HealthManagement, Volume 16 - Issue 2, 2016
Protocols For Timely And Accurate Assessment
Acute aortic syndrome (AAS) is a life-threatening condition which requires urgent and immediate treatment. AAS can be diagnosed by using computed tomography (CT) imaging, but it is important that key protocols are followed in order to optimise scanning parameters. These recommendations, published by the British Journal of Radiology, provide vital guidance to make full use of recent advances in CT technology to rapidly and accurately diagnose this dangerous condition.
Important principles are identified for motion-free imaging of the aorta with particular emphasis on the use of ECG-gating techniques. The paper outlines how each imaging centre can optimise protocols for accurate diagnosis, optimise radiation dose and reduce the risk of false-positives.
First author, Dr Varut Vardhanabhuti, said, “These recommendations are the first of their kind in the UK and will ensure consistent high performance imaging in these patients”.
Dr Stephen Harden, one of the authors and Past President of the British Society of Cardiovascular Imaging (BSCI) and The British Society of Cardiovascular CT (BSCCT), said. “We are delighted to have worked with the BIR to produce this vital publication”.
Dr David Wilson, President of the British Institute of Radiology, said, “This is an invaluable resource for radiology teams. It has been a privilege to work with the BSCI and the BSCCT to publish this work which will inevitably enable rapid and accurate diagnosis for people with this dangerous condition”.
Below are some key excerpts from the paper:
Definitions of AAS
“Timely and accurate assessment of suspected AAS is vital in this potentially life-threatening condition with significant pre-hospital and in-hospital mortality rates of up to 20 percent and 30 percent, respectively. There are many definitions of AAS; however, for the purpose of this document, AAS is defined as aortic dissection, intramural haematoma and the complications arising from penetrating atherosclerotic aortic ulcer. These are not mutually exclusive and may represent variations on the same disease spectrum. Different classifications of aortic dissection exist, but to avoid confusion, we recommend using the most recently proposed classification of defining dissection as follows: Type A, involving the ascending aorta; Type B, limited to aorta portion distal to left subclavian artery; and Type B with aortic arch involvement, involving the arch (between the innominate and left subclavian arteries) but not involving the ascending aorta. The classification reflects the current management approach, w hich s upports t hat Type B dissection can be managed conservatively. With recent advances in CT scanning technology and increasing expertise in cardiovascular CT, the purpose of these recommendations are to outline the best practice for the investigation of suspected AAS so that unequivocal diagnosis can be made based on imaging. Specifically, accurate motion-free imaging is vital to eliminate the possibility of false-positive diagnoses, needless patient transfer and potentially disastrous unnecessary surgery, all of which have been reported.”
Assessment of Pre-Test Likelihood
Recommendation 1
“Assessment of pre-test clinical probability of AAS should be performed using American College of Cardiology Foundation (ACCF)/American Heart Association (AHA) guidance.
Initial evaluation of AAS should be based upon careful history and clinical examination (i.e. assessing for peripheral pulse deficits and potential end organ damage secondary to dissection) resulting in the ability to determine a pre-test likelihood of AAS. A summary of pre-test likelihood is shown in Figure 1 which categorises patients into low, intermediate or high likelihood of AAS .
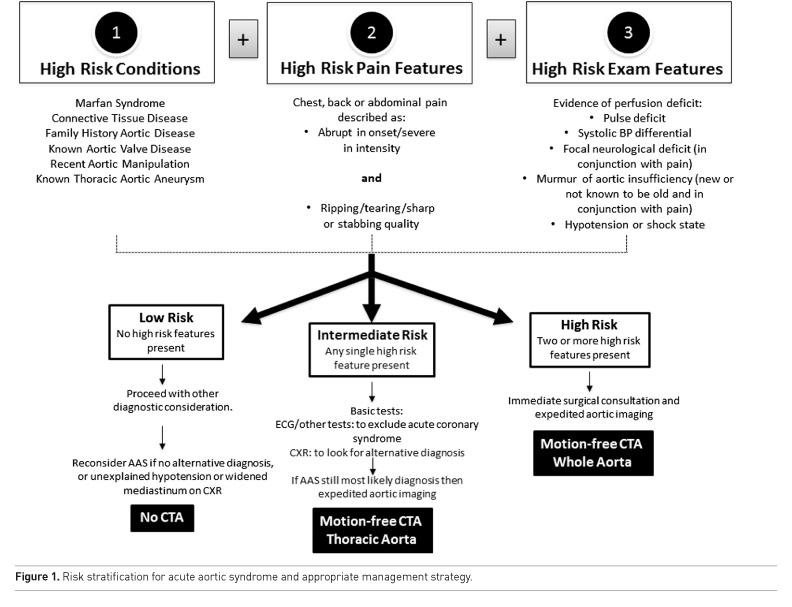
Recommendation 2
“Patients deemed to have intermediate or high risk should proceed to have imaging to establish a definitive diagnosis. In patients with low clinical risk, an alternative diagnosis should be considered but definitive imaging may also be required.”
Imaging Modality and Technique
Recommendation 3
“Imaging Modality And Technique When imaging is deemed appropriate, CT scan is the imaging modality of choice in an acute scenario.”
