Health Information Technologies (HIT) have the potential to enhance healthcare outcomes and patient safety, but risks associated with bad design or implementation persist. Despite their promise, HIT and Health Information Systems (HIS) can introduce errors due to various factors such as software glitches, user errors, and system flaws. This underscores the importance of ongoing evaluation of HIT safety in diverse healthcare settings, considering factors like software advancements, contextual use, and evolving medical practices. Methodological challenges in researching HIS safety, including defining errors, identifying causes, and implementing prevention strategies, are also to be discussed. A recent paper published in the Health Informatics Journal highlights the need for process improvement in ensuring quality healthcare services. It also points out the scarcity of published reports on the impact of HIS on workflows and the need for studies focusing on process-related medical errors. Addressing these challenges requires integrating technical and organisational components and selecting appropriate improvement methods aligned with organisational goals.
Healthcare Quality Improvement: The HOPT-fit Framework and Lean Principles
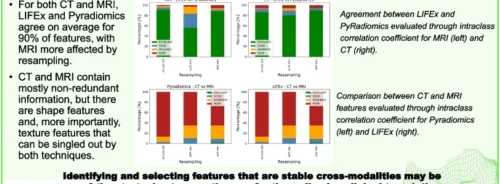
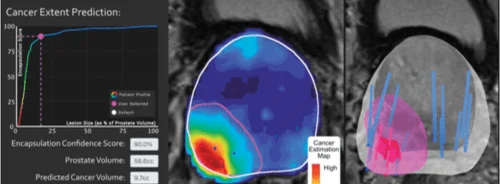
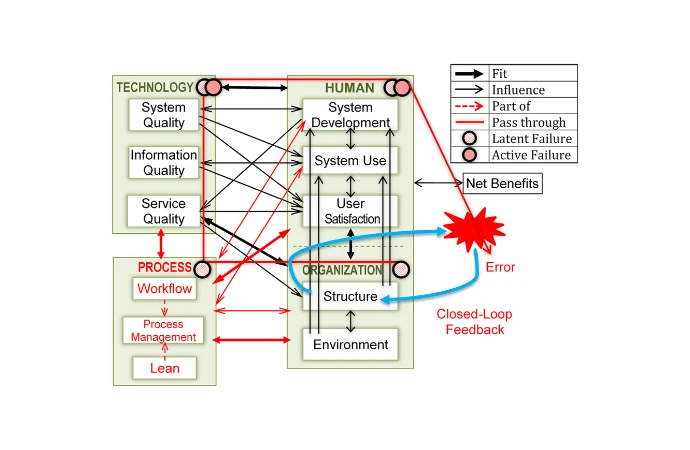
To bridge these gaps, the text proposes a process-oriented approach, integrating business process management (BPM) and Lean methods. This innovative approach holds the potential to revolutionize healthcare quality improvement, introducing the HOPT-fit framework. This framework, with its comprehensive approach, expands upon existing models by incorporating process factors and emphasizing safety and quality aspects. It aims to evaluate HIS-related errors comprehensively and proposes Lean methods for improving medication processes, offering a promising path towards enhanced patient safety and healthcare quality. The paper introduces a new evaluation framework, assesses HIS-related error management, and applies Lean principles to enhance patient safety. It presents detailed findings from case studies, validating the framework's applicability and offering insights into socio-technical, error management, and quality improvement perspectives.
Addressing Latent Errors from Design to Implementation
The authors provide an overview of errors related to Health Information Systems (HIS), distinguishing between active failures attributed to human actions and latent conditions stemming from systemic factors. Active failures encompass slips and mistakes, while latent conditions represent underlying system weaknesses. Unlike unpredictable active failures, latent conditions can be identified and mitigated proactively. HIS-related errors occur throughout the system development life cycle (SDLC), with a higher incidence post-implementation. Early prevention measures are crucial. Emphasis is placed on addressing errors during technology development to avoid widespread negative consequences. Various error models and studies highlight the importance of considering latent errors and socio-technical challenges in risk management. Understanding HIS risks during the design stage is crucial to prevent latent failures.
Holistic Approach to Health Information Systems Evaluation and Management
According to the socio-technical aspects of Health Information Systems (HIS), medical errors (MEs) stem not only from human or computer errors but also from poor interactions among technology, processes, organisations, and people. Understanding these interactions is crucial for optimising HIS potential on patient safety. Three trends in ME evaluation and management are identified: focusing on end-to-end workflow, process management, and the system development life cycle (SDLC). ME risk can be identified and mitigated across SDLC phases and process steps through a multidisciplinary and multifactorial systems approach. This approach involves interdisciplinary safety teams, including personnel from various organisational levels, with ideally an integration across processes, settings, and the overall organisation.
