HealthManagement, Volume 5 / Issue 3-4 / 2010
Author
Maurice Mars
Professor and Head of Tele-Health,
Nelson R Mandela School of Medicine,
University of KwaZulu-Natal, South Africa“E-Health has
the potential to be of great benefit to Africa if it can be planned and
implemented in an appropriate and sustainable manner.” Statements like this are
heard at many conferences and meetings around the world, but what is the
reality on the ground in sub-Saharan Africa?
One only has to look at the substantial amounts of money already spent on attempts to get electronic health systems going in the developed world and the low uptake of telemedicine internationally to ask why there is the expectation that things will be different in poverty stricken countries in Africa. Some tough questions need to be answered before embarking on e-Health in Africa. For example, is expenditure on IT for e-Health morally justifiable in the absence of hard economic data on the benefits of e-Health in the developing world?
The Dilemma of the African Politician – a
Scenario
Put yourself in the position of a minister of health of a hypothetical sub-Saharan African country. Like most countries in Africa, your country is very poor. It is five years since the civil war that left much of the country’s infrastructure damaged or destroyed. Many health professionals fled during the conflict and have not returned. The medical school lacks specialist staff and modern diagnostic equipment. Malaria, tuberculosis and HIV/AIDS are rife. Adding to the problem, refugees from one of your neighbours are fleeing the civil war in their country for the sanctuary of your now stable nation and adding to the burden of disease.
Donor agencies and international foundations are expressing confidence in the vision of the Government by supporting many projects in health, based on individual diseases. The international cell phone service providers see a new market opening up and are investing in infrastructure. You have a health policy that offers promise but which will be dependent on donor funding for some years to come. Your colleagues in Government have just finished the national ICT strategy and in general the country appears to be doing well. There is however the nagging issue of the health related Millennium Development Goals, reduction of maternal mortality, infant mortality and infectious diseases. Unfortunately even after 5 years of peace, you have not made any meaningful inroads on any of these. Indeed peace has lead to the reproductive rate increasing with associated increases in maternal and infant mortality.
At a recent regional meeting of Health Ministers, colleagues whose countries are members of the British Commonwealth, were talking about the Commonwealth Health Ministers’ Meeting focussed on e-Health, subsequent regional meetings on e-Health and their plans to work on e-Health strategies, something which you do not have. You are surprised because e-Health is not part of the current African Union Health Ministers’ Plan which you signed recently and you can’t recall e-Health being part of the NEPAD Health Strategy. You are reminded that a few years ago, towards the end of the unrest, the World Health Organisation called on member nations to develop an e-Health strategy and to ensure that there was an adequate telecommunications infrastructure.
But where do you get started? Several of the donors and NGO’s have set up electronic systems to monitor their Aids and TB related projects and you had a deputation of District Health Managers in your office just the other day complaining that staff is unhappy about having to enter patients data and test results in four different electronic systems. The time has come to look at e-Health and make informed decisions.
E-Health – the Promise?
Which aspect of e-health offers Africa the most promise? Is it a functional electronic district health system, an electronic patient card, a health portal, a health information system, an electronic patient record, an electronic medical record, store and forward telemedicine, synchronous telemedicine, robotic surgery, home monitoring, home care, tele-education or surveillance. All are e-Health needs that have been identified in the developed world.
The e-Health requirements and aspirations of countries vary, and this is exemplified in the e-Health road maps of the European Union member nations. Likewise, it is expected that there will be variations in the needs of African countries. These may differ markedly from those of developed nations because health issues in the developed world and the developing world are different. The developed world is grappling with the problem of increasing healthcare costs and keeping ageing populations out of hospitals. The developing world faces a disproportionately high burden of disease, growing populations, poverty, and shortages of healthcare workers.
The term ‘developing world’ is unfortunate as it includes both emerging giants like China, Brazil and India and also the poorest of the poor countries, home to the ‘bottom billion’ people. e-Health solutions for the emerging nations may well be different to those of the non-developing nations. It is the people of the bottom billion who are most in need of the potential benefits offered by e-Health and who are least likely to derive these benefits. All of sub-Saharan Africa’s countries are categorised as developing and many countries are part of the unfortunate bottom billion family.
Africa’s Health Problems
The World Health Report of 2006 succinctly stated the health problems facing Africa and sub-Saharan Africa in particular, “…Africa has 24 percent of the burden (of disease), but only 3 percent of the health workers commanding less than 1 percent of world health expenditure” and that the “exodus of skilled professionals in the midst of so much unmet health needs places Africa at the epicentre of the global health workforce crisis.” In 2005, the World Health Assembly saw e-Health as a possible way of addressing some of these problems and resolution WHA58.28 called on member nations to develop long term e-Health strategic plans, provide necessary telecommunications infrastructure for e-Health and establish national centres of excellence. The WHO Global Observatory for e-Health report of 2006 suggested that, “It may be time to put forth the concept of ‘e-Health for all by 2015’ as an addendum to the Millennium Development Goals.” It also noted the need for an international knowledge exchange network to share practical experiences on the application and impact of e-Health initiatives, the use of e-learning programmes and the inclusion of ehealth courses within university curricula.