Recommendation 4
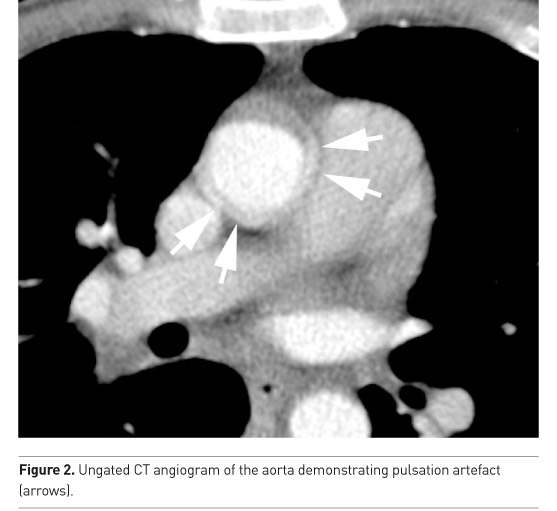
“All CT scans should be performed with the aim of producing motion-free images of the aortic root, which is prone to pulsation artefact (Figure 2).”
Recommendation 5
“A non-contrast ECG synchronisation CT scan should be performed to look for a rim of hyper-attenuation around the aortic wall (Figure 3).”

Coverage
Recommendation 6
“Coverage should be limited to thorax from aortic arch to diaphragmatic sulcus in the first instance, unless the patient is deemed high risk or has known disease.”
Scan Initiation and Contrast Regime
Recommendation 7
“A dedicated injection protocol should be used, taking into account the speed of scan acquisition and coverage with the aim to achieve adequate contrast concentration of at least 250 HU in the aorta.
There are three distinct methods of scan initiation that may be used: Fixed delay, Test bolus, and, Bolus tracking.”
Recommendation 8
“The key to adequate contrast opacification is to achieve an iodine delivery rate of at least 1.6 g s-1 (ideally up to 2 g s-1) when using a tube voltage of 120 kVp.”
Optimising CT Parameters
“Although diagnosis of AAS can be made using non-gated CT techniques, image quality at the aortic root is often suboptimal owing to motion artefact. This limits the diagnostic confidence and may on occasion mimic aortic dissection, leading to unnecessary further investigation and treatment, including sternotomy/ thoracotomy. The prevalence of aortic motion artefacts with non-gated CT has been reported to be high as 57–93 percent in some series. With ECG synchronisation, the occurrence of this artefact is less common, allowing motion-free visualisation of the aortic root and proximal coronary arteries in almost all cases.
To allow for prospective acquisition of the aorta, systems with detector coverage of at least 32 mm in the z-axis are recommended to make breath-holding possible during the whole scan acquisition. ECG synchronisation must be available to allow co-registration with heart rhythm. Scanners with ≥64 detector rows should be used in conjunction with narrow reconstructed slice thickness (<1 mm) in order to provide adequate multiplanar reformats, preferably with isotropic resolution utilising small voxel size through the use of a small field of view tailored to the aorta..”
Specific Protocol Examples
“For each scanner type, it is important that dedicated protocols are used and optimised. These protocols outlined below should be used as a guide, and variations may exist depending on differing parameters as outlined above. These protocols are advocated based upon expert BSCI user recommendations and in collaboration with UK application specialists.”
Basic Concept
“For a 64-detector-row system (including “128-slice” scanners and similar), prospective (“step-and-shoot”) acquisition should be employed where possible with phase selection based on HR. This is because the phase with minimal motion of the aortic root varies with HR. At HR <65 beats per minute (bpm), this is usually the end-diastolic phase. With HR >65 bpm, this is usually end-systolic phase. Where phase selection is not adjustable (e.g. on a scanner with prospective helical acquisition with diastolic phase acquisition only for slow HRs), then a retrospective protocol may need to be employed for patients with faster HRs. Retrospectively gated acquisitions can be used but should be only employed where no prospectively triggering alternative exists. Iterative reconstruction algorithms should be used where deemed appropriate to allow reduced radiation dose. For larger detector array or high-pitch dual-source systems, ECG synchronisation may not be necessary for motion-free imaging of the aorta.”
Conclusion
“With continuing rapid advancement of CT technologies and the need to standardise image acquisition coupled with an obligation for dose optimisation, these recommendations should allow centres to adopt protocols specific to their scanners for timely and accurate assessment using the basic principles outlined in this document. Acquisition is only one aspect of the scan and to properly implement this imaging strategy, centres must also adopt appropriate reporting facilities (e.g. picture archiving and communication system must be able to manage ECG-gating data sets, including handling of multiphasic reconstruction of retrospective acquisition), radiographer's training, as well as reporting expertise.
In terms of implementation, it has been shown that application of ECG gating by adequately trained staff has no impact on the workflow of the CT examination in acute setting.
Definitive diagnosis of ascending aortic pathology, eliminating false-positive scans, should become routine practice and no patient should undergo sternotomy/ thoracotomy or other intervention without an optimal AAS CT scan.”
Source:
The British Institute of Radiology (BIR ) Republished with permission of British Institute of Radiology, from [Recommendations for accurate CT diagnosis of suspected acute aortic syndrome (AAS )—on behalf of the British Society of Cardiovascular Imaging (BS CI)/British Society of Cardiovascular CT (BS CCT), Vardhanabhuti V, Nicol E, Morgan-Hughes G et al, 89, http://dx.doi.org/10.1259/bjr.20150705]
For full supporting references please see original article.
References:
Vardhanabhuti V, Nicol E, Morgan-Hughes G et al. (2016) Recommendations for accurate CT diagnosis of suspected acute aortic syndrome (AAS)—on behalf of the British Society of Cardiovascular Imaging (BSCI)/British Society of Cardiovascular CT (BSCCT). BJR, 89 (1061): 20150705.