Navigating Challenges in Health Information Systems Development
Each system development phase of Health Information Systems (HIS) can be associated with challenges:
- Planning: Unclear purposes in system planning can lead to subsequent phase issues. Unrealistic planning, inadequate user involvement, and unclear requirements can be costly.
- Design: Design flaws such as poor function aids and complex interfaces can lead to errors. Simplifying HIS design may be more effective than extensive training. Incident reports and usability testing inform design improvements.
- Implementation: Chaotic implementation strategies, such as insufficient training, can disrupt workflows. Implementation must consider organisational needs, customisation, integration, education, and testing.
- Testing: Usability inspection and testing identify usability and system problems, ensuring smooth implementation. Correcting errors at this stage can save costs in the long term.
- Use: Proper HIS use requires alignment with workflows to ensure safety and effectiveness. Risks include alert fatigue, automation bias, and misuse of functions.
- Evaluation and optimisation: Early and continuous testing and error mitigation can reduce risks. Collaboration with vendors is crucial for optimising HIT for quality and safety.
Overall, a systematic approach to system development, from planning to optimisation, is essential for effective HIS implementation and usage.
Maximising Benefits and Minimising Errors in Health Information Systems Management
Authors offered an inventory of tangible benefits derived from efforts to enhance Health Information Systems (HIS) and manage HIS-related errors:
- Efficiency and Error Reduction: Despite an increase in work duration due to additional tasks such as data entry, the implementation of templates and innovative educational approaches has led to improved work efficiency and a reduction in errors. These strategies have streamlined processes and standardised procedures, making it easier for users to input instructions and descriptions.
- Patient Safety Unit Improvements: The establishment of a patient safety unit has yielded multiple improvements, particularly in reducing medication errors and enhancing staff participation in error reporting and problem-solving. This unit's multidisciplinary efforts have contributed to the development and implementation of effective risk management strategies.
- System Enhancements: According to system theory, the process of system development often uncovers problems or "reverse salient," which, when addressed, lead to system improvement and innovation. Identifying these issues contributes to a cycle of continuous improvement, where ongoing evaluation and problem-solving drive enhancements in HIS effectiveness and efficiency.
- Effective Error Management: Various strategies, including Kaizen (continuous improvement), strong management, effective communication, and incident reporting, have facilitated effective error management within HIS. These strategies focus on identifying, mitigating, and learning from errors to build resilient systems and promote a culture of safety.
- Medication Error Reduction: Through improved system design, the addition of alerts, and the standardisation of procedures, significant reductions in medication error rates have been achieved. These measures aim to simplify processes, enhance user interfaces, and provide timely reminders and warnings to prevent errors.
- Simulation-based Training: Simulation-based training has emerged as an effective method for minimising errors by allowing users to practice realistic scenarios in a safe environment. This approach not only identifies potential workarounds and system weaknesses but also improves user proficiency and system usability.
- Communication and Education: Efforts to enhance communication, education, and training have increased staff awareness, understanding, and participation in error reporting and prevention. By providing comprehensive training and fostering a culture of open communication, organisations can empower staff to identify and address errors effectively.
- Evaluation and Optimisation: Early and continuous testing, coupled with organisational risk management strategies, have played a crucial role in reducing risks and optimising safety processes within HIS. These data-driven approaches enable organisations to identify potential risks, monitor system performance, and implement targeted interventions to prevent errors.
- Holistic Approach: The proposed evaluation framework, HOPT-fit, offers a structured and holistic approach to identifying potential HIS-related errors and their consequences. By considering various dimensions and measures, this framework enables organisations to systematically evaluate and address errors throughout the entire system development life cycle.
- Lean Principles and Lean IT: Leveraging Lean principles and Lean IT methods has enabled organisations to optimise workflows, improve system design, and cultivate a culture of safety. Organisations can enhance system efficiency and effectiveness while minimising errors by eliminating waste, standardising processes, and promoting continuous improvement.
- Continuous Improvement: The study underscores the importance of ongoing evaluation and continuous improvement throughout the SDLC and overall process stages. Organisations can optimise system potentials and enhance patient safety by continually identifying and addressing emerging HIS-related errors.
Various strategies and approaches, ranging from system enhancements to communication and education efforts, contribute to improving HIS effectiveness, reducing errors, and ultimately enhancing patient safety within healthcare systems.
Source & Image Credit: Health Informatics Journal