Cardiac specialists have proposed new guidelines for heart transplant patients to receive donor organs. The proposed changes will improve the organ distribution process, increasing the survival rates of patients awaiting transplant surgery and post-transplant treatment. The recommendations are detailed in the January 2015 edition of the American Journal of Transplantation.
Currently, donor hearts are allocated according to urgency, wait time, geography and blood type. However, the heart transplant wait list is growing at a rate which outpaces the number of donated organs. The limitations of the existing three-tiered system prompted an evaluation of how to ensure a more fair and equitable distribution of donor organs.
Moving To A Multi-Tiered System
The Organ Procurement and Transplantation Network (OPTN) operates under contract with the US Department of Health and Human Services by the United Network for Organ Sharing (UNOS). A heart subcommittee comprised of representatives from cardiology, surgery and organ procurement administration, as well as transplant coordinators and a patient advocate, has been charged with evaluating the current system and proposing a framework for modelling wait list and post-transplant survival under the new guidelines.
Lead author Dan M. Meyer, MD, former chairman of the UNOS/OPTN heart subcommittee and currently a cardiothoracic surgeon at San Diego-based Scripps Health, believes the changes will dramatically improve patient health. "We think the proposed, modified multi-tiered allocation system embraces the key aspects of our charge, providing organs to the group of patients with the greatest need and who will gain the greatest benefit from heart transplant," said Meyer. Meyer is also a professor of cardiovascular and thoracic surgery at the University of Texas Southwestern Medical Center in Dallas.
Ventricular Assist Devices Factor Into Guideline Changes
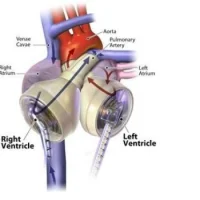
Including additional tiers in the guidelines helps provide doctors with more information about the patients' level of illness, taking into account the expected wait list mortality, rather than simply having a position on the list as a major driver of organ allocation. The geographic distribution of organs, post-transplant survival rates and the emerging population of patients surviving with ventricular assist devices also factor into the new guideline recommendations.
"Much of the impetus for this change in the allocation system stems from the dramatic increase in the use of ventricular assist devices for end-stage heart failure, an area that Scripps has focused on through the development of our successful Mechanical Circulatory Support Program," said Meyer. "Ventricular assist devices help to stabilise many patients on the waiting list."
Next Steps: UNOS Approval
Following further review and analysis, the subcommittee will present the proposed changes for public comment, after which a final version will be submitted to UNOS for consideration. UNOS has had only two major policy changes since 1988; the new guidelines would replace the current three-tiered system which was adopted in 1998.
Source: Scripps Health
Image Credit: Google Images