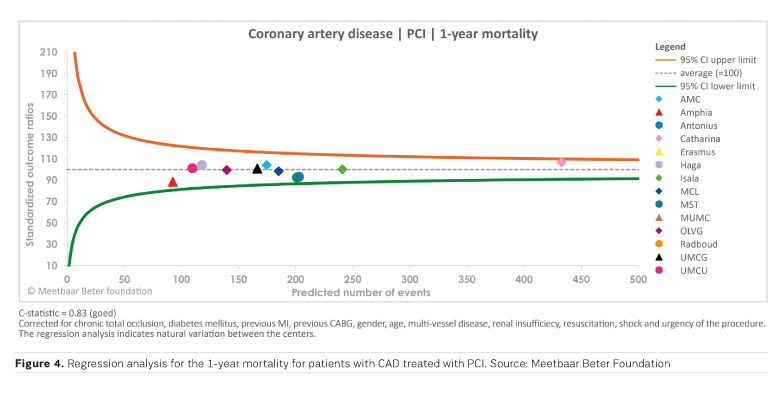
The second level of publication is segmented outcomes. Outcomes are presented in subgroups of initial conditions without risk correction (Figure 3). This gives doctors a deeper insight into the outcomes for relevant subgroups. Finally, if statistical data are adequate, regression analysis is made. Outcomes are corrected for the impact of the case mix across heart centres. Comparison between heart centres then becomes possible using these analyses (Figure 4).
Quality Improvement
Meetbaar Beter organises events that encourage doctors and heart centres to use insights in outcomes as a way to initiate quality improvement projects. Examples are round table sessions where doctors can select best practices; internal events that encourage the organisation of quality improvement projects and cycles and finally, brainstorm sessions with doctors to advance data analyses and create more insights. Several heart centres have been successful in organising improvement projects, and as a result have seen a progress in outcomes. Examples are the reduction of mortality after PCI for patients with renal insufficiency (in OLVG from 9.2% to 5.0%) and complications after PVI (reduction of tamponades in Catharina Hospital from 3.6% to 0.7%) and CABG (reduction of deep sternal wound infections in St. Antonius Hospital from 1.5% to 0.8%). More examples have been published in the Meetbaar Beter Books (Meetbaar Beter 2017).
A successful practice in Meetbaar Beter was rolled out in 2013. The 2013 regression analyses showed a significant lower mortality rate in Isala. The hypothesis proposed that a check in the operating room called the Isala Safety Check (ISC) contributed strongly to this relatively low mortality rate. The ISC was implemented in six other heart centres that voluntarily joined the project. The implementation will be subject to scientific evaluation.
In 2016, three potential best practices have been selected. These projects include the Haga Braincare Strategy, a protocol to reduce CVAs after heart surgery, a protocol for PCI patients with renal insufficiency used in OLVG; and the Cleveland Checklist used by the Catharina Hospital to reduce reoperations after heart surgery. These projects will be presented to other heart centres for a roll out in 2017.
Conclusion
VBHC is a concept that supports and encourages the improvement of quality and efficiency in healthcare. Meetbaar Beter has implemented VBHC in practice, creating an internationally unique and transparent learning environment. The solid methodology of Meetbaar Beter has created traction in Dutch healthcare, built enthusiasm amongst doctors and heart centres and has made a great leap forward in the transparency of healthcare quality. The first results of quality improvement projects within and amongst heart centres are more than promising. The ultimate success of Meetbaar Beter and VBHC will be concluded within a few years. With regards to Meetbaar Beter, success is defined by improved outcomes over the full range of medical conditions in heart care.
Dennis van Veghel is
one of the designers and founding fathers of Meetbaar Beter, and has been
director from the start. Educated as a health economist with a track record in
health insurance and health management, he was elected “most talented manager
in healthcare under 40” in the Netherlands in 2013.
References:
Larsson S, Lawyer P, Garellick G et al. (2012) Use of 13 disease registries in 5 countries demonstrates the potential to use outcome data to improve health care’s value. Health Aff (Millwood), 31(1): 220-7.
Meetbaar Beter (2017) Meetbaar Beter Boek. [Accessed: 31 January 2017] Available from meetbaarbeter.com/documents/meetbaar-beter-boeken
Porter ME (2010) What is value in health care? N Engl J Med, 363(26): 2477-81.
Porter ME, Teisberg EO (2006) Redefining health care. Boston, MA: Harvard Business School Publishing.
van Veghel D, Marteijn M, de Mol B2; Measurably Better Study Group and Advisory Board (2016) First results of a national initiative to enable quality improvement of cardiovascular care by transparently reporting on patient-relevant outcomes. Eur J Cardiothorac Surg, 49(6): 1660-9.
De Hart en Vaatgroep (2016) Kransslagadervernauwingen Resultaten geplande bypassoperaties. [Accessed: 31 January 2017] Available from: hartenvaatgroep.nl