While the World Health Report identifies the problems of disease burden, the health workforce and budget in Africa, it does not mention technological and other obstacles to the implementation and uptake of e-Health solutions in Africa or the effect of population growth. These need to be examined in more detail to better understand the potential use of e-Health and the obstacles to its sustainable use.
Poverty
All of sub-Saharan Africa’s Countries are poor, the percentage that governments spend on health is relatively low and the resultant budgets are very small. The median government budget for health is US$ 14.00 per capita per annum which when corrected for purchasing power parity equates to US$ 32.00 per capita per annum. With budgets like these, salaries in Government hospitals and clinics are low, modern diagnostic equipment is scarce and drugs are in short supply.
What then is available for e-Health? A working figure is that Governments spend about 2 – 2.5% of their health budgets on healthcare IT and communications technologies. Based on the median spend in sub-Saharan Africa this is US$ 0.28 – 0.35 per capita per annum which, after taking purchasing parity into account is US$ 0.64 – 0.80 per capita per annum.
What can be done with a budget at this level? Clearly expectations of what e-Health can offer have to be tempered by the reality of the available budget, careful reflection on the opportunity cost of using this money for e-Health and the recurring costs of ownership? What hard data are there to support the change to e-Health in the developing world: very little. What of the cost of change management which can be a 40 – 60 percent overhead on the infrastructure cost? The ultimate question becomes, what e-Health activity will benefit the most people?
Population Growth
While many developed countries face stagnant or negative population growth, Africa continues to grow rapidly. The United Nations Population Division forecasts the population of Africa to increase by over a billion people by 2050. Who is going to treat this growing and by inference, young population? Is there capacity to offer adequate care to the mothers and their children while at the same time addressing infectious diseases?
Human Resource Issues
The shortage of health professionals is already dire. Twentyeight countries have ten or fewer doctors per 100,000 people and 35 countries have fewer than 20 doctors per 100,000 people. Germany, Italy Norway and the United Kingdom there are 340, 370, 380 and 230 doctors per 100,000 people respectively. While there are moves to increase the production of doctors in Africa, it is often forgotten that when there is a shortage of doctors there is also a shortage of doctors to teach doctors. It is not uncommon for medical schools to have no specialists in some disciplines and in some countries there are no specialists in certain fields. Who then teaches these specialties at undergraduate and specialist trainee level? In South Africa with 80 doctors per 100, 000 people, approximately a third of all academic posts at medical schools are said to be vacant. It is also forgotten that in order to produce more doctors, the school system has to be able to produce enough people with sufficient basic education and of sufficient calibre to enter medical schools.
Some solution has to be found to build the capacity to develop capacity in sub-Saharan Africa.
Effects
In some countries maternal mortality and infant mortality rates have increased as already overstretched health services are unable to cope. Little progress has been made in reducing HIV and tuberculosis while inroads have been made in combating malaria through recent campaigns to provide chemically treated mosquito nets. It is unlikely that any African country will achieve its health related Millennium Development Goals and for the foreseeable future there will be large numbers of children being born and mothers and children dying because of inadequate human resources.
Telemedicine as a Solution?
Telemedicine offers an obvious solution to some of the clinical problems associated with a shortage of doctors. Information travelling through the Internet knows no borders. Rural patients can be treated at a distance in their own country and patients can receive specialist services from doctors in other countries. Why then is telemedicine, both store and forward and synchronous, not being widely used in sub-Saharan Africa and more particularly why are the free international humanitarian services not used?
An example is the Swinfen Charitable Trust which offers free store and forward telemedicine services to 153 hospitals and clinics in 50 countries around the world. Hospitals and clinics in 13 African countries have used the service. Data from 2007 show that only 7 of 206 cases referred that year, were from 6 African countries and of the 6 doctors who referred cases, only one was a local national.
Why is use of a free service low? Possible reasons for this are: cost, lack of infrastructure or access to infrastructure, ignorance, workload, lack of training, issues of remuneration and legislative and policy barriers.
Workload
Workload is seldom mentioned as a barrier to the implementation of telemedicine but it is when there is shortage of doctors. Telemedicine adds steps to the normal workflow of both the doctors and nurses at the send and receive sites. It is not uncommon to be told by doctors that, “Telemedicine is a nice idea but I don’t have time to do it. I’m too busy.”
Connectivity
Connectivity is a pre-requisite for telemedicine. Africa missed the benefits of the dotcom boom when widespread deployment of cable occurred in the developed world. It not only missed the dotcom boom, it missed the plain old telephone generation. Fixed line telephone penetration in Africa is only 1.4 percent. Most Internet service providers use fixed phone lines for Internet delivery. It is not surprising therefore that internet penetration in sub-Saharan Africa is low, in the region of 4.5 percent compared to Europe 52 percent and North America 74 percent.
