HealthManagement, Volume 25 - Issue 1, 2025
Artificial Intelligence is reshaping healthcare by enhancing diagnostics, improving clinical outcomes and optimising operational efficiency. It enables remote patient care, streamlines workflows and reduces healthcare costs. AI also contributes to sustainability by minimising waste and energy consumption. However, realising its full potential requires integrated frameworks and multidimensional metrics to measure impact across clinical, operational and environmental dimensions.
Key Points
- AI improves accuracy, speeds up disease detection and enables personalised treatment.
- It reduces inefficiencies, lowers costs and streamlines workflows, optimising operations.
- AI bridges healthcare gaps through telemedicine and remote patient monitoring.
- It supports sustainability by minimising waste, reducing energy consumption and lowering carbon footprints.
- AI’s impact must be measured using integrated frameworks and metrics to align with healthcare goals.
Artificial Intelligence (AI) is transforming healthcare, but what the healthcare sector has seen so far is just the tip of the iceberg. AI’s ability to improve clinical outcomes, reduce inefficiencies and connect isolated communities is remarkable—but it merely scratches the surface of what is possible. Beneath this visible success lies a vast, uncharted potential waiting to be realised. While AI systems can be energy-intensive and contribute to sustainability challenges due to their high computational demands (Bratan et al. 2024), AI also holds significant potential to advance sustainable development as a result of optimising resource use, enhancing operational efficiency, reducing waste and expanding equitable access to essential services like healthcare (Ueda et al. 2024). To unlock this potential, the healthcare sector must move beyond fragmented innovations. What is needed is a clear path encompassing cohesive frameworks with proactive, multidimensional metrics that allow measuring the outcomes of AI in healthcare (Chustecki 2024).
The Intriguing Promise of AI in Healthcare
AI has already proven its worth, reshaping how diseases are diagnosed, managed and prevented. Hospitals across the globe are leveraging its computational might to streamline workflows, accelerate life-saving decisions and alleviate resource constraints. By collaborating with AI, radiologists are not just faster but more precise—able to identify subtle abnormalities with machine-learning tools while dedicating time to solving complex cases. AI also entails the potential to enable remote clinics to no longer be disconnected from specialists, with AI-powered telehealth tools bridging that gap in a matter of seconds. Indeed, there are numerous real-world examples of AI transforming healthcare, including enhancing diagnostic precision in imaging, optimising workflows and enabling remote patient monitoring and proactive care, all of which contribute to improved clinical outcomes and patient experiences (Philips Editorial Team 2022). Hence, AI’s ability to revolutionise direct clinical outcomes is vast, offering unparalleled opportunities to enhance diagnostic accuracy, personalise treatments and improve patient care at an unprecedented scale.
Beyond clinical outcomes, AI can also be considered a facilitator of significant clinical improvements—quick, accurate diagnostics and timely treatments. However, looking deeper, one will discover operational efficiencies that extend well beyond clinical care. Healthcare facilities operate as energy-intensive ecosystems, often burdened by inefficient practices. When applied thoughtfully, AI can transform how hospitals utilise resources. From optimising energy consumption to accurately predicting supply chain demands, it can reduce carbon footprints and lower costs. For instance, a working paper from the Economics of Artificial Intelligence Conference (Sahni et al. 2023) estimates that broader AI adoption could lead to savings of 5 to 10 per cent in U. S. healthcare spending, totalling approximately €192 billion to €345 billion ($200 billion to $360 billion) each year. The global savings may thus be immense. These savings flow throughout the value chain by enhancing resource utilisation, minimising waste and promoting innovation, which ultimately leads to better environmental, social and economic outcomes. Hence, AI contributes to operational efficiency by optimising resource use, reducing waste and streamlining energy-intensive processes, creating more sustainable and cost-effective healthcare systems.
