HealthManagement, Volume 20 - Issue 8, 2020
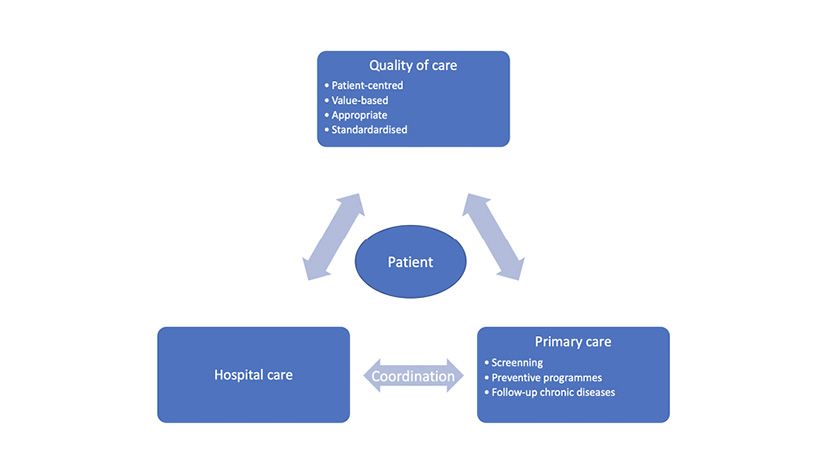
New care-delivery models should include screening, preventive check-ups and follow-up of patients with chronic diseases. All specialties, including radiology, need to be involved. This will involve significant investment, practice reorganisation and systems that are high-value based and patient-centred. This will require coordination and organisation between primary care centres and referral hospitals.
Key Points
- As an integral component of healthcare, radiology is involved in the whole patient process, from prevention to diagnosis and treatment of diseases.
- New care-delivery models should involve all specialties, including radiology.
- Harmonisation between primary care centres and hospital care is essential for an optimal and consistent care delivery.
- Radiology departments, in coordination with primary care physicians, can contribute to the diffusing of information and to educating the population.

Introduction
Our health care system and its various models are being questioned, particularly now with the challenges and added pressure of the current pandemic.
As an integral component of healthcare, radiology is involved in the whole patient process, from prevention to diagnosis and treatment of diseases.
The application of new technologies and artificial intelligence has led to advances in the medical world in general, and radiology in particular has seen the benefit of these improvements.
But the ever-growing number of imaging studies is having a serious impact on health care spending (Hendee et al. 2010). Among the factors contributing to this growth, an ageing population, chronic diseases and lifestyle have been identified.
This constellation of factors leads us to reflect on how we can improve our health system and how to organise it from primary care to hospital care. Seamless coordination between these two health care areas is essential, so that they can function together as a well-harmonised and interlinked work chain. Currently they function as independent entities with very little interconnection. This has led to deficiencies in care provision, excessive growth in imaging utilisation, a saturation of the system and increase in care spending, as well as dissatisfaction of health personnel.
New care-delivery models should involve all specialties, including radiology. A patient-centred and high-value based system that includes screening, preventive check-ups and follow-up of patients with chronic diseases will require a significant investment and precise organisation at all levels.
However, these changes must be introduced without neglecting the quality of care that should be a priority in every health system.
Primary Care
The first line of approach in care delivery is primary care. Whilst in primary care most patients present with chronic ailments, there will be some acute conditions that demand a rapid response to imaging requests and immediate reports are necessary (Insights Imaging 2010). Radiology departments must adapt their internal organisation to provide a fast-track, effective response. This requires a standardisation of the protocols, in agreement with the reference hospital centre, and a rapid reporting response. A collaborative effort will be needed to develop evidence-based appropriateness criteria for imaging studies that include education of primary care physicians and patients where necessary.
Implementation of computer-based decision support systems aligned with general practitioners can be an effective instrument to guide and standardise the appropriate use of imaging studies (Qayyum et al. 2013).
Taking a standardised approach can help avoid unnecessary hospital admissions for imaging procedures and further improve patient experience by avoiding overutilisation and/or duplication of tests.
Artificial intelligence systems and structured reporting are valuable preparation tools that will help in the standardisation and rapid response of reports. They should be extended to the entire radiological community and become the standard of care in radiology.
Hospital Care
Harmonisation between primary care centres and hospital care is essential for an optimal and consistent care delivery. Radiology departments have a key role to play in this coordination (Figure 1).
Hospital specialists need to offer suitable support to primary care physicians and promote their training and participation in common organisational decisions that will favour the integration of the two areas of care (Sarwar et al. 2015).
Screening/Preventive Programmes
Ischaemic and hypertensive heart disease, strokes, pulmonary infections, cancer, and diabetes still remain the most relevant causes of death in middle-, upper- and high-income countries.
The screening and management of cardiovascular disease, together with smoking-related diseases, comprise a major element in the workload of primary care practitioners. There is convincing evidence that GP-based preventive programmes for cardiovascular and smoking-related diseases and intervention are both feasible and cost-effective. Imaging is an essential tool in the risk-stratification and screening of these patients. Radiology departments, in coordination with primary care physicians, can contribute to the diffusing of information and to educating the population.
Chronic Diseases
A growing number of chronic diseases, principally heart disease, stroke, cancer, diabetes, and obesity, require prevention and screening programmes.
Experts have estimated that by 2030, chronic diseases will account for more than 70% of the global disease burden and will be responsible for 80% of deaths across the world (Beaglehole et al. 2003).
Primary care centres, in coordination with hospitals, can be part of the monitoring process of chronic diseases. This will require a change of scope and vision in physicians, and greater collaboration and networking between professionals, including radiologists.
Conclusion
Radiology departments have their part to play as a vehicle of coordination between primary care and hospital care, participating in prevention and screening programmes as well as in the diagnosis, assessment and planning of treatments.
Conflict of Interest
None
References:
Beaglehole R, Yach D (2003) Globalisation and the prevention and control of non-communicable disease: the neglected chronic diseases of adults. The Lancet, 362: 903–08.
Hendee WR, Becker GJ, Borgstede JP, Bosma J, Casarella WJ, Erickson BA, Maynard CD, Thrall JH, Wallner PE (2010) Addressing overutilization in medical imaging. Radiology, 257:240–245
Radiology and primary care in Europe. (2010) Insights Imaging, 1:46–52.
Sarwar A, Boland G, Monks A, Kruskal JB (2015) Metrics for radiologists in the era of value-based health care delivery. Radiographics, 35:866-878.
Qayyum A, Yu JPJ, Kansagra AP, von Fischer N, Costa D, Heller M, Kantartzis S, Plowman RS, Itri J (2013) Academic Radiology in the New Healthcare Delivery Environment. Acad Radiol, 20: 1511–1520.



