The use of AI-assisted technology in cancer contouring for prostate cancer shows promising improvements in accuracy compared to traditional methods. Conventional contouring often underestimates cancer extent, leading to suboptimal treatment outcomes. AI tools, such as "Unfold AI" by Avenda Health, leverage multimodal clinical data to better visualise cancer probability. Recent studies have demonstrated that AI software outperforms conventional methods in accurately defining cancer boundaries and assessing the likelihood of residual clinically significant prostate cancer (csPCa). This advancement is particularly crucial for focal therapy (FT), which aims to eradicate cancer while preserving quality of life by targeting specific areas instead of the entire prostate gland. The study of effectiveness of AI in improving treatment planning underscores its potential to enhance patient outcomes by providing precise and reproducible assessments of cancer extent.
Evaluating AI-Assisted Cancer Contouring in Prostate Cancer Treatment Planning
In a multi-reader multicase study, ten physicians (urologists and radiologists) from five institutions participated in a fully crossed design where each reviewed the same cases twice: once using conventional manual cancer contouring (SOC) and once using AI-assisted contouring. The study aimed to evaluate the accuracy and clinical impact of AI in prostate cancer treatment planning.
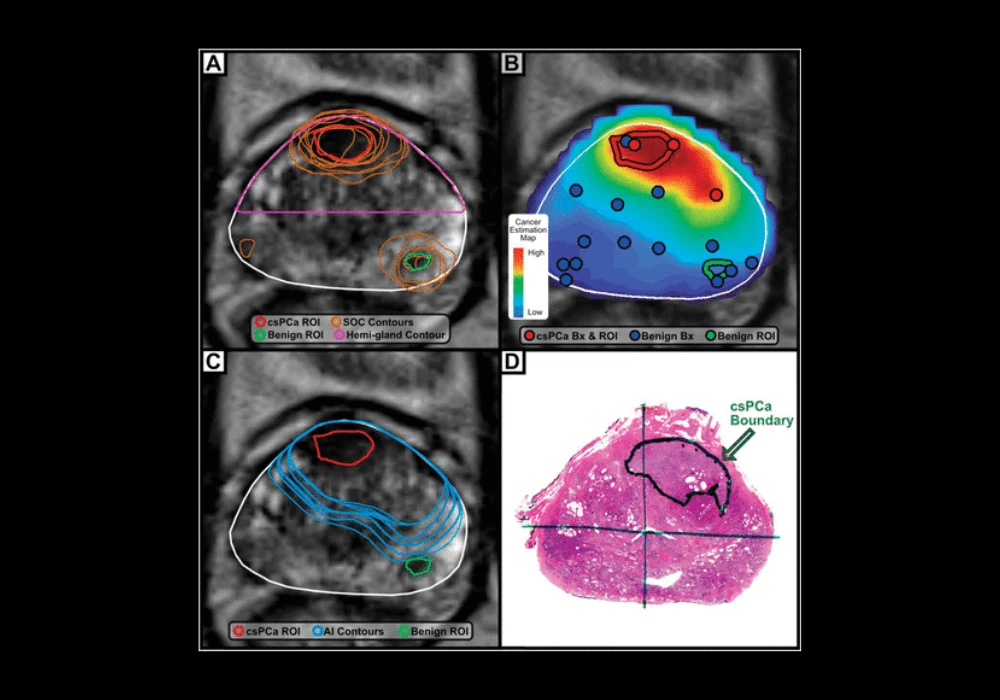
During the SOC phase, readers manually delineated cancer contours after reviewing diagnostic data including MRI scans and biopsy reports. After a washout period to minimise bias, they repeated contouring with AI assistance, which provided 3D cancer estimation maps based on MRI data, biopsy results, and PSA levels. The AI software generated contours aiming to encapsulate all clinically significant prostate cancer (csPCa), supported by an "encapsulation confidence score" indicating the likelihood of complete csPCa encapsulation.
A subset of readers recorded their treatment recommendations following each contouring phase to assess changes in clinical decision-making influenced by AI-assisted contours. Evaluation metrics included voxel-wise balanced accuracy (a combination of sensitivity and specificity), negative margin rate (proportion of cases where csPCa was entirely encapsulated), and contouring time. Ground truth data from whole mount pathology served as the benchmark for assessing contouring accuracy.
The study concluded by comparing the performance of SOC and AI-assisted contours across various metrics, focusing on clinical relevance and accuracy in csPCa identification. Statistical analyses were conducted to determine significant differences and validate the impact of AI on treatment planning decisions in prostate cancer management.
AI-Driven Advancements in Prostate Cancer: Enhancing Accuracy and Guiding Treatment Decisions
AI-assisted cancer contouring outperformed both standard-of-care (SOC) and hemigland methods across 50 cases. AI contours achieved significantly higher balanced accuracy (84.7% vs 67.2% for SOC and 75.9% for hemigland, P < .001), greater sensitivity (97.4% vs 38.2% for SOC, P < .001), and higher specificity (72.1% vs 53.4% for hemigland, P < .001). The negative margin rate with AI was markedly superior to SOC (72.8% vs 1.6%, P < .001), with reduced contouring time (mean 2.0 vs 3.5 minutes, P < .001). While hemigland contours showed a higher negative margin rate than AI, the difference was not statistically significant (86.0% vs 72.8%, P = .7).
Among urologists and radiologists, AI-assisted contours consistently demonstrated improved balanced accuracy compared to SOC (84.6% vs 68.0% for urologists and 85.0% vs 65.4% for radiologists). Survey results from 7 readers revealed significant shifts in prostate cancer management decisions with AI use, influencing treatment recommendations in 42% of cases (28% for urologists, 61% for radiologists, P < .001). Urologists leaned towards recommending focal therapy more often with AI (21.5% vs 12.5% SOC) and less radical prostatectomy (52.0% vs 58.0% SOC), while radiologists tended to decrease recommendations for radiation therapy (33.3% vs 38.0% SOC) and increase recommendations for radical prostatectomy (16.7% vs 11.3% SOC).
Success of AI in Contouring and Treatment Decision-Making
Generating accurate cancer contours for prostate cancer proved challenging with conventional methods (SOC), which tended to underestimate the extent of clinically significant prostate cancer (csPCa). This was attributed to reliance on MRI appearances, that often do not reveal the full tumour extent. AI emerged as a solution, demonstrating significantly better accuracy compared to SOC and hemigland methods in the study. AI-assisted contours achieved a higher balance between sensitivity and specificity, substantially increasing the negative margin rate from 1.6% with SOC to 72.8%. AI also influenced clinical decision-making, prompting changes in treatment recommendations in over 25% of cases, particularly favouring focal therapy over whole gland therapy.
The study acknowledged limitations such as its single-institution case derivation and reliance on radical prostatectomy cases, potentially skewing results towards more advanced disease. Despite these constraints, AI showed promise in improving treatment planning accuracy and patient-specific therapy selection. Future research directions include validating AI in broader patient populations and exploring its potential impacts on biopsy strategies and targeted therapies. AI-assisted cancer contouring represents a significant advancement over current practices, offering potential enhancements in clinical outcomes and treatment efficacy in prostate cancer management.
Source & Image Credit: Journal of Urology