Building on the foundation of operational efficiency, AI’s potential extends further to address one of healthcare’s most pressing challenges: breaking down geographic and economic barriers to ensure equitable access to quality care for all, accessibility. AI is helping healthcare leap geographic and economic barriers. From telemedicine platforms that connect rural populations with world-class care to predictive algorithms that ensure supplies reach the areas that need them most, technology is rewriting the rules of equity in care. Consider, for example, the case of an AI-powered remote monitoring system for diabetes management (Tenovi 2024), which tracks blood glucose levels, physical activity and diet to provide personalised meal and exercise plans. This system helps individuals manage their condition effectively, regardless of location or proximity to specialised healthcare facilities. Similarly, AI-driven heart failure monitoring devices analyse real-time data like heart rate and blood pressure, enabling early detection of exacerbations and preventing costly hospitalisations. These examples showcase AI’s potential to transform remote healthcare, making advanced care accessible to patients worldwide.
These outcomes are undoubtedly crucial, delivering significant improvements in clinical care, operational efficiency and accessibility. Yet, as incredible as these strides are, they are only part of a much larger story. These currently visible advancements—the intriguing clinical promises, optimised workflows and enhanced patient access—form the innermost layers of a convoluted structure. Beyond this, AI holds the power to fundamentally change the way healthcare interacts with society and the planet.
Unveiling the Hidden Layers
What is often missing in these discussions on these layers is their direct and indirect contribution to social and ecological sustainability. On the one hand, in terms of direct contributions, the previous layers generally underscore tangible outcomes—such as improved patient care and cost savings—yet often overlook their broader environmental implications. First, AI’s ability to enhance diagnostic accuracy and streamline care pathways indirectly reduces resource waste, such as unnecessary tests, hospital readmissions and excessive medication use. For example, predictive models can minimise overstocking in supply chains while optimised treatment plans reduce the environmental impact of prolonged hospital stays. Second, operational efficiencies brought about by AI—such as energy optimisation in hospitals and predictive maintenance of equipment—significantly lower the carbon footprint of healthcare facilities. For instance, AI-driven energy management systems ensure minimal resource wastage by adjusting lighting, heating and cooling based on real-time demand. Third, accessibility advancements like telemedicine and remote monitoring contribute further to sustainability by reducing travel-related emissions. For example, fewer patient journeys not only decrease greenhouse gas emissions but also alleviate the strain on infrastructure in underserved regions. Taken together, these indirect contributions across clinical care, operational efficiency and accessibility advancements highlight the deeper, systemic role AI can play in aligning healthcare systems with broader sustainability goals, even beyond its immediate and visible impacts.
This broader perspective is depicted in the following diagram (Figure 1), illustrating how AI’s influence spans from immediate clinical outcomes to system-wide social and ecological sustainability. As one moves from the inner to the outer layers of the diagram, the focus on AI’s applications in healthcare may seem to diminish. Yet the outcomes of the first three layers—direct clinical improvements, operational efficiencies and enhanced accessibility—are not merely compartmentalised gains; in reality, each contributes directly to social and ecological sustainability. By reducing hospital waste, facilitating remote care and streamlining resource usage, AI’s more immediate benefits cascade into broader, system-wide transformations that lower carbon footprints and bridge healthcare gaps across diverse communities. Although social and ecological sustainability is often the hardest layer to quantify, it is precisely this realm that elevates AI from a narrow clinical tool to a catalyst for long-term societal and environmental well-being. Embracing the fluid interconnections among these layers is crucial, ensuring that AI’s impact extends beyond quick wins and accelerates healthcare’s transformation into a truly sustainable and equitable ecosystem.