In the developed world, fixed broadband is replacing dial-up access. Broadband connectivity is essential for synchronous telemedicine services. It has been identified as a prerequisite for e-Health services in Europe, and the United States is finalising a national broadband policy.
The situation in Africa is somewhat different with fixed broadband penetration at less than 0.1%. Mobile telephone broadband access is in the region of 0.9% but its use is limited by the high cost of mobile phone access. Lack of broadband remains an obstacle to synchronous telemedicine in the Africa.
In part this is due to the low fixed telephone line penetration which limits the use of asymmetric digital subscriber lines (ADSL).
Per capita bandwidth is very low. In 2008, Africa had 12 Gbps of international bandwidth which is less than a third of that of India. New undersea fibre optic cables are coming online on the East coast of Africa and new cables are planned for the West coast. These will improve per capita bandwidth and are expected to reduce costs. Currently there is a large disparity in bandwidth per capita in sub-Saharan Africa with landlocked countries still dependent on expensive satellite access.
Communication Costs
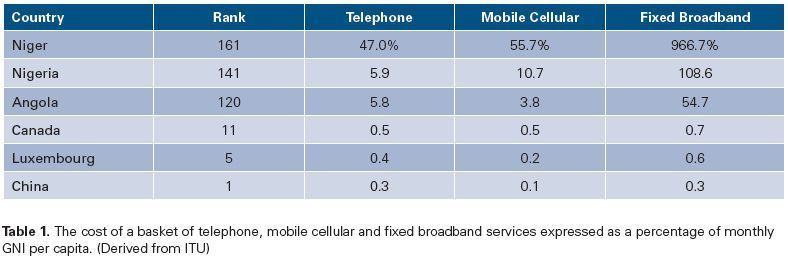
The ITU has developed an ICT Price Basket and ranks 161 countries on the basis of a set of standardised fixed phone line telephony, mobile cellular, and broadband services and describes these in terms of relative cost, expressed as a percentage of the average monthly gross national income (GNI) per capita. Nineteen of the most expensive services are in countries in sub-Saharan Africa. Some examples of costs of sub-Saharan African and developed nations are shown in Table 1.
Broadband costs vary greatly. In the Central African Republic, Ethiopia and Malawi the monthly cost of the ITU bundle for fixed broadband services, is 39, 21 and 20 times the average per capita GNI per month. Broadband access exceeds the monthly GNI in 22 African countries. This is due in part to poor fixed phone line penetration and the resultant need to use fixed leased lines like WDSL and SDSL for broadband access rather than ADSL through a fixed phone line. Although costs continue to fall, they remain too high. This is a barrier to further uptake of healthcare IT in sub-Saharan Africa and may further increase the digital divide. Broadband connectivity costs are therefore a major obstacle to e-Health, especially synchronous telemedicine.
Mobile Telephony
It is frequently said that Africa has jumped the fixed phone line generation and has moved directly to mobile phones. Large annual growth in mobile phone penetration is reported annually. It must be remembered that this is off a low initial base.
Mobile phone penetration is now estimated to be in the region of 32 percent. Mobile phone penetration has increased access to rural communities with over 40 percent of the rural population covered by a cell phone signal in 2006. Of these areas only 3 percent have fixed telephone connections.
Health Informatics
Telemedicine is seen as a partial solution to the clinical needs of Africa, but what of district health information systems, hospital information systems, electronic medical records, electronic patient records and surveillance? Most sub-Saharan African countries are in the fortunate situation of having few if any electronic health information legacy systems.
They are, however, faced with another problem, that of vertical programmes and data duplication. Many international donors support disease specific programmes and require patient data capture and programme reporting in specific formats. It is not uncommon for the same patient’s information to be entered several times in different systems in the same hospital or health system if for example they have had malaria, are HIV positive, on antiretroviral therapy and have tuberculosis. It is seldom that data can be moved freely from one system to another.
This vertical approach is a problem for Governments which, because of their dependence on donor funding to benefit their people, do not have enough power or influence to force donors to adopt a uniform system of data capture and reporting system in their country. This also leads to situations in which disease specific health information systems are written in proprietary software without any attempt to standardise data formats so that data can be shared between systems.
The use of free and open source software is now seen as the logical approach to the development of health information systems in sub-Saharan Africa. The Health Information System Programme (HISP) and the Open Medical Record System (Open MRS) are examples. Open source solutions are however a double edged sword; the end user is not committed to an initial purchase cost and subsequent upgrades but the open source developers are not beholden to an employer to provide support or software fixes.
There are other problems. Paper based district health information systems do not function well in sub-Saharan Africa. Data capture is erratic and often incomplete and time to analysis long. In most African countries there is not a culture of data acquisition, analysis and interpretation. The problem is exacerbated when data are captured electronically as people do not see the need to change the way they do things as in many instance they do not see the benefit of change. Internet penetration in Africa is low and computer literacy is also low. As a result, computer training is often required before electronic data capture can begin and training may have to be repeated as staff change.
>to be continued in Issue 5.





