Pulsed field ablation (PFA) was not superior to radiofrequency ablation (RFA) in patients with drug-resistant paroxysmal atrial fibrillation (AF), according to results from the late-breaking BEAT-PAROX-AF trial presented in a Hot Line session at ESC Congress 2025.
AF is the most common sustained cardiac arrhythmia. When antiarrhythmic drugs fail to control symptoms, catheter ablation is often performed to isolate the pulmonary veins and interrupt abnormal electrical activity.
Radiofrequency ablation is a well-established treatment for drug-resistant AF, but pulsed field ablation has emerged as a faster, nonthermal alternative that may offer more selective tissue targeting. Previous comparisons between PFA and thermal energy sources have been inconclusive. BEAT-PAROX-AF was designed to directly compare PFA with advanced RFA in this patient group.
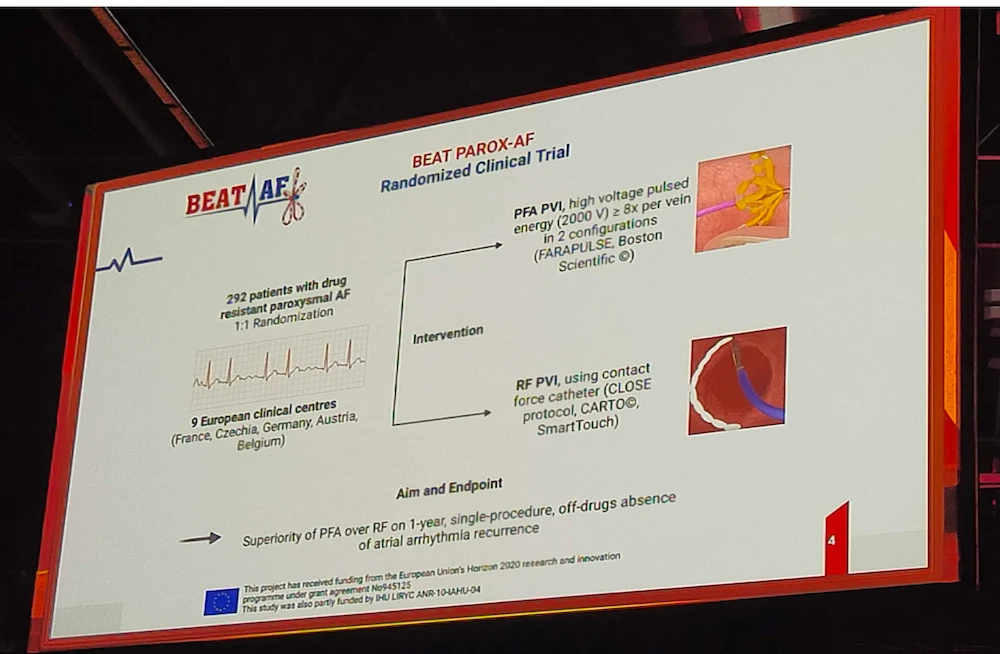
The trial was conducted across nine centres in France, Czechia, Germany, Austria and Belgium. Eligible patients (18–80 years) had symptomatic paroxysmal AF resistant to at least one antiarrhythmic drug, with an ESC Class I/IIa indication for ablation and ≥3 weeks of prior oral anticoagulation. Participants were randomised 1:1 to pulmonary vein isolation using either single-shot PFA or point-by-point RFA (CLOSE protocol). The primary endpoint was single-procedure success at 12 months, defined as no ≥30-second atrial arrhythmia recurrence, cardioversion, Class I/III antiarrhythmic drug resumption after a 2-month blanking period, or repeat ablation. Weekly self-recorded ECGs and symptom-triggered tracings were used for follow-up. A total of 289 patients (mean age 63.5 years; 42% female; mean AF duration 39 months) were analysed.
At 12 months, single-procedure success was high and similar between groups: 77.2% with PFA versus 77.6% with RFA. Procedure duration was significantly shorter with PFA (56 vs. 95 minutes).
Safety outcomes were excellent overall. Serious procedure-related events occurred in 3.4% of PFA patients and 7.6% of RFA patients. Complications were more frequent with RFA, including two tamponades and two cases of pulmonary vein stenosis >70%. PFA was associated with one transient ischaemic attack. No deaths, strokes, or persistent phrenic nerve palsy were reported.
Both PFA and CLOSE-protocol RFA achieved excellent efficacy, with comparable single-procedure success rates. PFA was associated with shorter procedure times and a trend toward fewer complications.
Source: ESC
Image Credit: ESC