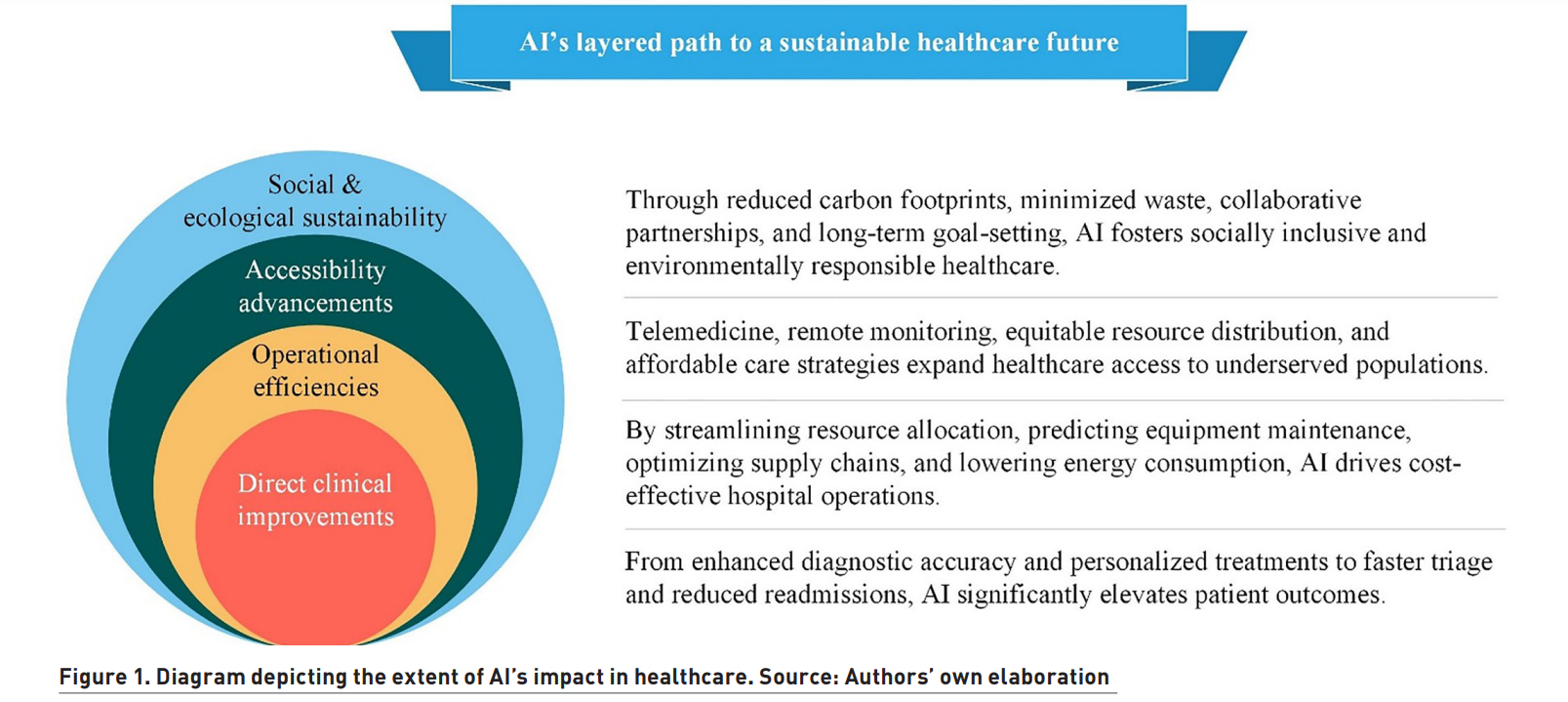
Though overshadowed by the breakthroughs at the centre, the outer layers of the diagram hold equally pivotal roles in shaping the broader trajectory of AI in healthcare. This is primarily due to two reasons: first, the immense attention commanded by clinical breakthroughs—such as improved diagnostic precision, personalised treatments and life-saving interventions—tends to overshadow the broader systemic and societal impacts represented by the outer layers. Second, the contributions of the outer layers, such as operational efficiency, accessibility and particularly social and ecological sustainability, are inherently more challenging to measure and quantify. These impacts often span long-term outcomes and involve complex interdependencies that do not lend themselves to straightforward metrics. Despite being less talked about, these outer layers are equally critical, as they represent the broader potential of AI to transform healthcare into a system that is efficient, inclusive and deeply aligned with sustainability goals. Ignoring these layers risks undervaluing AI’s capacity to address some of the healthcare system’s most pressing challenges while shaping its future in meaningful and transformative ways.
However, there is a crucial point to consider: without reliable benchmarks and holistic evaluation tools, many of these more profound potential risks remain hidden, undervalued or unachieved. This is where multidimensional metrics become indispensable. Tools that combine measurements of energy savings, carbon reductions, patient outcomes and social equity—could provide a roadmap to align AI innovations with broader sustainability goals. Furthermore, such frameworks and metrics also provide a way to communicate the bright side of AI’s adoption in healthcare.
