HealthManagement, Volume 4 - Issue 1, 2010
The European e-health IMPACT (2006, www.e-health-impact.eu) and
EHR IMPACT studies (2008, www.ehr-impact.eu) showed that effective
e-health solutions can substantially contribute to improvements in quality,
access and efficiency of healthcare, thus increasing the capacity of the supply
side.
How to Invest in
E-Health
The recently completed Financing e-health Study (2008, www.financing-e-health.eu) provided a generic guide for potential Ehealth investors to support them in the decision-making process. The guide, addressing decision makers and managers, sheds light on, and draws the connection to, the overall decision taking and change management processes that are part of E-health investment.
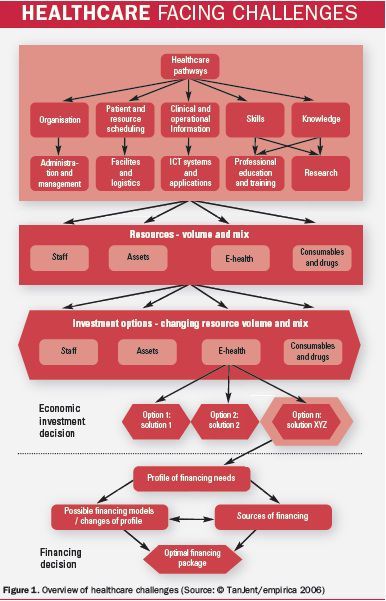
The main lesson regarding the models to adopt is to integrate the e-health investment decisions into the healthcare strategy of the organisation. E-health can deliver, but it has to become part of the general resource mix considered in addressing healthcare needs. Then, e-health investments are considered alongside more conventional investments and the ones with the best value for money can be selected.The financing model for the investment should only be considered after the economic analysis is being performed. The approach is illustrated in figure 1. Too often, investments are driven by affordability considerations and not by a comparison between investment and the economic value of its impact.
The Process of Economic and Financing Decisions
Common difficulties in e-health investments reflect the differences between E health and conventional ICT investment. E-health focuses on changes in the way healthcare is delivered, which is a demanding endeavour. In e-health investment, ICT serves only as an enabler, not as an end. In this context, the main obstacles to success include:
- Unrealistic timescales;
- Underestimated risks;
- Inherent procurement difficulties, and
- A common misperception of the nature of most valuable benefits of E health.
Timescales for
E-Health
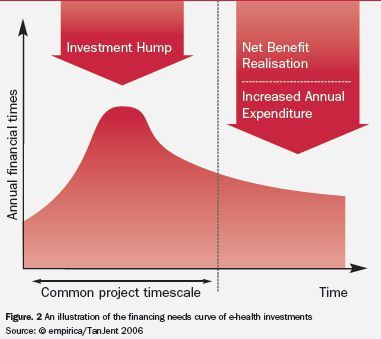
Project management for some e-health projects focuses mainly on deploying and managing the resources during the design, development and implementation stages, and possibly the initial stages of operation. This timescale can be too short for sustainable e-health investment, as shown in the chart below. It may fit an ICT project, but seldom provides the time required for the activities needed to realise net benefits: typically, about four years on average and at least eight years for EHRs. The appropriate timescales extend well beyond the business and financial planning of most health care provider organisations and can present financing challenges for e-health.
Instead, the e-health investment lifecycle should be set according
to the time needed to realise the required net benefit, the ultimate objective.
This will enable the management and productive utilisation of all the
reallocated resources, as part of the change lifecycle.
Managing Risks
Like all investments, as complexity and scale increase, so do the scope, probabilities and costs of risk. Plans for e-health investment seldom evaluate the potential of risk realistically. The result is no recognition of risks as costs, no mitigation and no respective financial provision. This in turn leads to understated costs and overstated benefits, which is not a good foundation for e-health investment.
For example, engagement with users and other stakeholders is a high-risk activity. Where it is not successful, the effect can inhibit e-health activities for many years. Where it is successful, e-health investors tend to apologise for the extended timescales, understating the significant reduction in risk by pursuing effective collaboration and engagement, especially with healthcare professionals.
Procurement
Another concern is that there is still a mismatch between supply and demand for e- Health systems and tools. Experts consulted in the Financing E-health Study reported of repeated occasions in which ICT suppliers were not in the position to supply the solutions needed for benefit realisation, leaving investors with the task to develop rather than procure. At the same time, requirements are not always set effectively by procurers, something that can make the lives of ICT vendors more difficult.
Garnering Added Value from E-Health
The challenge is to ensure that the total investment matches an appropriate total economic benefit. It is important to treat E health investment in the same way as other new investments in healthcare, such as new drugs and surgical techniques. It should not be a means of saving money and improving overall cash flow, but an investment in better healthcare.
Large proportions of economic benefits from e-health are from quality, including patient safety, and time improvements. E health is usually a net investment, with a negative financial return, so financial benefits must be realistic in their value and their timing. Sustainable e-health investment requires that all decision takers and financial stakeholders be clear about the distinction between economic benefits and financial savings.
The task is to identify, define and describe all the benefits
needed from better information for each strategic initiative. There are several
examples, such as informing patients better, improving patient safety and
timeliness, streamlining healthcare, improving clinical effectiveness by
sharing patient information with other healthcare professionals that form the
multidisciplinary team providing patient care, and modernising healthcare: all
quality goals. Some citizens, such as those in remote locations, may need
improved access to hospital and other specialist health services. Improving efficiency
by saving time and cutting waste may be a priority.
Impact of
E-Health on HospitalManagement
The critical requirement for leaders, executives and e-health stakeholders is to be able to deal with e-health investment as an integrated part of all healthcare investment. Finance executives and managers have a more specific role. First, they need to understand the value and impact of e-health, so they can extend and develop financial planning to deal with e-health investment timescales. Second, they need to extend their financial management skills to be able to develop ways to invest in better value.
This expands the principle of organisational change from healthcare professionals who use the e-health investment directly, to the whole organisation. It is just as uncomfortable for executives as it is for healthcare professionals. As healthcare professionals use new information to improve quality, access and efficiency, executives are confronted with new clinical, working, and information exchange practices: they have a different organisation to run.