Artificial intelligence (AI) is rapidly reshaping the healthcare industry, with its integration into clinical decision support systems (CDSS) marking a significant advancement in patient care. These systems, designed to assist healthcare professionals with evidence-based insights, are essential in improving diagnostic accuracy, optimising treatment plans and enhancing patient safety. By leveraging AI technologies such as machine learning, natural language processing (NLP) and deep learning, CDSS have progressed beyond traditional tools, enabling more precise, efficient and personalised medical decisions.
The Evolution of Clinical Decision Support Systems
Clinical decision support systems have been instrumental in healthcare since their inception in the 1970s, evolving from rule-based frameworks to sophisticated AI-powered tools. Early CDSS, such as the pioneering MYCIN system developed at Stanford University, relied on "knowledge-based" models. These systems used predefined IF-THEN rules derived from medical literature, clinical guidelines and patient data to generate recommendations for diagnosis and treatment. While revolutionary at the time, these systems were limited by their reliance on static knowledge bases and fixed algorithms, which constrained their ability to adapt to new information or evolving medical practices.
As healthcare data has grown in volume and complexity, non-knowledge-based CDSS have emerged. These systems leverage AI to process vast datasets, identifying patterns and correlations that elude human interpretation. Unlike their knowledge-based predecessors, non-knowledge-based systems utilise machine learning to continuously analyse historical patient data and refine their predictions. This evolution has transformed CDSS into dynamic, adaptive tools capable of handling complex medical scenarios. By integrating AI technologies, these systems offer real-time insights that enhance clinical decision-making, enabling earlier diagnoses, reducing human error and optimising patient outcomes.
The distinction between knowledge-based and non-knowledge-based systems highlights AI's transformative impact on CDSS. While traditional systems remain valuable for their reliability and evidence-based approach, the flexibility and data-driven capabilities of AI-powered CDSS represent a new frontier in healthcare. This shift underscores the importance of integrating AI to address the challenges of modern medicine and unlock the full potential of clinical decision support.
AI in Medical Diagnostics and Treatment Planning
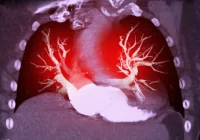
Integrating AI in medical diagnostics has unlocked unprecedented possibilities for precision medicine. AI-powered CDSS can process data from electronic health records (EHRs), medical literature and clinical notes, offering personalised insights tailored to individual patients. In diagnostics, AI systems have demonstrated proficiency in identifying diseases such as skin cancer and heart failure with accuracy comparable to trained specialists. For instance, deep learning models used in CDSS can detect subtle anomalies in imaging or lab results, facilitating early intervention and improving patient prognoses.
In the case of sepsis, AI-driven CDSS is proving transformative, offering real-time risk assessments that enable emergency room and intensive care clinicians to act swiftly. This capability is crucial in preventing severe complications and saving lives. Furthermore, AI's ability to process vast amounts of unstructured data, including clinical notes and imaging reports, allows it to extract valuable insights that might otherwise be missed, further enhancing diagnostic accuracy.
Beyond diagnostics, AI enhances treatment planning by generating tailored recommendations based on a patient’s medical history, genetic profile and current health status. This personalised approach minimises trial-and-error treatments, improving outcomes and reducing healthcare costs. Additionally, natural language processing enables AI systems to extract actionable insights from unstructured clinical data, ensuring that no critical information is overlooked in decision-making processes.
AI-powered CDSS also play an increasing role in predictive analytics, helping clinicians anticipate disease progression and tailor interventions accordingly. For example, recurrent neural networks, a form of machine learning, have shown promise in predicting the likelihood of heart failure by identifying subtle patterns in patient data. These predictive capabilities illustrate AI’s potential to not only support clinical decisions but also proactively mitigate risks and ensure earlier interventions.
Enhancing Patient Safety and Healthcare Efficiency
AI-powered CDSS significantly enhance patient safety by minimising errors and supporting clinicians with real-time, evidence-based recommendations. These systems are particularly valuable in high-stakes environments such as emergency rooms and intensive care units, where timely and accurate decisions are critical. By continuously monitoring patient data and analysing it against established benchmarks, AI systems can flag potential complications before they escalate, allowing clinicians to intervene promptly.
For instance, AI has demonstrated effectiveness in identifying patients at risk of sepsis or heart failure, enabling early interventions that save lives. These capabilities improve individual outcomes and contribute to broader public health goals by reducing preventable complications and hospital readmissions. Moreover, AI systems can learn from past cases, ensuring that their recommendations evolve and improve over time, further enhancing patient safety.
The impact of AI extends beyond clinical outcomes to operational efficiency. By automating routine tasks, such as data entry and report generation, AI reduces the administrative burden on healthcare professionals, freeing them to focus on patient care. This efficiency translates into cost savings for healthcare providers and improved accessibility for patients, making high-quality care more widely available. AI also facilitates better resource allocation by providing insights into patient flow and staffing needs, enabling healthcare organisations to optimise their operations.
The combination of improved safety, personalised care, and operational efficiency underscores AI's transformative potential in healthcare. By addressing both clinical and administrative challenges, AI-powered CDSS are expected to set a new standard for effective and efficient patient care.
Integrating artificial intelligence into clinical decision support systems is profoundly transforming healthcare, offering transformative benefits in diagnostics, treatment planning and patient safety. With AI’s power, CDSS have evolved into indispensable tools for modern medicine, improving outcomes while reducing costs and inefficiencies. As AI technologies continue to advance, their potential to reshape clinical decision-making and enhance patient care will only grow. This progress not only benefits healthcare providers and patients but also lays the foundation for a future where precision medicine becomes the norm, ensuring that the right care is delivered at the right time.
Source: Healthcare Transformers
Image Credit: iStock