Two articles published online by JAMA Dermatology address the use of mobile technology applications in skin cancer prevention and skin care. The first reports on the results of two studies of the Solar Cell app for promoting sun safety, while the second discusses how teledermatology can assist patients and physicians in the short-term monitoring of atypical skin moles.
Solar Cell Smartphone App
The Solar Cell smartphone app was developed by Golden, Colorado-based Klein Buendel, in research supported by the National Cancer Institute. The app offers real-time advice for sun protection, based on UV forecasts and user information, to improve safe behaviours such as seeking shade and wearing sunscreen.
“The Solar Cell mobile app seemed to promote sun protection practices, especially when it was used. Specifically, it increased use of shade. Shade can substantially reduce exposure to solar UV radiation (UV-R), but it needs to be available for it to be used,” wrote David B. Buller, PhD, and his co-authors.
Buller conducted a randomised clinical trial on a mobile phone app that provided sun-protection advice based on UV Index forecasts in combination with users’ personal information. The app also employed alerts which reminded users to apply or reapply sunscreen.Of 604 enrolled participants, 232 of the 305 individuals in the treatment group downloaded the app. However, just 125 individuals (41 percent) actually used it. Compared with the general US population, the study’s participants were young, highly educated and affluent, and there were fewer Hispanic whites.
The participants in the treatment group were more likely than control participants to spend time in the shade (41 percent vs. 33.7 percent of days staying in the shade) but they were not more likely to use sunscreen than those in the control group (28.6 percent vs. 34.5 percent of days). Treatment participants spent 39.4 percent of days using combined sun protection habits (including shade, sunscreen and protective clothing) versus 33.8 percent of days for the control group.
Volunteer Trial: App Is Effective — When It Is Used
A second randomised study involving the Solar Cell app collected data from 202 volunteers, and was also associated with greater sun protection behaviours. This time, 74 of the 96 participants who were assigned to use the app actually did so. At the seven-week follow-up, treatment participants were more likely than control participants to wear wide-brimmed hats (23.8 percent vs. 17.4 percent). Female participants reported higher combined use of the sun protection strategies (46.4 percent vs. 43.3 percent). Men and older participants, meanwhile, were less likely to use sunscreen (32.7 percent vs. 35.5 percent) and hats (15.6 percent vs. 17.9 percent).
Buller et al. concluded that the app is effective, but its use must be encouraged. “Strategies to increase the use of the mobile application are needed if the application is to be deployed effectively to the general population,” they wrote.
Mobile Teledermoscopy For Mole Monitoring
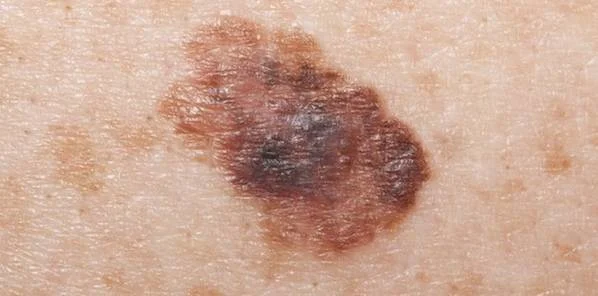
Another study published in JAMA Dermatology discusses the feasibility of patients using mobile devices to photograph skin anomalies as a short-term method of monitoring atypical moles. Atypical moles are routinely monitored in the short-term for changes in appearance, with the standard length of observation being 2.5 to 4.5 months. During that time, approximately 19 percent of moles will show changes, with 11 to 18 percent of those going on to be diagnosed as malignant.
Teledermoscopy, in which patients use a mobile dermascope attached to a smartphone to take pictures of their monitored moles and submit them electronically to a dermatologist, is an ideal way for patients and doctors to follow any changes which might require follow-up care.
Xinyuan Wu, BA, of the Memorial Sloan Kettering Cancer Center, New York, and other authors examined teledermoscopy for its effectiveness, feasibility and patient receptivity. The researchers recruited 34 patients under the care of two dermatologists; 29 patients completed follow-up. Dermoscope images were collected by patients and sent to the dermatologist at baseline and follow-up three to four months later.
There was near-complete agreement between the diagnoses generated by teledermoscopy and those which came from traditional office visits, the study found. In terms of patients' receptivity to teledermatology for the short-term monitoring of moles, they were agreeable to the method.
“Our results showed that the use of teledermoscopy in short-term monitoring is highly feasible, has strong diagnostic concordance with conventional clinical visits and is well received by patients,” the authors wrote.
The Role of the Teledermatologist
An accompanying editorial by Monika Janda, PhD, of Queensland University of Technology in Brisbane, Australia, and coauthors commented on the Wu et al. study. “The study by Wu and colleagues in this issue adds significantly to the discussion on whether regular follow-up visits with clinicians could be replaced by patient self-monitoring with remote feedback by a teledermatologist. … In conclusion, the findings from Wu and colleagues provide further support for the feasibility of consumer-driven mobile teledermoscopy.”
Souce: JAMA Dermatology
Image Credit: Google Images
Latest Articles
telemedicine, skin cancer, mobile apps, dermatology
Two articles published online by JAMA Dermatology address the use of mobile technology applications in skin cancer prevention and skin care. The first repo...