Digitoxin reduced the risk of a composite endpoint of all-cause death and hospitalisation for worsening heart failure (HF) in patients with advanced HF and reduced ejection fraction (HFrEF), according to late-breaking results from the DIGIT-HF trial presented in a Hot Line session at ESC Congress 2025.
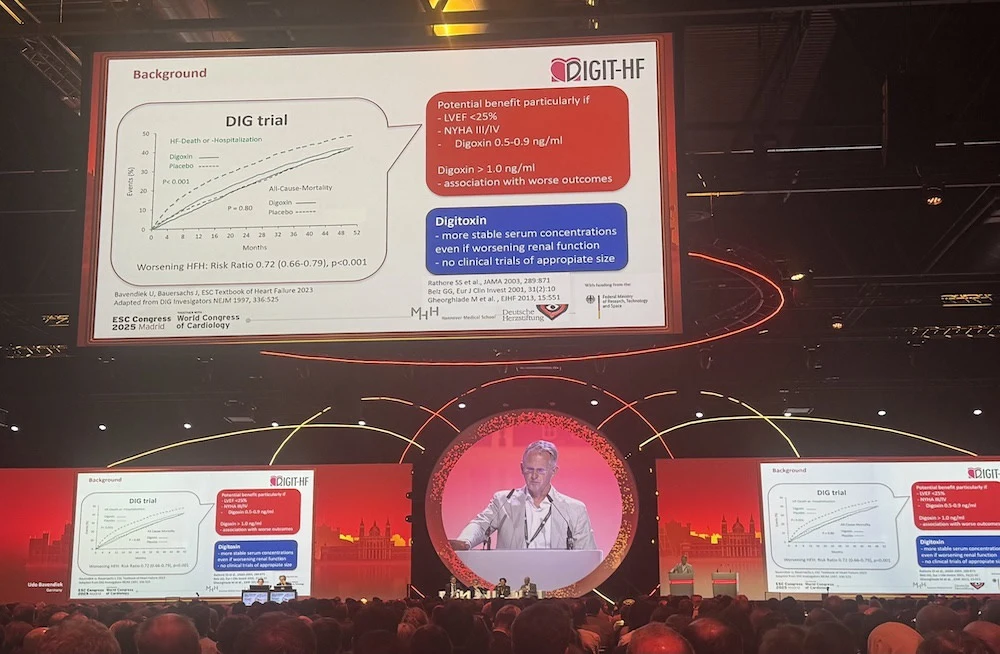
Cardiac glycosides such as digitoxin and digoxin have been used to treat HF for over two centuries. Yet robust evidence for their efficacy in HFrEF comes largely from the DIG trial, published in 1997. In that study, digoxin showed a neutral effect on mortality overall, but lower serum digoxin levels appeared to improve outcomes, whereas higher levels worsened prognosis. Digoxin significantly reduced hospitalisations for worsening HF, particularly in patients with more severe symptoms and markedly reduced left ventricular ejection fraction (LVEF).
The DIGIT-HF (Digitoxin to Improve Outcomes in Patients with Advanced Chronic Heart Failure) trial was designed to test digitoxin in patients with symptomatic HFrEF and high disease burden. The trial was conducted at 55 sites across Germany, Austria, and Serbia. Eligible patients had symptomatic HFrEF, defined as New York Heart Association (NYHA) class II with LVEF ≤30% or NYHA class III–IV with LVEF ≤40%. Participants were randomised 1:1 to digitoxin or placebo, on top of guideline-based standard care. Initial digitoxin dosing was 0.07 mg once daily, with blinded dose adjustment to 0.05 or 0.1 mg daily after six weeks to target plasma concentrations of 8–18 ng/ml. The primary endpoint was a composite of all-cause death or first hospitalisation for worsening HF, analysed by intention-to-treat (ITT).
The ITT cohort included 1,212 patients (mean age 66 years; 20% women) with a mean LVEF of 29%. HF severity was high: 70% were NYHA class III–IV. Background therapy was contemporary and comprehensive, with high device use (implantable cardioverter defibrillator 64%; cardiac resynchronisation therapy 25%).
Over a median follow-up of 36 months, the primary outcome occurred in 39.5% of patients in the digitoxin group versus 44.1% in the placebo group. All-cause mortality was 27.2% with digitoxin and 29.5% with placebo. First hospitalisation for worsening HF occurred in 28.1% and 30.4%, respectively. The total number of events (deaths or HF hospitalisations) was similar between groups (537 with digitoxin vs 531 with placebo).

Treatment effects were generally consistent across pre-specified subgroups, with particular benefit observed in patients with heart rate ≥75 bpm or systolic blood pressure ≤120 mmHg. Safety outcomes showed serious adverse events in 4.7% of digitoxin-treated patients and 2.8% of placebo-treated patients, driven mainly by cardiac disorders (3.4% vs 1.8%).

The findings show that with a simple dose-titration protocol, digitoxin significantly reduced the risk of death or hospitalisation for worsening HF in patients already receiving comprehensive modern therapy. Despite lower-than-expected enrolment, DIGIT-HF demonstrates that digitoxin offers an additional treatment option for HFrEF, particularly for patients with atrial fibrillation, elevated heart rate, low blood pressure, or impaired kidney function.
Source: ESC
Image Credit: ESC
References:
Bavendiek U et al. (2025) Digitoxin in Patients with Heart Failure and Reduced Ejection Fraction. NEJM.