The Metrics Needed to Measure Progress Across the Layers
For AI to ascend beyond these visible achievements and redefine healthcare on a systemic level, various frameworks that assess its impact holistically are needed. Current implementations often focus on narrow objectives like cost-cutting or technical precision. While these are important, they alone are insufficient. What about the carbon footprint of AI systems themselves? What about their long-term role in reducing global health disparities? These concerns are reinforced by insights from the Journal of Big Data, where Raman et al. (2024) assert the critical need for a unified approach to AI innovation—one that seamlessly integrates sustainability goals to shape a more responsible and transformative trajectory for AI in healthcare. Along the same line, another study by Ueda et al. (2024) suggests that “The integration of AI sustainability within broader institutional and societal sustainability efforts will be crucial for achieving a future where healthcare not only improves patient outcomes but also promotes environmental stewardship.”
To unlock AI’s full potential in healthcare and ensure it aligns with sustainability goals, robust frameworks are needed to measure its impact across various layers. Each layer—whether direct clinical improvements, operational efficiencies, accessibility advancements or social and ecological sustainability—requires tailored, multidimensional metrics that reflect its unique contributions.
For the innermost layer, metrics should focus on clinical outcomes such as diagnostic accuracy, treatment personalisation and patient recovery rates. These measures can highlight how AI is revolutionising healthcare at its core by improving care quality and saving lives.
In the operational efficiency layer, metrics must evaluate resource optimisation, such as reductions in energy consumption, hospital waste and operational costs. For example, tracking energy savings from AI-automated hospital management systems or quantifying cost reductions from supply chain predictions can make the case for AI’s economic and environmental value.
Moving outward, the accessibility advancements layer demands metrics that assess AI’s ability to bridge gaps in care delivery. These might include the number of rural or underserved communities gaining access to telemedicine services, the reduction in patient wait times or the distribution of medical supplies to areas in need—clear indicators of AI’s role in making healthcare more aligned with social and ecological sustainability.
Finally, in the outermost layer of social and ecological sustainability, the metrics must focus on long-term impacts, such as carbon footprint reductions in healthcare systems, progress toward carbon-neutral facilities and partnerships driving broader sustainability initiatives. These measures ensure AI is not just solving immediate problems but is also contributing to a healthier planet and society.
When these metrics are linked to each layer of the diagram, they can provide a cohesive roadmap for assessing AI’s transformative potential in healthcare. Transparent, real-time dashboards are critical for assessing AI’s impact across all layers of the diagram, particularly in the healthcare sector, where timely and actionable insights can directly influence patient outcomes and system-wide efficiency. For example, in hospitals utilising AI-powered energy management systems, dashboards can track energy consumption patterns in real time, enabling administrators to optimise lighting, heating and cooling systems based on patient flow and occupancy levels. Such tools not only reduce operational costs but also lower carbon emissions, aligning healthcare facilities with sustainability goals.
In clinical settings, AI-integrated dashboards can provide physicians with up-to-the-minute data on patient health metrics, such as vital signs from remote monitoring devices. For instance, a patient with chronic heart failure using an AI-enabled monitoring device can have their data—heart rate, blood pressure and respiratory rate—visualised on a real-time dashboard.
At a systemic level, healthcare organisations can use AI-driven dashboards to monitor supply chain efficiency. By tracking inventory levels, predicting demand and flagging potential shortages, these tools ensure that resources like essential medications and medical equipment are allocated where they are needed most, minimising waste and avoiding supply disruptions.
By embedding transparent, real-time dashboards into healthcare workflows, healthcare organisations gain a powerful tool to measure the direct and systemic contributions of AI. These dashboards ensure that advancements in clinical outcomes, operational efficiency, accessibility and sustainability are not only visible but also actionable, driving a future where healthcare systems are more efficient, equitable and environmentally responsible.
