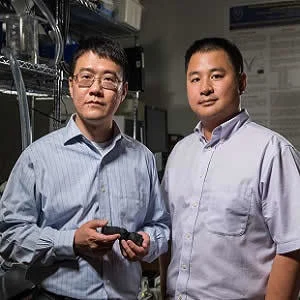
Researchers at Georgia Institute of Technology and the Piedmont Heart Institute have used standard medical imaging and 3-D printing technologies to create patient-specific heart valve models. These models can mimic the physiological qualities of the real valves and can help improve the success rate of TAVR by picking the right prosthetic and avoiding paravalvular leakage. The study is published in JACC: Cardiovascular Imaging.
Zhen Qian, chief of Cardiovascular Imaging Research at Piedmont Heart Institute, which is part of Piedmont Healthcare explains that paravalvular leakage is an important indicator that could convey how well the patient will do with the new valve in the long-run. By using patient-specific models with tissue-mimicking 3-D technology, it may be possible to test how the prosthetic valves interact with the 3-D models. This could help predict leakage.
Chuck Zhang, a professor in the Stewart School of Industrial and Systems Engineering at Georgia Tech believes that these 3-D printed valves can have significant impact on patient care in the future. Thousands of patients are diagnosed with heart valve disease each year and a large number of these patients undergo TAVR. Prosthetic valves are made in several different sizes by multiple manufacturers. There is always a risk of leakage if the valve is not a precise fit and if the blood flows around the prosthetic instead of through it. By reducing the risk of leakage, patient outcomes can be improved quite significantly. These 3-D printed models can enable interventional cardiologists to evaluate how well a prosthetic valve would fit a patient.
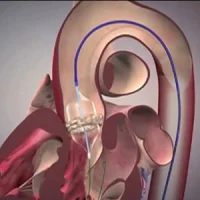
The models are created with a metamaterial design and then are made by a multi-material 3-D printer. Researchers have control over the diameter and curving of the metamaterial and they can thus try to achieve results that closely mimic the physiological properties of the tissue.
"Previous methods of using 3-D printers and a single material to create human organ models were limited to the physiological properties of the material used," Zhang said. "Our method of creating these models using metamaterial design and multi-material 3-D printing takes into account the mechanical behavior of the heart valves, mimicking the natural strain-stiffening behavior of soft tissues that comes from the interaction between elastin and collagen, two proteins found in heart valves."
The models have been developed on the basis of medical imaging of 18 patients who had undergone valve replacement surgery. The models were then outfitted with radioopaque beads and paired with the same type and size prosthetic valves that are used during valve replacement procedures. The prosthetics were implanted inside the models. The location of the radioopaque beads were analysed before and after the experiment to determine how the prosthetics interacted with the 3-D models. Any inconsistencies were identified and assigned values that formed a bulge index. A higher index meant a higher degree of leakage after valve placement.
The researchers plan to optimise the metamaterial design and 3-D printing process and also want to evaluate the use of these valves as a pre-surgery planning tool.
"Eventually, once a patient has a CT scan, we could create a model, try different kinds of valves in there, and tell the physician which one might work best," Qian said. "We could even predict that a patient would probably have moderate paravalvular leakage, but a balloon dilatation will solve it."
Source: Georgia Institute of Technology
Image Credit: Rob Felt
Latest Articles
heart valve, TAVR, 3-D printing, paravalvular leakage
Researchers at Georgia Institute of Technology and the Piedmont Heart Institute have used standard medical imaging and 3-D printing technologies to create patient-specific heart valve models. These models can mimic the physiological qualities of the real