Breast cancer remains the most frequently diagnosed cancer among women worldwide. While mammography has been the cornerstone of breast cancer screening, its one-size-fits-all approach has notable limitations, particularly in women with dense breast tissue and those at higher risk. In recent years, the focus has shifted toward more personalised screening strategies, incorporating a variety of imaging modalities such as MRI, ultrasound, and artificial intelligence. The adoption of a risk-stratified approach to breast cancer screening has shown potential to address the shortcomings of traditional screening, enhancing early detection and improving outcomes for high-risk populations.
The Limitations of Traditional Mammography
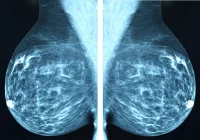
Mammography has long been regarded as the gold standard for breast cancer screening due to its broad availability and capacity for early detection. Regular mammograms have been shown to reduce breast cancer mortality by at least 20% over the last three decades. Despite this success, mammography's efficacy varies significantly depending on factors such as breast density. Dense breast tissue, found in approximately 40-50% of women, can obscure cancerous lesions on mammograms, leading to underdiagnosis. In women with dense breasts, the sensitivity of mammography drops to as low as 62%, compared to 86-89% in women with largely fatty breasts. This underlines the need for additional screening methods tailored to individual risk profiles.
Digital breast tomosynthesis (DBT) has emerged as a promising alternative to mammography. DBT offers pseudo-3D imaging, reducing tissue superimposition and increasing cancer detection rates by up to four additional cancers per 1,000 screens. However, DBT’s benefits are still limited in women with extremely dense breasts, and concerns about overdiagnosis persist. Mammography also has drawbacks in high-risk populations, where it often fails to detect smaller, more aggressive cancers at an early stage. These limitations highlight the need for more personalised and supplemental screening methods, particularly for high-risk women and those with dense breasts.
Advancements in Personalised Screening
The Role of MRI and Ultrasound Breast MRI has proven to be the most sensitive imaging modality for detecting breast cancer, particularly in high-risk populations. Its ability to detect neovascularity allows it to identify aggressive tumour subtypes, making it an essential tool for women with a high lifetime risk of breast cancer. MRI is not affected by breast density, and studies such as the Dutch DENSE trial have demonstrated its cost-effectiveness in reducing mortality among women with extremely dense breasts. For high-risk women, screening with breast MRI is recommended annually starting at age 25, with mammography supplementing MRI from age 35-40.
Ultrasound is another valuable supplemental imaging tool, especially for women with dense breasts who cannot undergo MRI. Automated breast ultrasound systems have been introduced to address some of the limitations of handheld ultrasound, such as operator dependency and long examination times. Supplemental ultrasound has been shown to increase the detection of small, invasive, node-negative cancers often missed by mammography. However, ultrasound’s high recall and biopsy rates raise concerns about cost-effectiveness and the potential for unnecessary procedures. While it may benefit specific populations, the balance between its advantages and disadvantages must be carefully considered when integrating it into routine screening protocols.
Addressing the Downsides of Breast Cancer Screening
Despite the undeniable benefits of breast cancer screening, certain downsides, such as underdiagnosis, false positives, and overdiagnosis, need to be addressed to optimise outcomes. Underdiagnosis occurs when a clinically relevant cancer is present but missed during screening. This is particularly prevalent in women with dense breasts, where up to 30% of cancers detected through mammography have already spread to the lymph nodes or grown larger than 2 cm. Retrospective evaluations often show that a significant percentage of these cancers could have been detected earlier using more sensitive imaging techniques like MRI or DBT.
False positives are another drawback of breast cancer screening, with up to 12% of women undergoing mammography being recalled for additional workups. These false positives can lead to unnecessary biopsies and short-term follow-ups, contributing to patient anxiety and healthcare costs. Double reading, where two radiologists independently review mammograms, has been shown to reduce recall rates without compromising cancer detection rates. However, the experience of a false positive can still deter women from participating in future screening rounds, emphasising the need for more precise imaging modalities that minimise false alarms.
Overdiagnosis refers to detecting cancers that would never have become clinically significant if left untreated. This can lead to overtreatment, unnecessary surgery, and even patient morbidity. Slower-growing cancers, often detected via mammography, are more likely to be overdiagnosed. Reducing overdiagnosis requires identifying “low-risk” cancers and carefully monitoring them without immediate intervention. Active monitoring is currently being explored in clinical trials as an alternative to conventional treatment for low-risk ductal carcinoma in situ (DCIS), to minimise overtreatment without compromising outcomes.
Conclusion
As breast cancer screening continues to evolve, moving toward a personalised approach is essential to overcoming the limitations of traditional methods like mammography. Incorporating advanced imaging modalities such as MRI, DBT, and ultrasound can improve detection rates, particularly in high-risk populations and women with dense breasts. Using artificial intelligence to enhance risk stratification and reduce interval cancers further supports this transition. While challenges such as false positives and overdiagnosis must still be addressed, personalised screening can improve early detection, reduce unnecessary interventions, and ultimately save more lives. The future of breast cancer screening lies in tailoring protocols to individual risk profiles, ensuring that every woman receives the most effective care based on her unique needs.
Source Credit: European Radiology
Image Credit: iStock