Looking to the Horizon: Aligning AI’s Promise with Sustainable Healthcare Goals
As AI’s transformative role is examined across the layers of the diagram, from direct clinical improvements to social and ecological sustainability, it becomes clear that the journey is only beginning. The road ahead requires intentionality and collaboration to ensure that AI not only reaches its potential in enhancing healthcare outcomes but also aligns with broader sustainability goals. Governments, healthcare organisations and tech innovators must work together to embed sustainability across all layers of the healthcare system.
This begins with actionable steps, starting with the implementation of transparent, real-time dashboards to track progress across the various layers of healthcare operations. These dashboards can monitor everything from patient flow and staff allocation to energy consumption and waste production, providing immediate insights that help administrators make data-driven decisions. Developing tailored metrics for each layer—clinical, operational, accessibility and sustainability—is equally critical, ensuring that every domain’s unique impact is accurately measured and improved upon. For instance, while clinical metrics might focus on diagnostic accuracy or patient recovery times, sustainability metrics could capture greenhouse gas reductions from AI-enabled energy management systems. Such systems, when integrated with remote monitoring technologies, can not only optimise hospital lighting, heating and cooling but also predict maintenance needs, ultimately extending the lifespan of critical equipment. Finally, fostering partnerships among governments, healthcare providers, technology firms and community organisations can pave the way for ambitious initiatives, such as building carbon-neutral healthcare facilities and distributing resources equitably to underserved areas. By uniting diverse stakeholders, these collaborations accelerate the pace of innovation, broaden access to life-saving care and ensure that AI’s benefits reach every corner of the health ecosystem—leading to a greener, more inclusive future.
The potential is enormous: healthcare systems that reduce emissions, enhance access to care for underserved populations and build resilience against future crises. However, realising this vision requires sustained investment in workforce training, ethical AI development and robust frameworks to measure and adapt progress across all dimensions of healthcare.
Conclusion
To fully realise the transformative potential of AI in healthcare, its impact must be measured across all layers of the system—enhancing clinical outcomes, streamlining operations, breaking down barriers to accessibility and advancing sustainability. AI-enabled dashboards, tailored metrics, and partnerships can help bridge the gap between innovation and tangible, system-wide benefits. Achieving this vision demands novel forms of collaboration among healthcare providers and various other stakeholders to align their strategies and scale sustainable solutions. By doing so, AI will not only redefine patient care but also catalyse a greener, more equitable future for healthcare systems worldwide.
Conflict of Interest
None
References:
Bratan T, Heyen NB, Hüsing B. et al. (2024) Hypotheses on environmental impacts of AI use in healthcare. The Journal of Climate Change and Health, 16: 100299 (accessed on 31 January 2025). Available from doi.org/10.1016/j.joclim.2024.100299
Chustecki M (2024) Benefits and risks of AI in health care: Narrative review. Interactive Journal of Medical Research, 13(1): e53616 (accessed on 31 January 2025). Available from doi.org/10.2196/53616
Philips Editorial Team (2022) 10 real-world examples of AI in healthcare. Philips, 24 November (accessed on 29 January 2025). Available from philips.com/a-w/about/news/archive/features/2022/20221124-10-real-world-examples-of-ai-in-healthcare.html
Sahni N, Stein G, Zemmel R et al. (2023) The potential impact of artificial intelligence on healthcare spending. Cambridge, MA, USA: National Bureau of Economic Research: w30857.
Tenovi (2024). How is AI used in remote patient monitoring? Tenovi, 23 August (accessed on 29 January 2025). Available from tenovi.com/ai-in-remote-patient-monitoring/
Raman R, Pattnaik D, Lathabai HH et al. (2024) Green and sustainable AI research: an integrated thematic and topic modeling analysis. Journal of Big Data, 11(1): 55 (accessed on 31 January 2025). Available from doi.org/10.1186/s40537-024-00920-x
Ueda D, Walston SL, Fujita S et al. (2024) Climate change and artificial intelligence in healthcare: Review and recommendations towards a sustainable future. Diagnostic and interventional imaging, 105(11): 453–459 (accessed on 31 January 2025). Available from doi.org/10.1016/j.diii.2024.06.002








